Chapter 191 Multiple Sclerosis
 General Considerations
General Considerations
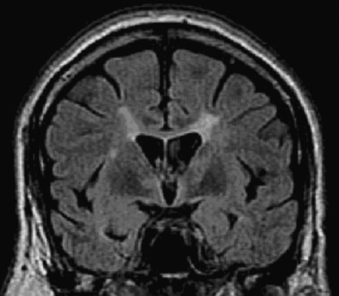
MS is the most common disabling neurologic disease of young and middle-aged adults in North America and Europe.1 Physicians have recognized its pathologic and clinical features since the mid–nineteenth century. MS pathology consists of multifocal areas of demyelination, referred to as plaques, in the brain, spinal cord, and optic nerves. In these areas there is destruction of the myelin sheath around axons with relative sparing of axons, although axonal damage also occurs in MS. Inflammatory cells composed of macrophages and lymphocytes are present when there is active demyelination within MS plaques, indicating that MS is an inflammatory disease. Magnetic resonance imaging (MRI) provides a means of visualizing MS lesions within the brain and spinal cord (Figure 191-1). Clinically, MS can cause various neurologic problems, depending on the location and severity of MS plaques (Table 191-1). In about 85% of cases, MS starts with a relapsing-remitting course.2 Patients experience relapses or attacks of MS during which they develop a new neurologic problem, return of an old problem that had resolved, or worsening of preexisting symptoms. Relapses develop over a few days or weeks, followed by a period of improvement and stability. In between relapses, patients are clinically stable, although they may have residual permanent neurologic symptoms from previous relapses. However, relapses that cause symptoms represent only the “tip of the iceberg” of disease activity at this stage of the illness. Serial MRI studies in MS patients have disclosed that new, asymptomatic MS lesions appear within the brain 5 to 10 times more commonly than symptomatic lesions, and these cause permanent damage that contributes to the overall MS disease burden.3
TABLE 191-1 Symptoms of Multiple Sclerosis and Their Neurologic Causes
| SYMPTOMS | CAUSES |
|---|---|
| Weakness and numbness and tingling in legs and arms; stiffness in legs | Spinal cord lesions |
| Urinary urgency, retention, incontinence and recurrent infections | Spinal cord lesions |
| Constipation | Spinal cord lesions; diet |
| Sexual dysfunction | Spinal cord lesions |
| Blurred vision and blindness | Optic nerve lesions |
| Double vision | Brainstem lesions |
| Imbalance | Spinal cord and cerebellar lesions |
| Tremor of arms | Cerebellar lesions |
| Impaired memory and concentration | Cerebral lesions |
| Fatigue | Effects of inflammatory cytokines on neuronal function; nerve fiber fatigability resulting from demyelination |
| Heat sensitivity | Sensitivity of demyelinations to elevations in body temperature |
| Depression and other mood changes | Cerebral lesions and changes/disorders in neurotransmitters |
About 50% of patients with relapsing-remitting MS (RRMS) enter a progressive phase of the disease 10 to 15 years after onset. Steady worsening characterizes this phase of the illness, called secondary progressive MS. Patients with secondary progressive MS may or may not continue to have relapses. About 15% of MS patients have progressive worsening from the onset of their illness, a form of MS referred to as primary progressive MS. Although MS is rarely fatal, it is often disabling, with about one third of patients losing the ability to walk 15 to 20 years after onset. In benign forms of MS, comprising up to 15% of patients, patients never develop any permanent disability from MS. Most patients, however, develop varying degrees of permanent neurologic disability.
Epidemiology
MS affects about 1 of 1000 persons in the United States, Canada, and northern Europe. MS typically begins between the ages of 20 and 55 but may occur at any age. Women are more commonly affected than men, with about 60% of cases being female. A strong racial influence on the risk of developing MS exists: it is most common among whites, particularly those of northern European descent.4,5 Typical MS is rare among Asians and black Africans but is relatively common among black Americans. The racial predilection of MS is one piece of evidence indicating the strong influence of genes on the risk of developing MS. In addition to racial influences, there is also an interesting geographic distribution of the disease. Areas with the highest prevalence are located in higher latitudes, in both the northern and southern hemispheres.6,7 These high-risk areas include the northern United States, Canada, Great Britain, Scandinavia, northern Europe, New Zealand, and Tasmania.8,9
Pathogenesis
All of the signs and symptoms of MS relate to damage to the brain, spinal cord, and optic nerves.
