Patellar instability is a common problem, and medial patellofemoral ligament (MPFL) injury is inherent with traumatic patellar dislocations. Initial nonoperative management is focused on reconditioning and strengthening the dynamic stabilizers of the patella. For those patients who progress to recurrent instability, further investigation into the predisposing factors is required. MPFL reconstruction is indicated in patients with recurrent instability and insufficient medial restraint due to MPFL injury. A technique of MPFL reconstruction is outlined. This procedure may also be performed in combination with other realignment procedures.
Key points
- •
Preoperative evaluation for risk factors of patellar instability is warranted to identify contributing factors to instability apart from medial patellofemoral ligament (MPFL) pathology.
- •
The evaluation begins with examination of knee under anesthesia to confirm patellar instability.
- •
Diagnostic knee arthroscopy is performed to note morphology of trochlea, chondral injuries, and lateral displacement of the patella.
- •
During harvest of hamstring tendon, complete dissection of adhesions from semitendinosus should be ensured and damage to superficial medial collateral ligament should be avoided.
- •
Placement of patellar tunnel at the junction of the proximal and middle thirds of the patella is recommended.
- •
Risk of patellar fracture should be limited by drilling the patellar tunnel only to a depth of about 20 mm with sequential cleaning of the bit every few millimeters while using copious irrigation to limit thermal damage.
- •
It should be ensured that the patellar tunnel avoids violation of anterior cortex and subchondral bone.
- •
Femoral tunnel placement is aided by fluoroscopy on a true lateral view of the knee for anatomic graft position.
- •
Graft should be tunneled through the soft tissue in an extrasynovial manner in layer 2 of the knee.
- •
To avoid overconstraint by the graft, fixation should be done with the knee in 50° to 60° of flexion.
- •
This technique re-creates the neutralizing force on the patella; additional procedures may be needed if medicalization of the patella is desired to address lower limb malalignment.
Introduction
Dislocation of the patella represents 2% to 3% of all knee injuries. The MPFL is nearly always injured with patellar dislocation and is the main restraint to lateral patellar translation. Recurrent patellar instability may occur in 15% to 40% of patients who have been treated nonoperatively for first-time patellar dislocations. This rate may increase up to 49% for patients who have had 2 prior patellar dislocations. Recurrent instability episodes may lead to further cartilage injury, debilitating pain, and limitation of activities of daily living, and may limit return to sport.
This subset of patients that continues to have instability episodes may have predisposing factors that contribute to patellar instability, which include:
- •
Femoral anteversion
- •
External tibial torsion
- •
Genu valgum
- •
Patellar dysplasia
- •
Trochlear dysplasia
- •
Patella alta
- •
Vastus medialis obliquus atrophy
- •
Pes planus
- •
Generalized hyperlaxity
Valgus malalignment of the knee results in an increased Q angle and increased laterally directed force on the patella. In kind, increased femoral anteversion and external tibial torsion results in rotational malalignment that may result in an increased lateral force vector to the patella and possible lateral subluxation. As the knee flexes, the proximal soft tissue restraints of the patella, including the MPFL, guide it into the trochlear groove. In deep flexion, the bony constraints of the patellofemoral articulation provide stability. In patients with patella alta, this bony constraint occurs at a deeper flexion angle and can be more prone to dislocation or subluxation. In patients with trochlear dysplasia, the patellofemoral articulation yields insufficient constraint to lateral translation in flexion.
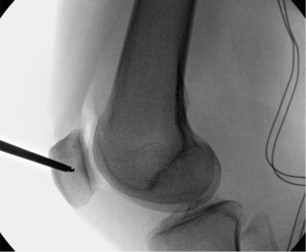
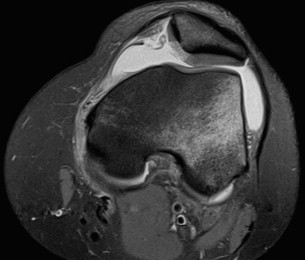
For patients with traumatic causes of patellar instability, the MPFL tears ( Fig. 1 ) and leads to loss of static restraint to lateral patellar translation. Injury of the MPFL may occur at the patellar origin, the femoral insertion, or the MPFL may sustain an intrasubstance tear. Injury may also occur at a combination of these sites.
The goal of nonoperative treatment is to recondition and strengthen dynamic stabilizers of the patella. In situations in which adequate therapy does not yield sufficient dynamic stabilization of the patella, reconstruction of the MPFL may be required. For patients who have failed nonoperative management, reconstruction of the MPFL is an accepted method to restore static medial stabilization. For patients with other predisposing factors outlined earlier, further evaluation should be performed to determine the need for additional procedures to address the underlying abnormal anatomy and causes of recurrent subluxation.
