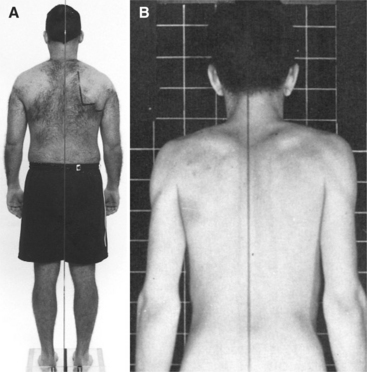
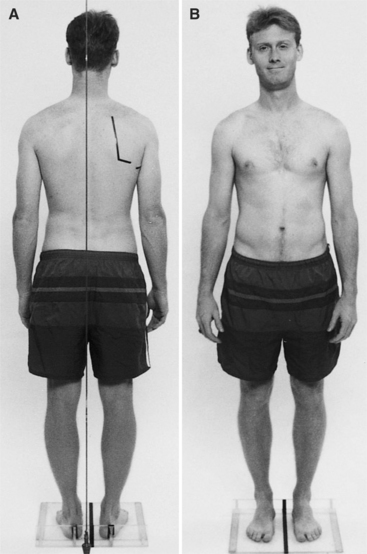
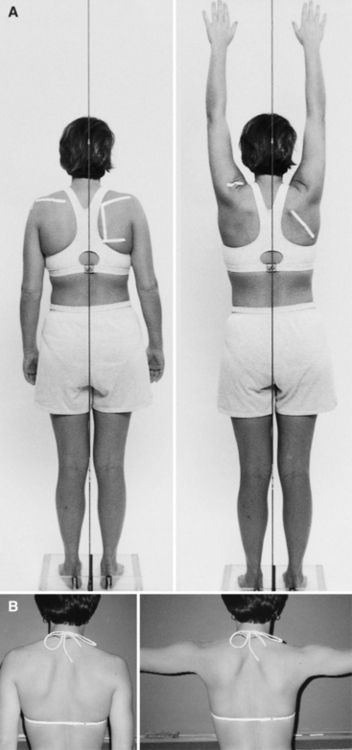
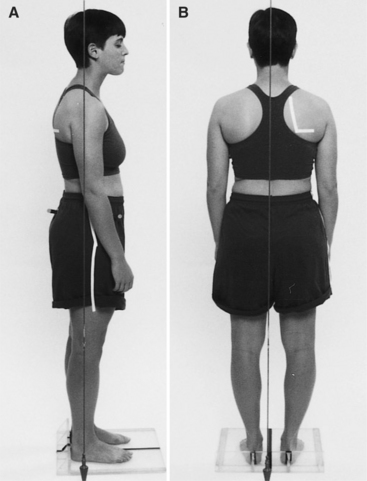
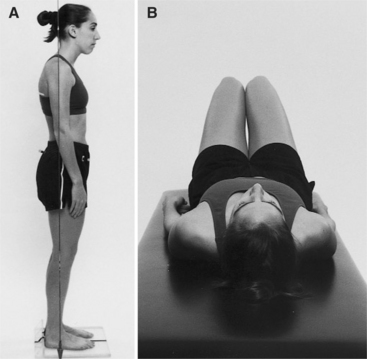
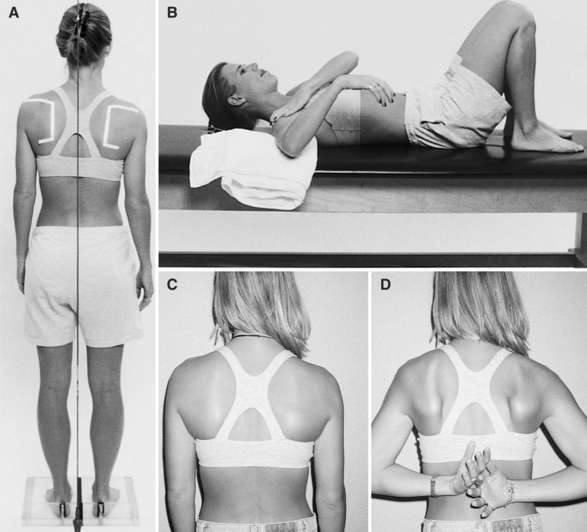
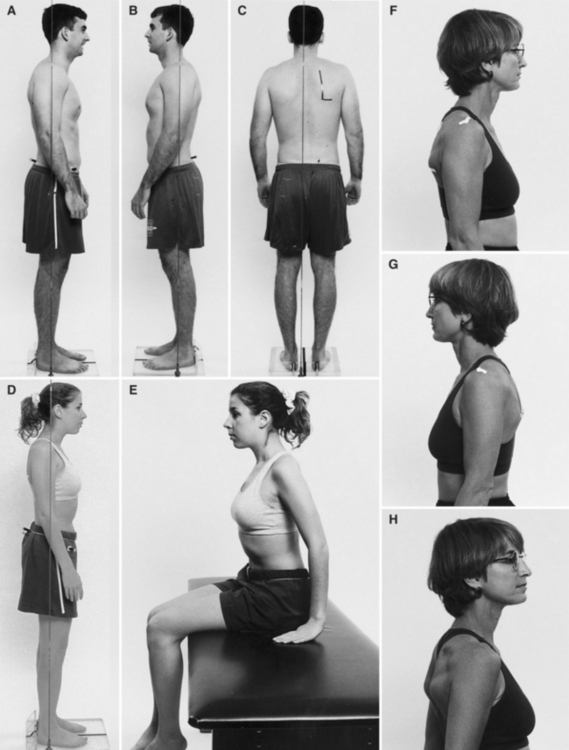
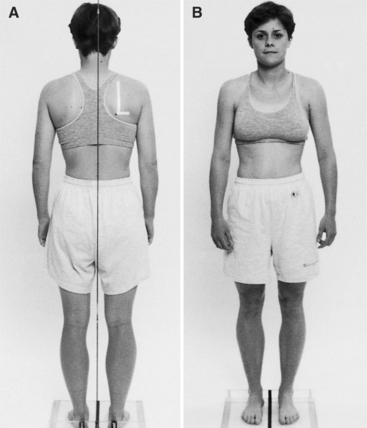
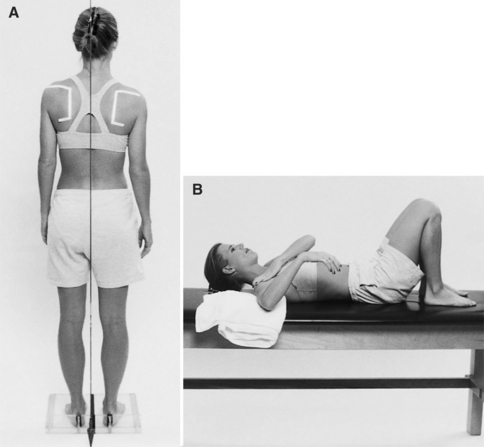
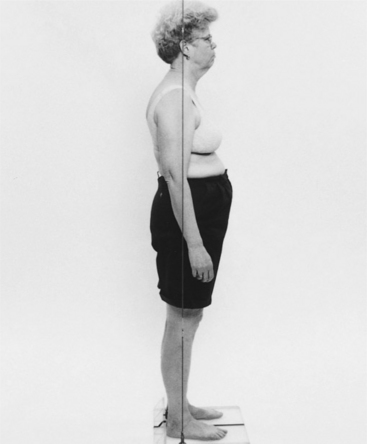
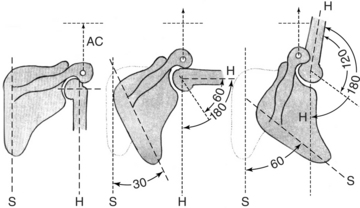
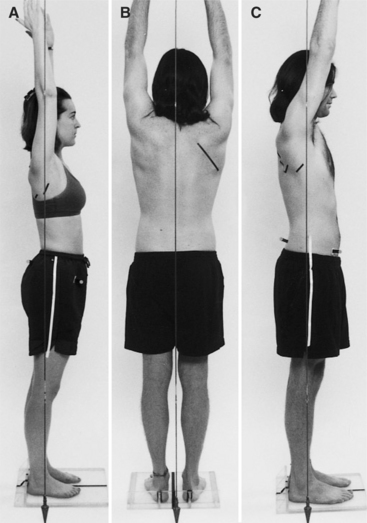
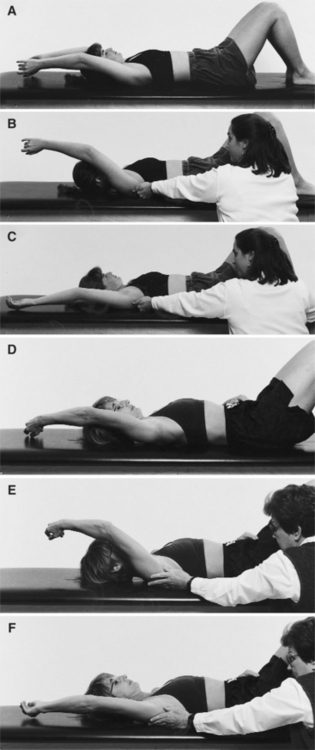
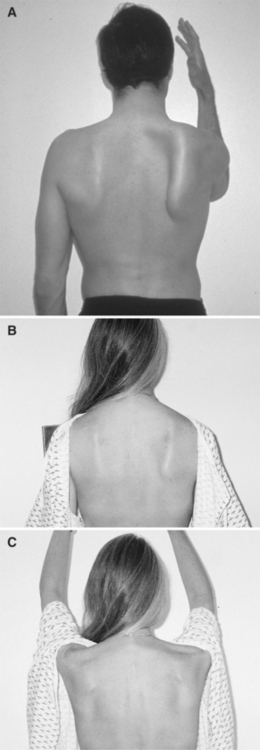
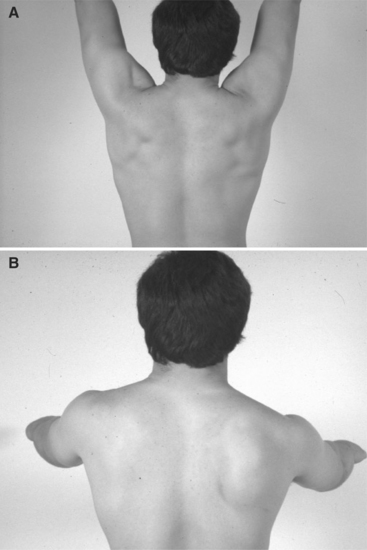
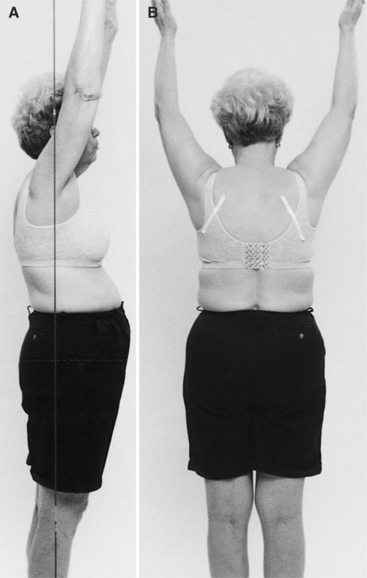
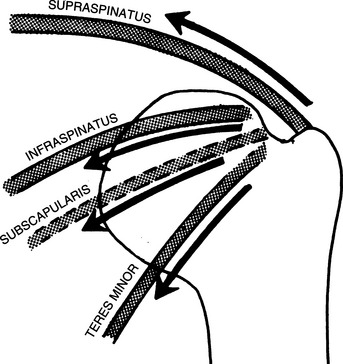
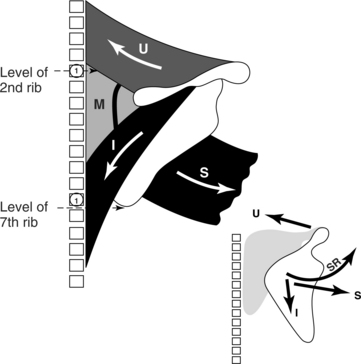
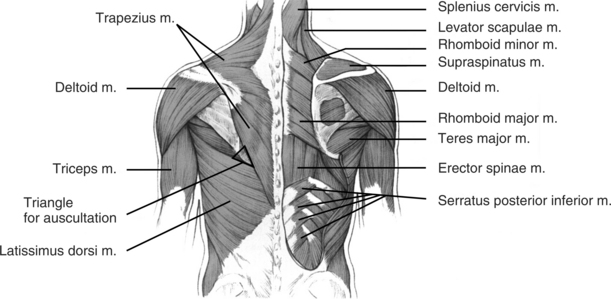
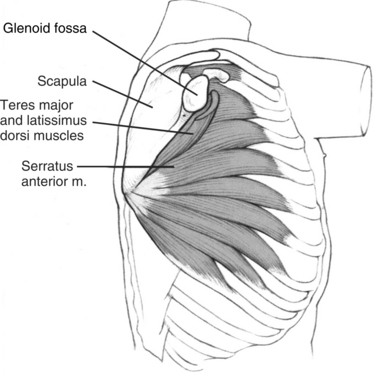
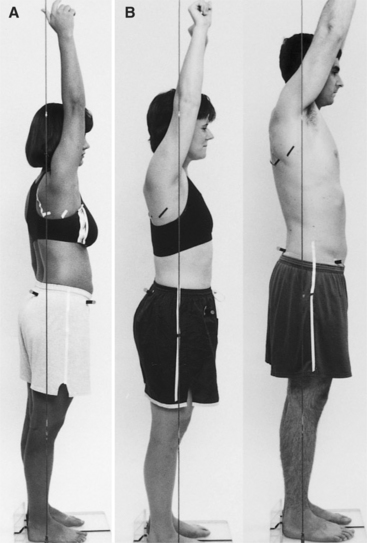
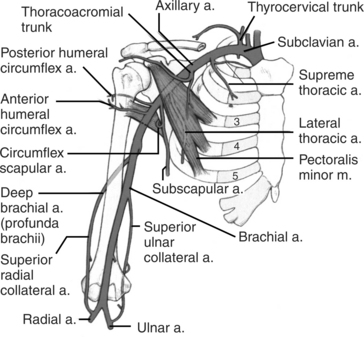
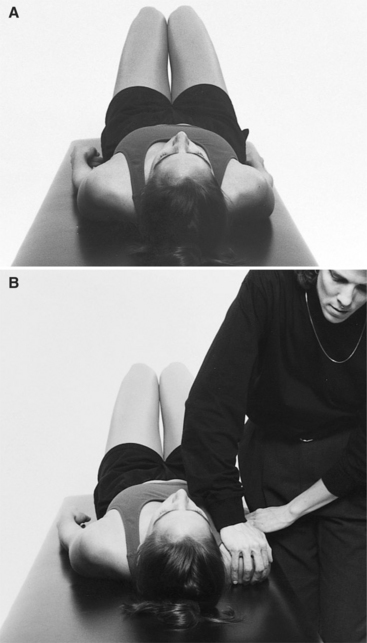
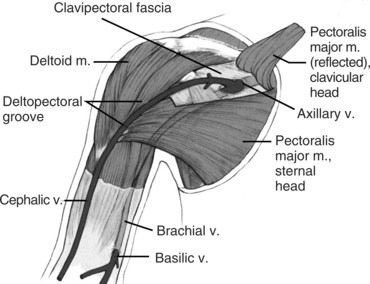
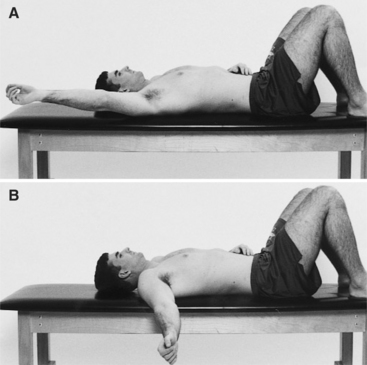
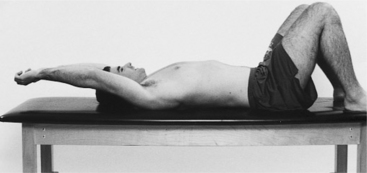
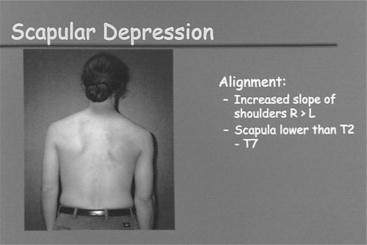
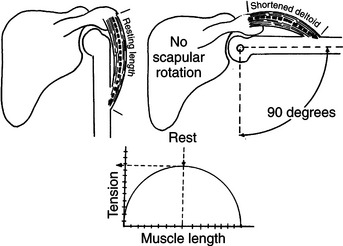
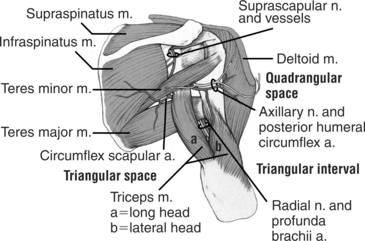
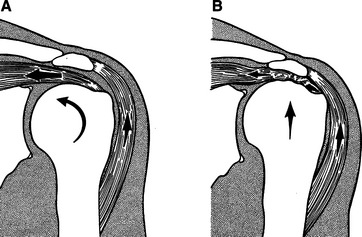
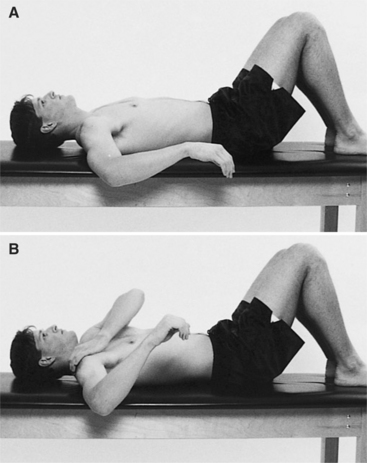
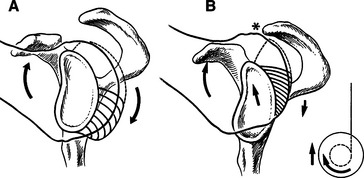
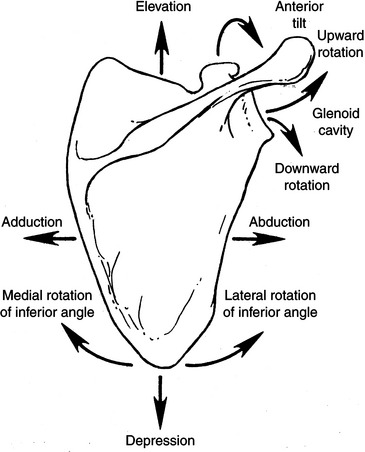
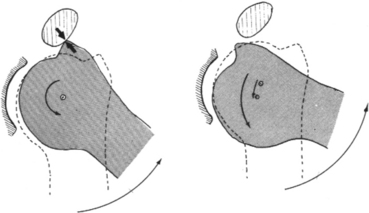
Chapter Five After considering the information presented in this chapter, the reader will be able to: 1 Describe kinesiology of the musculature of the shoulder girdle with emphasis on the counterbalancing actions of muscles and their roles in the force-couples that control shoulder motion. 2 Identify the characteristics of each movement impairment syndrome of the scapulothoracic and glenohumeral joints. In treating the patient with shoulder pain, the reader will be able to: 1 Perform an examination, consider the contributing factors, and establish the diagnoses, both primary and secondary, if indicated. 2 Develop and instruct the patient in a diagnosis-specific treatment program and modification of life’s activities, which contribute to the formation of the movement impairment syndrome. The therapeutic exercises and the correction of the movement patterns used to perform daily activities become the means to remedy the identified movement impairments. The observation of the movement characteristics and their effect on symptoms are the primary guides to the diagnosis and treatment of the movement impairments. If symptoms are associated with the impairment, the correction of the movement will alleviate the symptoms. For example, increasing the amount of lateral humeral rotation during shoulder flexion/elevation often eliminates the shoulder pain caused by one form of impingement. Because the scapula plays a critical role in controlling the position of the glenoid, relatively small changes in the action of thoracoscapular muscles can affect the alignment and forces involved in movement around the glenohumeral joint.31,32 Clinically based observations suggest that most syndromes involving the shoulder arise from impairments in the timing and control of scapular motion. Specific pain problems of the muscles and tendons arise from repeated movements that have altered their normal patterns rather than from a single episode of isolated stress placed on the specific painful tissue. For example, supraspinatus tendinitis or tendinopathy is a common pain problem that is attributed to overuse or to impingement from altered biomechanics of the shoulder, rather than from using the arm excessively on a particular occasion. Supraspinatus tendinopathy can begin as vascular insufficiency in the “critical zone” of the tendon.26 Tendinopathy refers to the whole range of painful conditions caused by overuse of the tendon. Tendinopathy is the preferred term to designate a condition such as tendinitis because most painful tendon conditions result from tendinosis, which has a different pathology than tendinitis and a longer healing time than the 1 to 2 weeks of tendinitis.13 Tendinopathy can be the result of mechanical impingement, compression of the rotator cuff by its surrounding local anatomic structures,18 damage of the undersurface of the cuff muscles,17 or the overuse of the muscle during movement. Neer was the first to categorize impingement syndromes into either outlet or nonoutlet. Outlet impingement resulted from damage to the cuff from contact with the structures of the coracoacromial arch, whereas non-outlet impingement occurs when there is a normal supraspinatus outlet.22 Jobe and colleagues suggest that outlet syndromes occur in individuals who are over 35 years of age and nonoutlet syndromes in those younger than 35 years of age and who participate in sports requiring overhead activities. In non-outlet syndrome, hyperangulation of the humerus that causes stretching of the anterior shoulder structures is a precipitating factor.17 Neer was the first to describe a continuum of shoulder problems that begins with impingement and progresses to rotator cuff tears.20 The limited subacromial space combined with the development of relatively small imbalances in muscle control of the scapula and humerus can lead to a wide range of soft tissue and even osseous changes. Other investigators have described the self-perpetuating cycle that can develop when the humeral depressor mechanism is dysfunctional.19 The premise that underlies movement impairment concepts is that this continuum arises from alterations in the control of scapular and humeral motions because of the changes in neuromuscular components that result from repeated use. This chapter emphasizes the need to identify the movement impairments and the component impairments that, when analyzed, form the basis of the diagnosis. Identifying these factors requires careful examination and testing. Remediation requires the appropriate selection of