Macrophages can cause damage by releasing soluble inflammatory mediators such as cytokines and free radicals or by actively stripping myelin from the axon sheath. Activated T cells can also release proinflammatory cytokines, which can contribute to tissue damage. Finally, antimyelin antibodies can damage myelin either by initiating complement-mediated demyelination or assisting the phagocytosis of myelin by macrophages. The disease process is “turned off” by apoptosis of the disease-initiating T cells and by the recruitment of regulatory T cells into the CNS. This model of the acute MS lesion is consistent with the most prevalent theory about the MS, namely that it is an immune-mediated disease (Figure 191-2).
Risk Factors
Genes
Substantial evidence indicates that genetic background influences the risk of developing MS.10,11 Race is a strong influence on this risk, with whites and blacks being much more at risk of developing MS than Asians. Having a first-order relative (parent or sibling) with MS increases the risk of developing the disease by fivefold to tenfold. Perhaps the most compelling evidence of the genetic influence on the risk of developing MS comes from studies of twins where at least one twin has MS.12 Among nonidentical twins, the chances of the second twin having MS are 1% to 2%, which is similar to the risk of nontwin sibling pairs. Among identical twins, the chance of the second twin having MS is 25%, indicating the strong influence of genetic background. An estimated 10 to 15 different genes may affect the risk of developing MS, and major research efforts are under way to identify these. Thus far, only the human leukocyte antigen DR2 gene has been definitively shown to be associated with an increased risk of developing MS among individuals of northern European descent.
Viruses
Considerable interest lies in identifying the target or targets of the pernicious inflammatory response in MS.13 Viruses and microbial agents have been postulated to be associated with an increased risk of developing MS. For decades there has been interest in the possibility that one or more viruses or other microbial infections might cause MS. This interest stems from the inflammatory nature of MS and the apparent influence of environment on the risk of developing MS, both suggesting the possibility of an infectious etiology. However, although various infectious agents have been reported to be associated with MS—including measles, Epstein-Barr virus, distemper virus, coronavirus, retrovirus, herpes simplex, human herpesvirus-6, and Chlamydia pneumoniae—there is no convincing evidence at present of a linkage between any infectious agent and MS.14 The lack of evidence does not exclude the possibility that an infectious agent causes MS, but as of now there is no widely accepted evidence associating MS with any specific virus or other microbe.
Environment
Geographic and Seasonal Influences
The association with latitude and MS prevalence has shown mixed results and is confounded by factors that include migration, lifestyle habits, biological influences, and social factors. However, in general there is an increased prevalence of MS in northern latitudes (high risk) and a decreased prevalence in southern latitutdes (low risk). People who move from a low-risk to a high-risk area before age 15 acquire a higher risk of developing MS, whereas those who make the same move after adolescence retain a lower risk.9,15 These observations suggest that an environmental exposure in the first two decades of life influences the risk of developing MS. They also suggest that early sunlight exposure, which is correlated to serum vitamin D levels, may influence the risk for developing MS.16
Although not consistent to all geographic areas,17 there are several European epidemiologic studies showing an association between season of birth and risk of developing MS 18,19 These studies indicate that there is a lower risk for MS for births occurring after summer and a higher risk for MS for births occurring after winter. The authors reporting these findings suggest that maternal levels vitamin D during the third trimester of pregnancy may influence the risk for MS, lower risk when maternal vitamin D levels are high (summer months) and higher risk when maternal vitamin D levels are low (winter months). Taken together, there is some evidence to suggest that sunlight exposure and vitamin D levels at a young age may have an influential role in the risk of developing MS.