Acute repair of the MPFL has been studied in the literature. With regard to primary patellar dislocation and acute MPFL injury, Camanho and colleagues described 33 patients with a minimum of 25-months’ follow-up. Of the 33 patients, 16 patients had nonoperative treatment with bracing and physical therapy and 8 had recurrent dislocations; 17 patients had MPFL repair and none had recurrent dislocations. All those who had MPFL repair had improved Kujala scores. Numerous other investigators, however, have not had as much success with acute repair. Christiansen and colleagues reported on 77 patients with 2-year follow-up in a randomized controlled trial. All patients had arthroscopy and then were randomized to MPFL repair versus nonoperative treatment. Of the total, 42 patients had MPFL repair with a 17% redislocation rate; 35 patients were treated in a nonoperative manner, and 20% of these had redislocation. In this group of patients, MPFL repair did not reduce the recurrence rate of dislocation and there were no improvements in the Kujala score.
Multiple studies have described MPFL reconstruction using anatomic and radiographic methods to obtain accurate tunnel placement. Anatomic femoral and patellar tunnel placement is important in re-creating MPFL anatomy. If nonanatomic tunnel positions are used, then abnormal tension may be created, leading to increased patellofemoral contact pressures, pain with flexion or extension, early arthrosis, loosening or graft stretching, and recurrent instability.
Introduction
Dislocation of the patella represents 2% to 3% of all knee injuries. The MPFL is nearly always injured with patellar dislocation and is the main restraint to lateral patellar translation. Recurrent patellar instability may occur in 15% to 40% of patients who have been treated nonoperatively for first-time patellar dislocations. This rate may increase up to 49% for patients who have had 2 prior patellar dislocations. Recurrent instability episodes may lead to further cartilage injury, debilitating pain, and limitation of activities of daily living, and may limit return to sport.
This subset of patients that continues to have instability episodes may have predisposing factors that contribute to patellar instability, which include:
- •
Femoral anteversion
- •
External tibial torsion
- •
Genu valgum
- •
Patellar dysplasia
- •
Trochlear dysplasia
- •
Patella alta
- •
Vastus medialis obliquus atrophy
- •
Pes planus
- •
Generalized hyperlaxity
Valgus malalignment of the knee results in an increased Q angle and increased laterally directed force on the patella. In kind, increased femoral anteversion and external tibial torsion results in rotational malalignment that may result in an increased lateral force vector to the patella and possible lateral subluxation. As the knee flexes, the proximal soft tissue restraints of the patella, including the MPFL, guide it into the trochlear groove. In deep flexion, the bony constraints of the patellofemoral articulation provide stability. In patients with patella alta, this bony constraint occurs at a deeper flexion angle and can be more prone to dislocation or subluxation. In patients with trochlear dysplasia, the patellofemoral articulation yields insufficient constraint to lateral translation in flexion.
For patients with traumatic causes of patellar instability, the MPFL tears ( Fig. 1 ) and leads to loss of static restraint to lateral patellar translation. Injury of the MPFL may occur at the patellar origin, the femoral insertion, or the MPFL may sustain an intrasubstance tear. Injury may also occur at a combination of these sites.
The goal of nonoperative treatment is to recondition and strengthen dynamic stabilizers of the patella. In situations in which adequate therapy does not yield sufficient dynamic stabilization of the patella, reconstruction of the MPFL may be required. For patients who have failed nonoperative management, reconstruction of the MPFL is an accepted method to restore static medial stabilization. For patients with other predisposing factors outlined earlier, further evaluation should be performed to determine the need for additional procedures to address the underlying abnormal anatomy and causes of recurrent subluxation.
Acute repair of the MPFL has been studied in the literature. With regard to primary patellar dislocation and acute MPFL injury, Camanho and colleagues described 33 patients with a minimum of 25-months’ follow-up. Of the 33 patients, 16 patients had nonoperative treatment with bracing and physical therapy and 8 had recurrent dislocations; 17 patients had MPFL repair and none had recurrent dislocations. All those who had MPFL repair had improved Kujala scores. Numerous other investigators, however, have not had as much success with acute repair. Christiansen and colleagues reported on 77 patients with 2-year follow-up in a randomized controlled trial. All patients had arthroscopy and then were randomized to MPFL repair versus nonoperative treatment. Of the total, 42 patients had MPFL repair with a 17% redislocation rate; 35 patients were treated in a nonoperative manner, and 20% of these had redislocation. In this group of patients, MPFL repair did not reduce the recurrence rate of dislocation and there were no improvements in the Kujala score.
Multiple studies have described MPFL reconstruction using anatomic and radiographic methods to obtain accurate tunnel placement. Anatomic femoral and patellar tunnel placement is important in re-creating MPFL anatomy. If nonanatomic tunnel positions are used, then abnormal tension may be created, leading to increased patellofemoral contact pressures, pain with flexion or extension, early arthrosis, loosening or graft stretching, and recurrent instability.
Indications
With the reportedly high recurrence rate with nonoperative management, surgical intervention may be necessary. Numerous procedures to address patellofemoral instability have been described. Some of these include medial retinacular reefing and lateral release. These procedures can result in recurrent subluxation, continued knee pain, and iatrogenic medial instability. The goal of reconstruction of the MPFL is to re-create a static medial restraint to lateral patellar translation while the knee is in extension and assist in guiding the patella into the trochlear groove.
The most common indication for MPFL reconstruction includes recurrent patellar instability with failed nonoperative management. Patients with chronic instability and trochlear dysplasia may also benefit from MPFL reconstruction.
Contraindications
Contraindications to MPFL reconstruction are few. Systemic or local infection is an absolute contraindication. If MPFL reconstruction alone is performed when coexisting factors for instability exist, then there is a higher potential for graft failure. MPFL reconstruction should not be performed to pull or recenter the patella. In this clinical setting, addressing malalignment and malrotation in combination with MPFL reconstruction may be indicated.
Surgical technique
Preoperative Planning
Preoperatively, the patient’s operative extremity should be assessed for previous surgeries, including scars or previous hamstring harvest. In addition, anteroposterior (AP), lateral, and merchant radiographs may be obtained to evaluate associated tibial tubercle malalignment or trochlear dysplasia.
Schöttle and colleagues performed a cadaveric study describing a method of radiographic identification of the femoral insertion of the MPFL. To maintain isometry, a point within 5 mm of the anatomic MPFL femoral insertion should be used. Redfern and colleagues have shown that a fluoroscopically guided technique can accurately identify the anatomic origin of the MPFL, which is accomplished with a true lateral view of the distal femur and by identifying a point 0.5 mm anterior to the distal posterior cortex and 3 mm proximal to Blumensaat line.
Preparation and Patient Positioning
The patient should be positioned supine on a standard operating room table. After induction of general anesthesia, the knee is examined to confirm patellar laxity. A nonsterile tourniquet is then placed on the proximal thigh. A kidney post is placed laterally to assist with stability of the extremity with the knee at 90° flexion. The contralateral extremity is well padded to prevent undue pressure. AP and lateral fluoroscopic images should be taken before prepping and draping the extremity. The C-arm fluoroscopy unit should be positioned on the operative side, with the sterile table and instruments placed at the foot of the bed.
The operative extremity is prepared with ethanol followed by ChloraPrep (Care Fusion Corporation, San Diego, CA, USA). A down sheet is then placed under the limb, and the distal extremity placed in a stockinette with Coban wrap (3M, St Paul, MN, USA). Sterile U-drapes and an extremity drape complete the draping process.
Surgical Approach
Graft harvest
If an autograft is chosen, a 3- to 4-cm anteromedial incision is made over the proximal tibia at the level of the tibial tubercle at the midpoint in the sagittal plane. The semitendinosus is identified and bluntly dissected with a right-angle clamp. Blunt dissection is used to identify and develop the plane between the superficial medial collateral ligament (MCL) and the pes tendons. The semitendinosus is then released off the tibia and whipstiched with a #2 FiberWire suture (Arthrex, Inc, Naples, FL, USA). Traction is applied to the tendon, and adhesions are released with Metzenbaum scissors, until the muscle belly of the semitendinosus can be easily palpated. The tendon is stripped with a tendon stripper. Graft diameter is a typically 4 to 5 mm in size. The pes anserine is then closed with 0 Vicryl suture, and subcutaneous tissues are closed with 3-0 monocryl suture.
Patellar preparation
A 2- to 3-cm incision is made along the medial border of the patella ( Fig. 2 ). A full-thickness subperiosteal flap including the MPFL and medial retinaculum are elevated off the proximal third of the patella in an extrasynovial, extra-articular manner.
With this exposure, the C-arm is brought in and a perfect lateral radiograph is obtained to localize the junction between the proximal and middle thirds of the patella. A guidewire is then placed at this point and drilled approximately 25 mm into the patella ( Fig. 3 ). C-arm images are taken to confirm that the patella is drilled in appropriate dimensions in both the coronal and sagittal planes to avoid cortical or articular penetration ( Fig. 4 ). A 5-mm cannulated drill bit (Arthrex MPFL Convenience Pack) is used to drill a tunnel of at least 20 mm in the patella. The drill bit has small flutes, so it is important to ream in a staged manner, removing the reamer to clean the flutes and proceeding slowly with ample irrigation to minimize heat necrosis. The edges of the tunnel are curetted to allow for easy passage of the graft ( Fig. 5 ).