Fig. 6.1
X-ray showing posterior displacement of the tibia on the femur. The radiographic posterior drawer is indicative of PCL tear. PCL posterior cruciate ligament

Fig. 6.2
a and b X-ray and CT respectively showing reverse segond fracture, which is osseous avulsion of meniscotibial ligament. CT computerized tomography

Fig. 6.3
Two different patients with X-rays demonstrating the “arcuate sign.” a Nondisplaced avulsion fracture of fibular head. b Mildly displaced avulsion fracture of the fibular head
MRI
When evaluating the dynamic and static knee stabilizers, the obtained MRI should be of high resolution. Optimally, imaging should be on a 1.5-Tesla magnet or higher, with small field-of-view (FOV) images of the knee, and should be tailored to evaluate ligaments, tendons, and cartilage. That is to say, large FOV images that cover from the mid femur through the mid tibia result in lower-resolution images, and potentially missed pathology. A high-quality exam is important to accurately evaluate the large stabilizers, but it is even more important to evaluate the complex, blending medial and lateral capsular stabilizers, subtle coexistent meniscal tears, and articular cartilage defects. MRI should be performed in the acute setting, because as normal healing progresses and edema resolves, injuries may become less conspicuous.
PCL
The knee is typically imaged in extension, where the anterior cruciate ligament (ACL) is taut and straight, and the PCL is lax and curved. This position is comfortable for the patient, and allows for the technologist to utilize a knee coil for high-resolution MR images. Unlike the ACL, the normal PCL is homogeneously low signal on both T2 and proton density (PD) weighted sequences, lacking internal striations that may be seen in the normal ACL [7, 8] (Fig. 6.4). The knee is not typically imaged in flexion, because a knee coil cannot be utilized, resulting in lower resolution images. However, when imaged in flexion, the PCL appears taut and remains homogeneously low in signal (Fig. 6.5). The normal PCL should measure 6 mm or less, when measured from anterior to posterior in the sagittal plane [9]. Like the ACL, the PCL has two functional bundles, the posteromedial bundle (PMB) and anterolateral bundle (ALB), named according to their femoral attachments [10]. In the axial plane, the separate bundles can often be distinguished from one another (Fig. 6.6). The meniscofemoral ligaments can often be seen coursing adjacent to the PCL, with the posterior meniscofemoral ligament (Wrisberg) being more common than the anterior meniscofemoral ligament (Humphey). Not uncommonly both meniscofemoral ligaments are present [11].


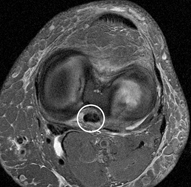

Fig. 6.4
a and b Normal PCL. Sagittal PD nonfat-suppressed image and sagittal T2 fat-suppressed image demonstrate normal appearance of PCL. The PCL is not taut like ACL when imaged in extension and thus has curved rather than straight morphology. The normal PCL is hypointense on PD and T2 weighted images. PCL posterior cruciate ligament, PD proton density, ACL anterior cruciate ligament