Diet
Diet may play a role as an environmental risk factor for acquiring MS. The first investigations into diet and MS centered around trying to explain why inland farming communities in Norway had a higher incidence than areas near the coastline. It was discovered that the diets of the farmers were much higher in animal and dairy products than the diets of the coastal dwellers, whose diet was enriched by cold-water fish.20 Additional studies have since correlated consumption of animal fat, animal protein, and meat from nonmarine mammals with the risk for MS.21
In a review of epidemiologic data reporting the relationship between diet and MS from 1952 through 1995, the authors concluded that multiple studies suggested that the risk of MS was significantly correlated with the following parameters: consumption of animal fat, animal protein, and meat from nonmarine mammals.21 However, a large prospective cohort study using data from the Nurses’ Health Study and Nurses’ Health Study II found no evidence linking risk of MS with intake of saturated fats. The authors did note, however, that intake of linolenic acid, an omega-3 fatty acid, but not fish oils or docosahexanoic acid, was associated with a trend toward a lower risk for MS.22
Using data from the same cohorts, this same group also found no relationship between intake of fruits and vegetables and risk of MS.23 A case-control study in Canada assessing the relationship between nutritional factors and risk of MS in 197 incident cases of MS and 202 frequency-matched controls found a positive association between animal fat intake and risk of MS.24 Taken together, these studies suggest that there is a modest influence of diet on the risk of developing MS.
 Diagnostic Considerations
Diagnostic Considerations
MS remains a clinical diagnosis.25 No single test such as a blood test, MRI examination, or cerebrospinal fluid (CSF) study “diagnoses” MS. The diagnosis rests on a knowledgeable physician taking a history, performing a neurologic examination, conducting various tests, and then making a diagnosis on the basis of all the data. In general, only neurologists have sufficient training and experience to make an accurate diagnosis. The diagnosis of MS rests on the objective demonstration of two or more areas of demyelination in the CNS that have occurred more than one time, and a diagnosis cannot be based only on a patient’s symptoms.
Means of “objective” demonstration of areas of demyelination include the neurologic examination, MRI of the brain and spinal cord, and electrophysiologic tests (called evoked potentials) that assess visual, auditory, and somatosensory pathways. CSF examination can also be useful in establishing the inflammatory nature of a given patient’s condition. In evaluating patients for possible MS, the CSF is evaluated for the presence of plasma cells that are producing immunoglobulins (IgGs) within the CNS by assessing for qualitative (oligoclonal bands) and quantitative (total IgG, IgG index, and IgG synthesis rate) IgG changes. Excluding the presence of other disorders that can masquerade or be misdiagnosed as MS is also important, such as unusual causes of cerebrovascular disease, vitamin B12 deficiency, spinal cord compression from tumors, herniated disks or spinal canal stenosis, vascular malformations of the spinal cord, Lyme disease, and various other disorders. Although MS was formerly difficult to diagnose, MRI scanning has significantly improved the ability to diagnose MS in its early stages, because it allows imaging of areas of demyelination in the brain and spinal cord and also helps exclude the presence of other diseases that might explain the patient’s symptoms.
 Therapeutic Considerations
Therapeutic Considerations
Conventional Treatments
The conventional approach to treating MS includes the use of medications to control disease activity and rehabilitation interventions designed to alleviate symptoms resulting from damage to the CNS. Medications that help decrease disease activity (also called disease-modifying agents, or DMTs) in RRMS include human recombinant interferon-β (Avonex, Betaseron, and Rebif); glatiramer acetate (Copaxone), a random polymer of four amino acids that stimulates protective T cells; a monoclonal antibody against α-4 integrin (Tysabri); fingolimod (Gilenya), the only oral agent that prevents activated lymphocytes from entering the CNS by sequestration in lymph nodes25a,25b; and a chemotherapy agent (Novantrone).26–31
Compared with placebo, these medications decrease the relapse rate by 30% to 50%, decrease new lesion formation in the brain as detected by MRI, and decrease the risk of developing permanent neurologic disability. An immunosuppressant (chemotherapy agent), mitoxantrone (Novantrone), has also been shown to decrease disease activity in patients with rapidly progressive forms of MS.32 A monoclonal antibody (Tysabri) that prevents inflammatory cells from entering the CNS has been shown to decrease the rate of MS exacerbations and reduce disease activity (MRI lesions) compared with placebo.26,27 Fingolimod (Gilenya), that was FDA approved in 2010, reduces CNS inflammation and axonal damage by retaining lymphocytes in the lymph nodes so fewer are able to enter the CNS. Fingolimod has been shown to reduce relapse rates by 50%, decrease rate of disease progression, and decrease disease activity (MRI lesions).25a,25b Corticosteroids, such as methylprednisolone, given in high doses can decrease the duration of relapses of MS but do not affect the degree of eventual recovery for relapses.33 A number of different medications are useful for treating various symptoms of MS, such as fatigue, bladder dysfunction, and spasticity, but these medications do not reverse damage that has already occurred or decrease disease activity.