and instruction in the therapeutic exercises that will result in correction of the movement impairments. • Elevated. The neck appears to be short and the shoulders appear to be closer to the ears than ideal (Figure 5-1). Clarification of the anatomic reference point used to assess shoulder position is important because of the variation in muscle impairments associated with different scapular positions. The reference points for observation of shoulder height are discussed in the scapula section. • Depressed. The clavicles appear to be horizontal or the acromioclavicular joint is lower than the sternoclavicular joint (Figure 5-2). The superior angle of the scapula is lower than T2. • Forward. When viewing the entire shoulder girdle, the tip of the shoulder at the acromion can appear to be forward because of several possible impaired scapular positions. In the forward shoulder position, the scapula can be abducted, tilted, or moved in a combination of these positions. Because each of these impaired scapular positions is associated with different muscle imbalances and requires different management, they are discussed in relation to the alignment of the scapula. The vertebral border of the scapula is parallel to the spine and is positioned approximately 3 inches from the midline of the thorax.28 It is situated on the thorax between the second and seventh thoracic vertebrae. The scapula is flat against the thorax and is rotated 30 degrees anterior to the frontal plane. • Downwardly rotated. The inferior angle of the scapula is medial to the root of the spine of the scapula rather than the vertebral border being parallel to the spine (Figure 5-3). Most often, the levator scapula muscle and rhomboid muscles are short and the upper trapezius muscle is long. The serratus anterior muscle may also be long. This is one of the most common alignment impairments in individuals with shoulder pain. Figure 5-3 Downwardly rotated scapula. The thoracic kyphosis contributes to this alignment of the scapula. • Depressed. The superior border of the scapula is positioned lower than the second and seventh thoracic vertebral landmarks (see Figure 5-2). This postural position infers that the upper trapezius muscle is long. Muscles that may contribute to this depressed position are the pectoralis major and the latissimus dorsi muscles. This alignment is also common in patients with shoulder pain. A postural alignment of depression that is not corrected during shoulder flexion and abduction contributes to stress at the glenohumeral and acromioclavicular joints. • Elevated. The elevation of the superior angle of the scapula, but not the acromion, suggests that the levator scapula muscle is short (see Figure 5-1). The elevation of the entire scapula, including the acromion, infers that the upper trapezius muscle is short. In this condition the lateral portion of the clavicle appears notably higher than the medial portion. If the levator scapula, rhomboid, and upper trapezius muscles are all short, then the entire spine of the scapula will appear higher and will be positioned closer to the seventh cervical vertebra than to the second thoracic vertebra and the scapula may also appear adducted. • Adducted. The vertebral border of the scapula is less than 3 inches from the midline of the thorax (Figure 5-4). The rhomboid and the trapezius muscles may be short while the serratus anterior muscle is long. • Abducted. The vertebral border of the scapula is more than 3 inches from the midline of the thorax (Figure 5-5). When the scapula is abducted, it is also rotated more than 30 degrees anterior to the frontal plane. When the scapula is abducted and rotated anteriorly, the glenoid will face anteriorly and the humerus will appear medially rotated. The medial rotation of the humerus in this condition should not be corrected because the orientation of the humerus in the glenoid is correct. When the patient adducts his or her scapula, the humeral position will be correct and appears normal. In the abducted-rotated scapular alignment, if the humeral position appears correct with the cubital fossa facing anteriorly, the actual alignment is one of lateral rotation. Often specific examination of the length of the lateral rotators indicates that they are short. The most common cause of the abducted-rotated scapular position is shortness of the serratus anterior and/or the pectoralis major muscles. • Tilted or tipped. The inferior angle protrudes away from the rib cage (Figure 5-6). Most often, this alignment is associated with shortness of the pectoralis minor muscle. Another cause of the tilted alignment is shortness of the biceps brachii muscle, the short head attaches to the coracoid process or to the anterior deltoid muscles or to both. If the biceps brachii muscle is short, then the elbow will flex when the scapular alignment is corrected. If the elbow is passively flexed while the scapula is held in the corrected position, then the shoulder will extend if the biceps brachii muscle is the source of the tilted scapula. If the shoulder remains flexed, then the most likely source of the tipped shoulder is the anterior deltoid muscle and/or the coracobrachialis muscle. • Depressed and tilted. The scapula is depressed as described previously, but the scapula is also anteriorly tilted. • Abducted and tilted. This alignment is the combination of the conditions of abduction and tilted, each of which has been described previously. • Winged. The vertebral border protrudes posteriorly from the thorax (Figure 5-7). This alignment is often associated with weakness of the serratus anterior muscle. Other alignment impairments that can contribute to the appearance of winged scapula include a flat thoracic spine, a rounded back, or scoliosis. In scoliosis, the scapulae appear notably asymmetrical in their alignment. When the subscapularis is hypertrophied, the scapulae will appear to be winged because the vertebral borders of the scapulae are prominent. However, they are not actually rotated in the frontal plane but are no longer flat on the thorax. Careful examination of the scapula indicates that the entire scapula is protruding from the thorax and not just from the vertebral border. This condition is seen most often in patients who regularly perform chin-up exercises or wall-climbing activities. • Upwardly rotated. The root of the spine of the scapula is medial to the inferior angle. The muscle most likely to be short is the trapezius muscle. There should be less than one third of the humeral head protruding in front of the acromion. Neutral rotation should be present so that the antecubital crease faces anteriorly and the olecranon faces posteriorly, with the palm of the hand facing the body. In some cases, the palm of the hand may face posteriorly without the olecranon facing posteriorly. Most often this condition is the result of short finger flexor muscles (Figure 5-8). The proximal and distal ends of the humerus should be in the same vertical plane when viewed from the side, the front, or the back. As discussed previously, the scapula must be in ideal alignment when properly assessing the glenohumeral joint position. • Anterior. More than one third of the humeral head is positioned anterior to the acromion (Figure 5-9). • Superior. The humeral head appears superior in relation to the acromion. • Abducted. The distal part of the humerus is away from the side of the body, or the scapula is downwardly rotated or depressed (Figure 5-10). • Rotated medially. The cubital fossa faces medially, the olecranon faces laterally, and often the palm of the hand faces posteriorly. As discussed previously the position of the scapula must be assessed for accurate assessment of humeral rotation. • Rotated laterally. Lateral rotation of the humerus is not common except when the scapula is abducted and the humerus appears to be in the correct alignment (Figure 5-11). • Flexion/extension. With flexion of the humerus, the distal aspect of the humerus is anterior to the proximal aspect of the humerus. With extension of the humerus, the distal end of the humerus is posterior to the proximal end of the humerus, which may also be associated with anterior position of the humeral head. The position of the humerus must be assessed in relation to the position of the scapula. What appears to be the correct alignment can be impaired depending on the position of the scapula, and vice versa. • Kyphosis. There is increased outward (posteriorly orientated) curve or flexion of the thoracic spine (Figure 5-12). • Scoliosis. Kyphosis and rotation of the spine with a rib hump that often results in malalignment of the scapula. When the alignment of the scapulae are markedly different, scoliosis is the most common cause. If a rib hump causes the scapula to wing, the patient should not be encouraged to correct the alignment by sustained contraction of the scapular adductors. The resulting shortness of the adductors restricts the abduction and upward rotation of the scapula and can lead to impingement, rotator cuff tears, and neck pain. The neck pain occurs because of the additional stress exerted on the cervical spine by contraction of the upper trapezius muscle in its role as an upward rotator of the scapula. • Flat. The loss of the normal outward curve resulting in a straight or flat thoracic spine. A flat thoracic spine makes the scapula appear to be winged. Glossary of Scapular Motions14 The following definitions are described to ensure commonality in understanding the segmental movements upon which the syndromes are based (Figure 5-13). • Rotation, lateral or upward, is movement about a sagittal axis in which the inferior angle moves laterally and the glenoid cavity moves cranially. • Rotation, medial or downward, is movement about a sagittal axis in which the inferior angle moves medially and the glenoid cavity moves caudally. • Elevation is a gliding movement in which the scapula moves cranially, as in shrugging the shoulder. • Depression is a gliding movement in which the scapula moves caudally and is the reverse of elevation and anterior tilt. • Adduction is a gliding movement in which the scapula moves toward the vertebral column. • Abduction is a gliding movement in which the scapula moves away from the vertebral column and into full abduction, following the contour of the thorax until it assumes a posterolateral position. • Anterior tilt is a movement about the coronal axis in which the coracoid process moves in an anterior and caudal direction. The coracoid process may be said to be depressed anteriorly. • Winging occurs around the vertical axis at the acromioclavicular joint. The vertebral border of the scapula moves away from the thorax, and the glenoid fossa moves anteriorly. This motion occurs to maintain the contact of the scapula with the curve of the thorax as the scapula slides (glides) around the thorax into abduction or adduction. The movement becomes abnormal when the motion of the vertebral border of the scapula away from the thorax becomes obvious.24 • Starting alignment. As discussed previously, if the scapula and humerus are not in the correct starting position, then during movement these faults must be corrected. For example, if the scapula is downwardly rotated, then during shoulder flexion the amount of upward rotation must be greater than the normal 60 degrees to compensate for the faulty starting position. • Scapulohumeral rhythm. During the first 60 degrees of shoulder flexion and 30 degrees of abduction the movement of the scapula is highly variable. Inman and Saunders termed this the setting phase.10 After the setting phase the humerus and scapula move in a constant ratio. A ratio of 2 degrees of glenohumeral motion for 1 degree of scapulothoracic motion results in 120 degrees of glenohumeral joint motion and 60 degrees of scapular motion at the completion of shoulder flexion (Figure 5-14). More recent studies have reported some variability in the exact timing of that motion.2,6,7 In analyzing patients who have pain, comparing one shoulder with the other provides a reference point to guide the examiner in making a decision as to whether the movement is impaired or just a normal variation. Observations of deviations in timing and range of scapular motion combined with the timing of the onset of pain and identification of impairments of muscle performance further guide decisions regarding the importance of the deviations. • Timing and range of scapular motion. During flexion the scapula will often stop its movement when the shoulder is flexed to about 140 degrees; the rest of the motion occurs almost entirely at the glenohumeral joint. Placing the thumb and first finger on the inferior angle of the scapula and following the motion of the scapula while observing the humerus is a good way to assess the movement pattern. Comparing one side with the other during unilateral and bilateral motion is also helpful. Upon the completion of flexion, the inferior angle of the scapula should be close to the midline of the thorax and the vertebral border of the scapula should be rotated 60 degrees (Figure 5-15). The inferior angle should not be forward of this line, nor should it protrude laterally more than ½ inch in full glenohumeral joint flexion or abduction. The movement of the inferior angle beyond the midline or the protrusion of the scapula laterally beyond the thorax indicates excessive scapular abduction (Figure 5-16). • Scapular winging. The scapula should not wing during arm movement, either during the flexion/abduction phase or during the return from flexion/abduction phase (Figures 5-17 and 5-18). • Scapular elevation. There should be some elevation of the shoulder (as in the shrugging motion), but it should not be excessive during the flexion/abduction phase. If the shoulder is depressed at rest, then elevation of the scapula is particularly important. • End of the range. The scapula should slightly depress, posteriorly tilt, and adduct to complete the motion of 180 degrees. The presence of a kyphosis or shortness of the pectoralis minor muscle can impede this depression (Figure 5-19). • Humeral head. The axis of rotation of the humeral head should stay relatively constant so that it is centered in the glenoid throughout the motion (Figure 5-20). Therefore the scapulohumeral muscles that depress the head of the humerus must offset the strong upward pull of the deltoid muscle and must laterally rotate the humerus to prevent the greater tuberosity from impinging on the coracoacromial ligament or the acromion (Figure 5-21). If the pectoralis major and latissimus dorsi muscles depress the head of the humerus, they will also medially rotate it and can alter the timing of humeral motion with the scapula and the position of the humerus relative to the glenoid. • Spine. Minimal movement of the spine should occur during full abduction or flexion of the shoulder. If the thoracic spine is kyphotic, the scapula will be tilted anteriorly by the convexity of the ribs, thus limiting the apparent range of shoulder flexion. Decreasing the degree of the thoracic kyphosis will improve the range of shoulder flexion. • Test for rhomboid dominance. When the patient has his arms at his sides with the elbows flexed and is instructed to perform shoulder lateral rotation, the scapula should not adduct, particularly during the first 35 degrees of the motion (Figure 5-22). Adduction of the scapula is interpreted as a sign of rhomboid dominance and poor control of glenohumeral lateral rotation. The desired motion is one in which the humerus is rotating in the glenoid about a vertical axis. The humeral head should not move anteriorly or superiorly; nor should the arm extend. These faulty movements of the humeral head demonstrate dominance of the posterior deltoid muscle over the infraspinatus and teres minor muscles. The correct length, strength, and pattern of participation of the muscles attaching to the thorax and to the scapula are important. The thoracoscapular muscles are responsible for the movement of the scapula, which must maintain an optimal relationship with the humerus to minimize abnormal stresses at the glenohumeral joint. A key to optimal glenohumeral joint motion is that the head of the humerus remains centered in relationship to the glenoid as motion occurs at the shoulder joint. The path of the instantaneous center of rotation (PICR) of the humerus in the glenoid defines motion in the glenoid (see Figure 5-20). This requires relatively precise timing of the muscles that produce scapular motion. The force couple action of the trapezius and serratus anterior muscles must be carefully assessed because this action is a key to motion of the scapula (Figure 5-23). Alterations in the relative participation of these muscles or restriction of motion by their antagonists disrupt the pattern of movement. Because shoulder motion does not involve true reciprocal muscular activity, most of the thoracoscapular muscles are active during shoulder motion although they have antagonistic actions. The trapezius muscle (Figure 5-24) adducts and upwardly (laterally) rotates the scapula. The upper trapezius muscle elevates the scapula, whereas the lower trapezius muscle depresses the scapula. The trapezius muscle attaches to the acromion and clavicle. When the upper trapezius muscle is short and the shoulder girdle is posturally elevated, the entire shoulder, including the distal end of the acromion, should be elevated. When the upper trapezius muscle is long, the shoulder is depressed (see Figure 5-2). If the scapula fails to elevate during shoulder flexion or abduction, the action of the upper trapezius muscle is considered to be insufficient. The levator scapula muscle (see Figure 5-24) adducts and downwardly (medially) rotates the scapula. This muscle is a synergist of the trapezius for adduction but an antagonist for rotation. The levator scapula muscle attaches to the transverse processes of the first four cervical vertebrae. This muscle can restrict cervical rotation and in the presence of excessive cervical joint flexibility may rotate the cervical spine during shoulder motions. For example, during shoulder flexion, the levator scapula muscle is stretched as the scapula upwardly rotates. If the cervical vertebrae are more flexible than the levator scapulae muscle is extensible, the stretch of the muscle will rotate the cervical vertebrae and, in some instances, actually rotate the head to the same side as the muscle being stretched. Because the levator scapula muscle attaches to the medial aspect of the superior angle of the scapula, shortness of this muscle can give the impression of an elevated shoulder if the examiner observes the shoulder height near the base of the neck (Figure 5-25). The attachment of the levator scapula muscle to the superior angle of the scapula can elevate the most medial portion of the scapula but does not elevate the acromial region (see Figure 5-25). Differentiating between shortness of the levator scapula and rhomboid muscles versus the upper trapezius muscle is extremely important in designing the correct therapeutic exercises. The rhomboid muscles (see Figure 5-24) adduct and downwardly (medially) rotate the scapula. Similar to the levator scapula muscle, the rhomboid muscles are both synergists and antagonists of the trapezius muscles. These muscles usually become more dominant than the trapezius muscles and can restrict upward rotation of the scapula. The exercise of shoulder shrugging with the arms at the sides (the glenohumeral joint is in downward rotation) is usually not a desirable exercise because it reinforces the activity of the rhomboid and levator scapulae muscles, contributing to the dominance of these muscles. To emphasize upper trapezius activity, shoulder shrugging should be performed with arms overhead so that the scapula is in upward rotation (Figure 5-26). Based on many postural assessments, the author has found that depressed shoulders are a common postural impairment; thus the upper trapezius muscle is frequently elongated. The serratus anterior muscle (Figure 5-27) abducts and upwardly (laterally) rotates the scapula and holds the scapula flat against the rib cage. The upward rotation is produced by the force couple action of the serratus anterior muscle with the trapezius muscle. The serratus anterior muscle is the primary abductor of the scapula. Complete active range of shoulder flexion/elevation motion is not possible when the serratus anterior is paralyzed or becomes severely weak (manual muscle test grade of 2/5). In addition, deficient control by the serratus anterior muscle, causing impairments in the timing and range of scapular motion, can cause stress at the glenohumeral joint. This stress results from the incorrect positioning of the glenoid for glenohumeral joint motion when there is insufficient abduction and upward rotation of the scapula. If the scapula is not correctly positioned during shoulder flexion or abduction, the scapulohumeral muscles will not be able to maintain their optimal length and tension relationships. The author has found that impaired control of the scapula by the serratus anterior muscle is common. The impaired control results from the serratus anterior muscle being weak, long, short, or altered in the timing of its movement of the scapula in relation to the movement of the humerus. Careful observation of the degree of abduction or adduction of the scapula is necessary to distinguish between insufficient performance of the trapezius or of the serratus anterior muscle. Although both muscles are upward rotators, because the trapezius is an adductor and the serratus an abductor, the medial/lateral position of the scapula can be a guide as to which muscle should be emphasized during the corrective exercise program. The primary indicators of impaired performance are inadequate abduction and inadequate upward rotation of the scapula during shoulder flexion and abduction. The inferior angle of the scapula reaching the midline of the lateral side of the thorax when the shoulder is in full flexion, as well as the scapula being upwardly rotated 60 degrees at the completion of shoulder flexion, is a guide to the correct action of the serratus anterior muscle (Figure 5-28). Patients with adducted scapulae and large acromioclavicular joints should be carefully examined and tested for impaired performance of the serratus anterior muscle. If the serratus anterior muscle does not sufficiently upwardly rotate the scapula, then the participation of the upper trapezius muscle, another upward rotator, may be increased. The upper trapezius muscle attaches to the clavicle. According to Johnson et al, this segment of the trapezius muscle exerts its primary effect during the terminal portion of scapular upward rotation and can create stress on the acromioclavicular joint.13 The pectoralis minor muscle (Figure 5-29) tilts the scapula anteriorly by tilting the coracoid process anteriorly and caudally, thus causing the inferior angle to rotate medially.14 Shortness of the pectoralis minor muscle interferes with the upward rotation of the scapula. If the patient has short or stiff abdominal muscles, this restriction by the pectoralis minor muscle can be even more exaggerated. Short or stiff abdominal muscles restrict the elevation of the rib cage, thus adding greater resistance to movement of the scapula than if the rib cage elevates as a compensation for the lack of extensibility of the pectoralis minor muscle. Shortness of the pectoralis minor muscle can also contribute to thoracic outlet syndrome (see Figure 5-29). This muscle is difficult to stretch because the pressure must be applied to the coracoid process, not to the humerus, while the chest is stabilized (see Figure 5-30). Therefore the most effective stretching requires an assistant. These techniques are described in the therapeutic exercise section. Correcting the scapular position (see Figure 5-30) with the glenohumeral joint in neutral position must be performed carefully. Because the emphasis should be on posterior tilt and not on adduction of the scapula, the exercise of scapular posterior tilt performed in the standing position must be taught carefully so that adduction is not exaggerated. This exercise may not stretch the pectoralis minor muscle, and the contraction of the rhomboid muscles can reinforce the downward rotation of the scapula, which is a common problem. The author prefers that the patient try to acquire the correct scapular alignment by abducting and depressing (posteriorly tilting) the scapula when the shoulders are flexed or abducted to at least 90 degrees and the elbows are flexed. The patient should then carefully return the arms to his or her sides by moving in the shoulder joint and not allowing the scapula to anteriorly tilt during the return to neutral position of the glenohumeral joint. Management of shoulder pain syndromes requires a careful examination of the length and stiffness of the pectoralis minor muscle and the implementation of a precise stretching program when an impairment is identified. Impairments of the pectoralis major (Figure 5-31) and the latissimus dorsi (see Figure 5-24) muscles can contribute to glenohumeral joint dysfunction. These muscles essentially bypass the scapula and attach directly to the humerus and can contribute to disruption of scapulohumeral rhythm. Because both of these muscles are medial rotators of the humerus and are powerful muscles with strong and extensive attachments to the axial skeleton, the range of shoulder lateral rotation can be limited during the last one third of the range of shoulder flexion if they become short or stiff. In addition, both muscles attach farther away from the axis of rotation of the glenohumeral joint than the scapulohumeral medial rotators. When they become the dominant muscles, they can be a source of faulty control of the humerus in the glenoid. The pectoralis major muscle adducts and medially rotates the humerus. The upper fibers flex and horizontally adduct the shoulder. The lower fibers depress the shoulder girdle through their attachments on the humerus. A common clinical finding is that the fibers forming the sternal portion of the pectoralis major muscle test short, whereas the fibers forming the clavicular portion test long (Figure 5-32). The latissimus dorsi muscle medially rotates, adducts, and extends the shoulder and depresses the shoulder girdle. Acting bilaterally, the latissimus dorsi muscles can help extend the spine and anteriorly tilt the pelvis. The range of shoulder flexion/elevation is limited when the latissimus dorsi muscle is short (Figure 5-33). If the abdominal muscles are short or stiff, the back will maintain a relatively normal lumbar curvature even without an active effort to contract the abdominal muscles. If the abdominal muscles are not taut when the patient performs shoulder flexion, he or she will compensate with lumbar spine extension (Figure 5-34). 1. Shortness or stiffness of the lateral rotators. 2. Insufficient activity of the lateral rotators and therefore inadequate lateral rotation of the humerus to prevent the greater tuberosity from contacting the acromion. 3. Insufficient activity of the subscapularis muscle, which in turn allows the humeral head to glide anteriorly and superiorly. 4. Dominance of the deltoid muscle, causing the humeral head to glide superiorly. 5. Shortness of the lateral rotators and teres major muscle also impeding the maintenance of the correct axis of rotation for the humeral head. 6. Shortness of the capsule, particularly the posterior inferior part. Because the rotator cuff muscles are an intrinsic part of the capsule, shortness or stiffness of these muscles should also imply similar effects on the capsule. The deltoid muscle (see Figure 5-24) abducts the humerus. The anterior portion of the deltoid muscle flexes and medially rotates the humerus, the posterior portion extends and laterally rotates the humerus, and the middle portion abducts the humerus. This is a powerful muscle and from the rest position generates a superiorly directed vector that pulls the humeral head toward the acromion. Therefore it is essential that the depressors of the humeral head, primarily the supraspinatus, infraspinatus, teres minor, and subscapularis muscles, adequately offset the proximal pull of the deltoid muscle. Often when the deltoid muscle becomes dominant as the patient performs shoulder abduction, the humeral head glides superiorly because the downward pull of the rotator cuff muscles is insufficient and cannot counterbalance the upward pull of the deltoid. As the humerus continues to abduct, the compression forces generated by the deltoid muscle maintain the humerus in this position. If the same patient flexes rather than abducts the humerus, the movement impairment is not evident. This can be explained by the reduced participation of the deltoid muscle. During flexion, the primary activity is in the anterior portion, which is just one third of the muscle, as compared with activity of the entire deltoid muscle during abduction. Depressed shoulder joint alignment is actually abduction of the glenohumeral joint despite the patient being at rest with his arms by his sides (Figure 5-35). When the glenohumeral joint is abducted, the deltoid and supraspinatus muscles are in shortened positions. If the resting glenohumeral joint position is one of medial rotation, the combination of abduction and medial rotation of the humerus predisposes the subject to an impingement syndrome (Figure 5-36). In some cases the deltoid muscle is short; to compensate, the shoulders become depressed or downwardly rotated or both so the arms will be close to the thorax while in a standing posture. The therapist can assess this by correcting the scapular position. If the humerus then assumes an abducted position, the deltoid muscle and possibly the supraspinatus muscle are short. Figure 5-36 Depressed shoulders. When the shoulders are depressed, the glenohumeral joint is in an abducted position. Another cause of depressed shoulders, besides short deltoid and supraspinatus muscles, is when the upper trapezius muscle has become lengthened. In this condition the deltoid and supraspinatus muscles are not necessarily short as described. Normally, the scapula must upwardly rotate during abduction or the deltoid muscle will become too short to work effectively (Figure 5-37). In patients with depressed shoulders, the amount of shoulder girdle elevation must exceed that of the normal situation to compensate for the impaired starting alignment. Typically the optimal degree of elevation does not occur. Precise function of the thoracoscapular muscles is critical in providing the required control of the scapula to position the glenoid and to optimize the action of the scapulohumeral muscles. The supraspinatus muscle (Figure 5-38) abducts and laterally rotates the shoulder, depresses, and stabilizes the humeral head in the glenoid. Because this muscle passes under the acromion, it is particularly vulnerable to injury when the shoulder is depressed. If the humeral head (1) glides superiorly, (2) does not glide inferiorly during shoulder flexion and abduction, or (3) does not laterally rotate enough to prevent impingement of the greater tuberosity against the coracoacromial ligament, then the supraspinatus muscle and tendon are exposed to compression forces (Figure 5-39). A commonly used exercise that increases the risk of impingement of the greater tuberosity of the humerus against the coracoacromial ligament is shoulder abduction to 90 degrees or more with the humerus medially rotated. Because of the increased risk of impingement, this exercise should be avoided particularly in the range of 70 to 90 degrees of abduction. Many patients performing this exercise have depressed shoulders; when they abduct to shoulder height, they are abducting more than 90 degrees. In addition, performing shoulder abduction in medial rotation can contribute to anterior tilt of the scapula. If the resting postural alignment of the scapula is one of exaggerated abduction, the apparent shoulder medial rotation is actually the correct alignment of the humeral head in its relationship to the glenoid (Figure 5-40). Because the scapula follows the contour of the rib cage during abduction, the degree of rotation in the frontal plane increases. The result is that the glenoid faces more anteriorly than if the scapula is positioned correctly on the thorax. Therefore when the scapula is abducted and the glenoid faces more anteriorly than laterally, the humerus will appear to be medially rotated because the cubital fossa is facing medially. However, this alignment helps to maintain the correct relationship between the humeral head and the glenoid. The following example illustrates the importance of careful assessment. A patient is referred to physical therapy for biceps tendonitis of the right shoulder. The magnetic resonance imaging (MRI) indicates a tendon pathologic condition and superior position of the humeral head. The patient also has subluxation of the sternoclavicular joint, scoliosis, and a right rib hump contributing to abduction of the scapula. In the resting position, her cubital fossa is directed anteriorly. She does not have any range of motion limitations. Her shoulder becomes painful with use of her right dominant hand, even when she is not doing overhead or lifting activities. Based on the belief that what appears to be the correct degree of humeral rotation with her arm at her side is actually lateral rotation, she is instructed to change the manner of using her arm. She is instructed to turn the cubital fossa medially, which also means that she has to be in slight abduction to use her arm for activities such as cutting and chopping food and working on her computer. This change in alignment coincides with a major improvement in her condition. No improvement had occurred in her condition during the month before changing the degree of rotation of her shoulder during daily activities. The infraspinatus muscle (see Figure 5-38) laterally rotates and depresses the head of the humerus. The infraspinatus and teres minor muscles are the primary lateral rotator muscles that depress the head of the humerus, with some assistance from the supraspinatus. The posterior deltoid, a powerful lateral rotator, causes superior glide of the humeral head. Based on comparison of the number of muscles and their size, the medial rotators should be able to generate greater tension than the lateral rotators. The lateral rotator muscles and the posterior capsule often become short or stiff and can interfere with the posterior glide of the humeral head; thus it is extremely important that they be monitored for both their length and strength properties.19 The teres minor muscle (see Figure 5-38) laterally rotates and depresses the head of the humerus. This muscle has the same important role in depressing and laterally rotating the humeral head as the infraspinatus muscle. Deficiencies in performance of these two muscles are very common. Shortness or greater stiffness of the teres minor and infraspinatus muscles relative to the stiffness of the axioscapular muscle is common (Figure 5-41). Shortness of the lateral rotators can contribute to excessive anterior and superior glide of the humeral head. Restricted posterior glide and excessive anterior glide of the humeral head are factors in shoulder impingement syndromes.12 Neer has described how the lack of posterior capsular length contributes to impingement during flexion21 (Figure 5-42). The subscapularis muscle (see Figure 5-38) medially rotates the humerus and depresses the head of the humerus. This muscle has a particularly important role because of its angle of pull, acting not only to depress the head of the humerus but also to pull it posteriorly, thus offsetting the muscles acting to cause an anterior-superior glide of the humerus. Because large powerful muscles such as the pectoralis major and latissimus dorsi muscles are also medial rotators, the subscapularis muscle often becomes less dominant. The subscapularis and the joint capsule provide anterior glenohumeral stability.29,30 If the subscapularis becomes long or weak, the result can be excessive anterior glide of the humeral head, which has been cited as a precursor to impingement syndrome.11 If the lateral rotators are short or stiff, this can contribute further to the anterior and superior glide of the humeral head and can limit the medial rotation range, resulting in lengthening or weakening of the subscapularis muscle. In addition, if the pectoralis major is the dominant medial rotator, its attachment on a more distal portion of the humerus and its anterior pull on the humerus will further exaggerate the anterior glide of the humeral head and place pressure on the anterior joint capsule during shoulder flexion or horizontal adduction. The teres major muscle (see Figure 5-38) medially rotates, adducts, and extends the shoulder joint. Shortness of this muscle limits shoulder flexion and can impede depression and lateral rotation of the humeral head. Accurate assessment of the length of the teres major muscle is particularly important when the range of shoulder flexion is limited and when the PICR of the humeral head does not remain centered but drops inferiorly during humeral flexion or abduction. Relationship Between Alignment and Movement As discussed in Chapter 1, optimal movement performance is more easily achieved if the alignment of body segments is closer to ideal than if marked deviations in segmental alignment are present. However, several combinations of movement patterns and alignments are possible with each combination having a different implication for the examination process and the subsequent management. The following examples illustrate how alignment and movement faults are used to define the various syndromes: • The scapular alignment is correct, but the movement of the scapula is impaired. Impaired scapular movement refers to insufficient or excessive range, alteration in orientation, or inappropriate timing of scapular movement in relation to humeral motion. For example, although the subject has ideal shoulder girdle alignment, the scapula only upwardly rotates 40 degrees at the completion of shoulder flexion. • The scapular alignment is impaired, and the movement is impaired. For example, the scapula is downwardly rotated in the starting position and upwardly rotates only 40 degrees by the time the range of shoulder flexion is completed. The result could be only 35 of the 60 degrees of upward rotation that are standard for scapular rotation during shoulder flexion. • The scapular alignment is impaired, and the movement is of normal range but does not correct or compensate for the initial impaired position. For example, the scapula is downwardly rotated 10 degrees and the range of scapular upward rotation is 60 degrees, but the final position of upward rotation is still 10 degrees less than that required for optimal scapular motion during shoulder flexion. • The scapular alignment is impaired, but the movement is of sufficient range (greater than ideal) to compensate for the initial position. For example, the scapula is downwardly rotated 10 degrees, and during shoulder flexion the scapula upwardly rotates 70 degrees. Because the scapular motion is correct, the glenohumeral joint motion is not particularly impaired, but the impaired alignment of the scapula is usually associated with neck pain. Correcting scapular alignment often alleviates the neck pain or the associated referred pain arising from myofascial stress or from radiculopathy. • The primary problem is impaired scapular movement. • The impaired scapular movement often causes or is associated with impaired humeral motion. • Symptoms are reduced when the patient performs the scapular motion correctly or the therapist corrects the scapular impairment during active movement performed by the patient. For example, the therapist assists the upward rotation of the scapula when this is identified as being insufficient during shoulder flexion/elevation. Because this correction decreases or eliminates the pain, the therapeutic program is designed to correct the movement impairment and the contributing impairments. • The syndrome is named for the observed impairment that may present as abnormal, an exaggeration of normal, or an insufficient range of motion. For example, scapular downward rotation syndrome is the name assigned to the condition when either the scapular downward rotation is exaggerated during the early phases of shoulder flexion/abduction or its upward rotation movement is less than the kinesiologic standard at the completion of the motion.
Movement Impairment Syndromes of the Shoulder Girdle
Introduction
Normal Alignment of the Shoulder Girdle
Shoulders
Impaired Alignment
Scapula
Impaired Alignment

Humerus
Impaired Alignment
Thoracic Spine
Impaired Alignment
Motions of the Shoulder Girdle
Williams & Wilkins
Shoulder Girdle Movement Patterns
FA Davis
Muscular Actions of the Shoulder Girdle
Thoracoscapular Muscles
Thoracohumeral Muscles
Scapulohumeral Muscles
Movement Impairment Syndromes of the Scapula
Criteria for the Diagnosis of a Scapular Syndrome
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Movement Impairment Syndromes of the Shoulder Girdle