Fig. 6.5
a and b Normal PCL in flexion. Coronal PD nonfat-suppressed and T2 fat-suppressed image shows knee imaged in mild flexion without a knee coil. PCL is taut in flexion rather than usual curved appearance in extension. Note lower quality images due to imaging without a knee coil. PCL posterior cruciate ligament, PD proton density
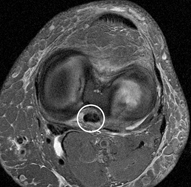
Fig. 6.6
Normal PCL. Axial T2 fat-suppressed image shows normal PCL, which is homogeneously low in signal. Anterolateral and posteromedial bundles are intact, but blend imperceptibly with one another. PCL posterior cruciate ligament
MRI is the radiologic study of choice in diagnosing acute PCL tears [7]. The sagittal MRI sequences quickly screen for PCL injury and determine the site of failure at the femoral attachment, midsubstance, or tibial attachment. MRI readily demonstrates acute high-grade injuries to the PCL (Figs. 6.7, 6.8, 6.9). However, unlike ACL tears, PCL tears are more commonly partial rather than complete [7]. In the sagittal plane, partially torn PCL tears often demonstrate a “stretched” appearance with thickening greater than 6 mm and intrasubstance signal changes, the latter of which may be seen only on PD sequence but not on T2 weighted sequences [9]. There are two potential pitfalls if one relies only on the sagittal plane when evaluating PCL tears. First, partial tears may be interpreted as complete tears. Second, mucoid degeneration may mimic a PCL tear in the setting of a functionally stable ligament. In this regard, we have found that the axial plane is complementary to the sagittal plane and can safeguard against the aforementioned pitfalls.
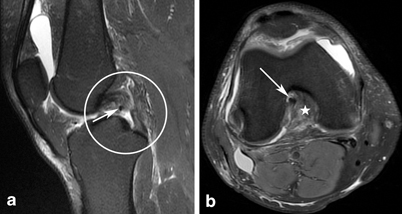
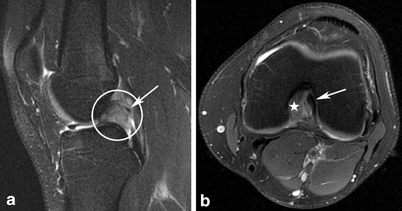
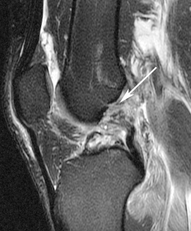
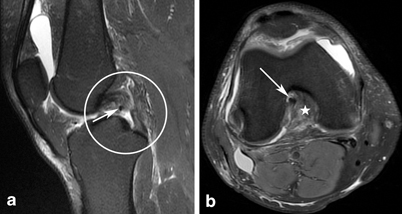
Fig. 6.7
Complete PCL tear. a Complete midsubstance disruption with intact femoral and tibial attachments intact. Note subjacent Humphries ligament (arrow). b Axial image shows empty notch (star) other than ACL (arrow), consistent with complete PCL tear involving PM and AL bundles. PCL posterior cruciate ligament, ACL anterior cruciate ligament, PM posteromedial, AL Anterolateral
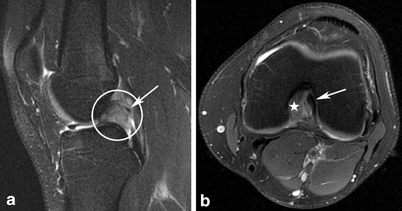
Fig. 6.8
Complete PCL tear. a Fat-suppressed T2 sagittal demonstrates complete proximal disruption of PCL. Note overlying Wrisburg ligament (arrow). b Axial image shows empty notch (star) other than ACL (arrow), consistent with complete tear involving PM and AL bundles. PCL posterior cruciate ligament, ACL anterior cruciate ligament, PM posteromedial, AL anterolateral
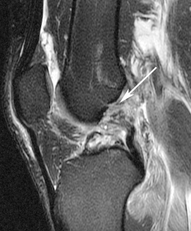
Fig. 6.9
Femoral avulsion PCL. Sagittal T2 fat-suppressed image demonstrating femoral avulsion of PCL (arrow). Axial image at femoral attachment showed complete tear (not shown). PCL posterior cruciate ligament
In the axial plane, the anterolateral and PMBs are often apparent and side by side, so we can better determine if the tear is partial or complete, depending on if one or both bundles are torn (compare Figs. 6.7 and 6.10 respectively). Mucoid degeneration of the ACL has been described as a pitfall resulting in false positive ACL tears on MRI [12]. More recently, mucoid degeneration of the PCL was described [13]. Both mucoid degeneration and partial PCL tears may demonstrate thickening and intrasubstance signal changes in the sagittal plane. The axial images help us to distinguish mucoid degeneration from PCL tear, because the former demonstrates the “tram-track” sign. The tram-track sign is defined as a single, linear striation in the PCL that does not surface, so is surrounded by low signal in all planes [13] (Fig. 6.11). In contradistinction, incomplete PCL tears demonstrate multiple heterogeneous internal striations that extend to the outer surface somewhere along the course of the ligament in the sagittal and/or axial planes (compare Figs. 6.10 and 6.11).
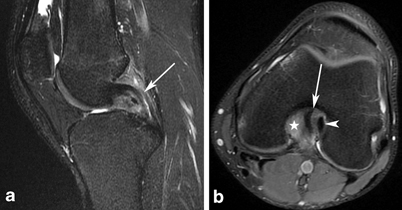
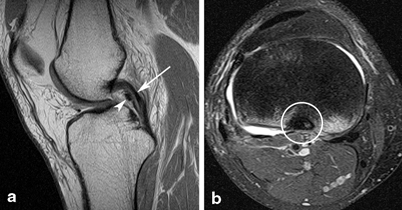
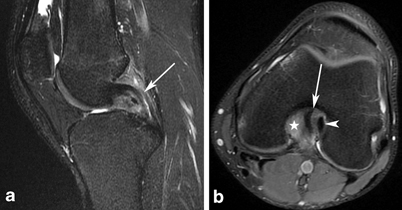
Fig. 6.10
Partial PCL tear. a Sagittal and axial T2 fat-suppressed images showing moderate grade midsubstance PCL injury. Intrasubstance striated signal changes with no visualization of tibial attachment. b Arrow shows normal ACL. PCL is diminutive with intact AL bundle (arrowhead) and fluid signal at expected location of torn PM bundle (star). PCL posterior cruciate ligament, ACL anterior cruciate ligament, AL anterolateral, PM posteromedial
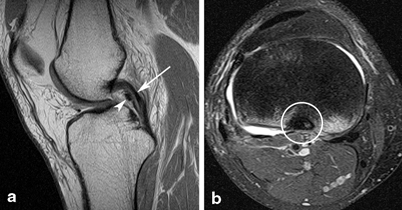
Fig. 6.11
PCL mucoid degeneration. a Nonfat-suppressed proton density (PD) image demonstrates mild linear intrasubstance fluid bright signal changes. b Axial T2 fat-suppressed image midsubstance of PCL. Signal changes do not reach the surface of the ligament on sagittal or axial sequences. Femoral and tibial attachments are intact. Note Humphries ligament (arrowhead). PCL posterior cruciate ligament
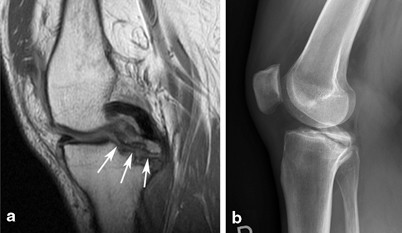
Fig. 6.12
Osseous avulsion of PCL. a Nonfat-suppressed PD images show intact PCL with osseous avulsion of PCL at tibial attachment (arrows). b Corresponding X-ray shows osseous avulsion as well. Note hypointense fracture margins on MRI and sclerotic fracture margins on X-ray, consistent with chronic rather than acute injury. PCL posterior cruciate ligament, PD proton density, MRI magnetic resonance imaging
Although chronic PCL injuries may be apparent on MRI (Figs. 6.12 and 6.13), MRI is not as sensitive in diagnosing chronic compared to acute PCL tears [14, 15]. Furthermore, MRI may appear normal as soon as 3 months following low- to moderate-grade PCL injuries [16]. Stress radiograph s, such as the Telos system, are accurate in their ability to evaluate for functional instability of the PCL [17, 18]. Given the above challenges in diagnosing chronic partial PCL tears on MRI, stress radiographs are useful to evaluate functional stability of the PCL in the presence of an indeterminate MRI that demonstrates mild PCL thickening and/or mild PCL signal changes (Fig. 6.14).
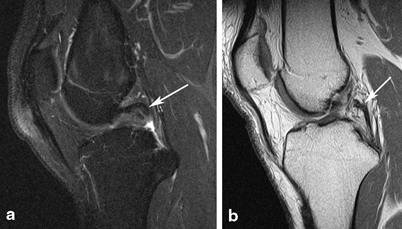
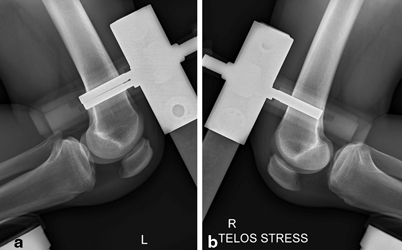
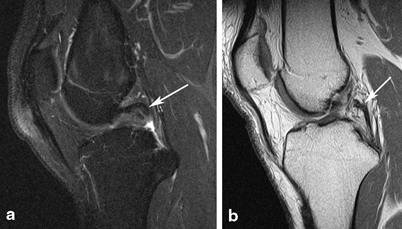
Fig. 6.13
Two patients with high-grade chronic tears. a T2 fat-suppressed image shows remote, complete nonosseous avulsion of PCL at tibial attachment with proximal retraction. b PD nonfat-suppressed images show marked attenuation of PCL with nonvisualization of femoral attachment, consistent with chronic tear. PCL posterior cruciate ligament, PD proton density
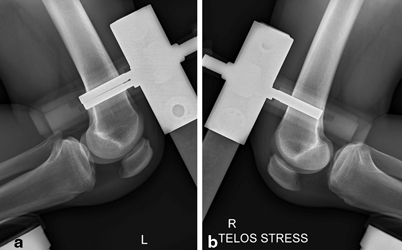
Fig. 6.14
a and b Stress radiographs of both knees with history of remote injury and only mildly thickened PCL on MRI (MRI not shown). Note posterior displacement of the right tibia on the femur in right knee with stress, with ~ 10-mm corrected side: side differential compared to normal left knee. PCL posterior cruciate ligament, MRI magnetic resonance imaging
Lateral and Posterolateral Corner Stabilizers
The large lateral stabilizers such as the iliotibial band (ITB), FCL, biceps tendon, and the conjoined insertion of biceps and FCL are well seen on MRI , and hence injuries are accurately characterized. MRI evaluation of the smaller ligamentous and capsular structures, such as the popliteofibular ligament and capsular ligaments, are challenging due to their diminutive size, oblique course relative to traditional imaging planes, and anatomic variation [1].
The FCL courses obliquely from anterior to posterior in the lateral and posterolateral aspect of the knee. The obliquely oriented biceps femoris courses from posterior to anterior. These two structures converge to form a “conjoined tendon insertion” as they insert onto the lateral aspect of the fibular head [19, 20]. Both structures are homogeneously low in signal on all pulse sequences, with the exception of their conjoined insertion, which we note often demonstrates faint, thin striations (Fig. 6.15). Injuries to the biceps, FCL, and their conjoined insertion are relatively straightforward due to the size of these structures. Figures 6.16, 6.17, and 6.18 demonstrate various injuries to the FCL.





Fig. 6.15
Normal FCL, biceps, and popliteus origin on coronal T2 fat-suppressed images. a Normal FCL (arrowheads) and partially imaged biceps tendon at their conjoined insertion (arrow). Note popliteus origin as well (circle). b Normal biceps tendon insertion is striated (arrow), which does not indicate pathology. FCL fibular collateral ligament

Fig. 6.16
Moderate- to high-grade FCL tear. Coronal T2 fat-suppressed image showing moderate- to high-grade injury to FCL, as denoted by intrasubstance and periligamentous edema (arrowheads). FCL fibular collateral ligament

Fig. 6.17
Complete disruption of FCL. Coronal T2 fat-suppressed image with nonvisualization of FCL (arrowheads) with the exception of edematous distal fibers at conjoined insertion, consistent with high-grade injury. Partially imaged biceps insertion was intact (arrow). Popliteus origin and popliteofibular ligament were intact (not shown). FCL fibular collateral ligament

Fig. 6.18
Avulsion of conjoined tendon insertion. Coronal T2 fat-suppressed image showing avulsion of FCL at the fibular attachment with proximal retraction of ~ 1 cm (circle). More posteriorly located biceps tendon insertion was intact (not shown). FCL fibular collateral ligament
The popliteus tendon and popliteofibular ligament are strong stabilizers of the PLC of the knee. The origin of the popliteus tendon is intra-articular from a sulcus on the lateral femoral condyle, inferior and anterior to the proximal attachment of the FCL [19, 20]. As the popliteus tendon wraps posteromedially, it become extra-articular at the meniscal hiatus and gives off a branch that acts as a pulley; this popliteofibular ligament courses laterally and inserts on the medial aspect of the fibular styloid process, medial to the attachment of the fabellofibular ligament and arcuate ligament [19–21].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