Natural Medicine Therapeutic Considerations
From a natural medicine standpoint, there are four major approaches to treating MS:
Diet Therapy
Swank/Low-Saturated-Fat Diet
Dr. Roy Swank has provided evidence that a diet low in saturated fats maintained over a long period of time tends to retard the disease process, reduce the number of attacks, and decrease mortality.34–36 Swank began treating patients with his low-fat diet in 1948. The approach to using a low-fat diet supplemented with cod liver oil is based on epidemiologic studies that found a decreased incidence of MS in populations that had a low consumption of animal fats with a high consumption of cold-water fish.
Based on current knowledge of the pathogenesis of MS, the rationale of using the Swank diet or other diets low in saturated fats in patients with MS relates to the general health benefits of such a diet and the antiinflammatory and perhaps neuron membrane–stabilizing effects of a diet enriched with omega-3 fatty acids. Although the consumption of red meat is significantly restricted on the Swank diet, fish appears to be particularly indicated owing to its excellent protein content and, perhaps more importantly, its high content of omega-3 fatty acids. Cold-water fish such as mackerel, salmon, and herring are rich in omega-3 fatty acids, which include eicosapentaenoic acid (EPA) and docosahexanoic acid (DHA). As reviewed under the “Nutritional Supplements,” section, omega-3 fatty acids have antiinflammatory effects that may be of benefit in MS. In addition, because optimal neuronal functioning depends on cell membrane fluidity, which in turn depends on lipid composition, optimal essential fatty acid (EFA) levels may be important in exerting neuroprotective effects by maintaining healthy neuronal functioning.37–39 Decreasing animal fats and increasing omega-3 fatty acids in the diet thus may improve neuronal function by modulating neuronal lipid composition.
Since Dr. Swank’s observational studies, two pilot studies evaluating diet in MS have been conducted. An open-label study evaluated the effects of a diet low in saturated fats combined with fish-oil supplementation and vitamin B complex and vitamin C in newly diagnosed RRMS.40 Beside dietary modifications, subjects were advised to reduce their intake of sugar, coffee, tea, and alcohol and to stop smoking. Diet was monitored over 2 years by a 4-day dietary record at the end of each year and plasma fatty acid levels were monitored at baseline, year 1, and year 2.
A partially blinded, randomized controlled study evaluated the effect of low-fat dietary intervention with omega-3 fatty acid supplementation in 31 subjects with RRMS.41 The intervention lasted for 12 months and the primary outcome was quality of life, using the Short Form Health Survey Questionnaire (SF-36). Subjects were randomized into one of two groups: the “low-fat diet/fish oil” group and the “diet/olive oil” group. The low-fat diet/fish oil group followed a diet that did not exceed 15% of saturated fats (percent of totally daily calorie intake) plus fish-oil capsules (daily doses of EPA 1.98 g and DHA 1.32 g). The diet/olive oil group followed the American Heart Association’s step I diet, 30% saturated fats (percent of total daily calorie intake) plus olive-oil capsules (6 capsules of 1 g of olive oil per day). The subjects were followed for an average of 11 ± 2.9 months and the low-fat diet/fish oil group maintained better quality-of-life scores for physical well-being (although not statistically significant) than the group using olive-oil supplementation. The mental health component scores were similar in the two intervention groups. At the 6-month time point, the olive-oil group reported an improvement in fatigue as compared with the fish-oil group (P = 0.035), which continued for 12 months. For both intervention groups, relapse rates were reduced as compared with the year prior to entering the study. This study suggests that a diet low in saturated fats with fish-oil supplementation might promote better physical and mental health for people with MS. Because all subjects improved after 12 months, the study also suggests that diet modification in addition to supplementation with a “good oil” (fish oil or olive oil) may be beneficial in people with MS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree