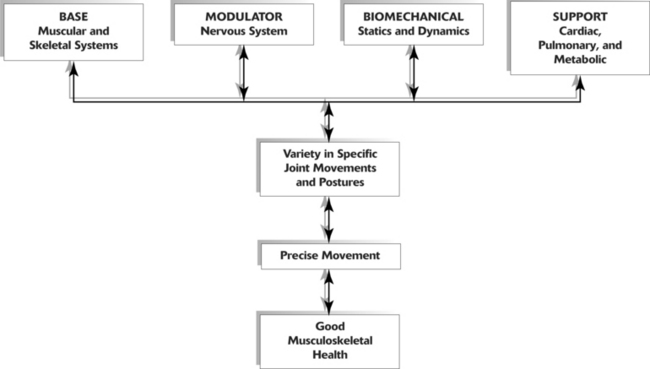
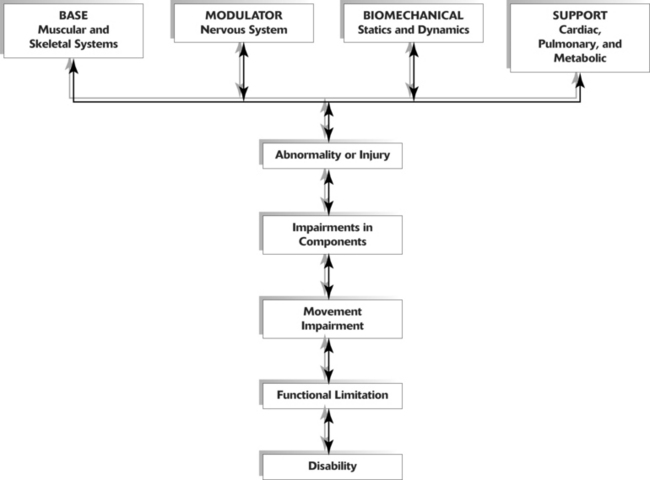
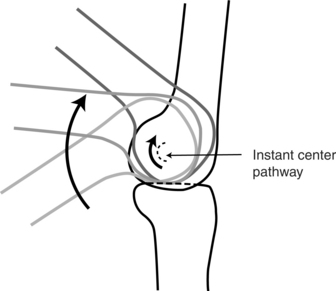
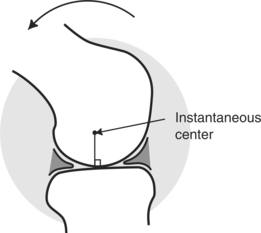
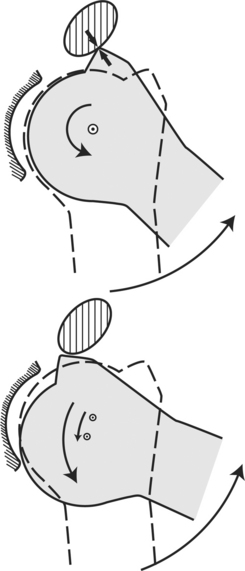
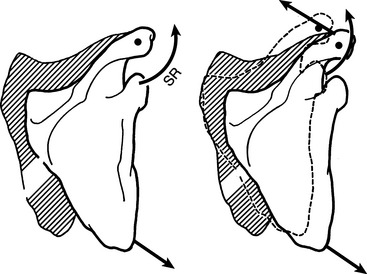
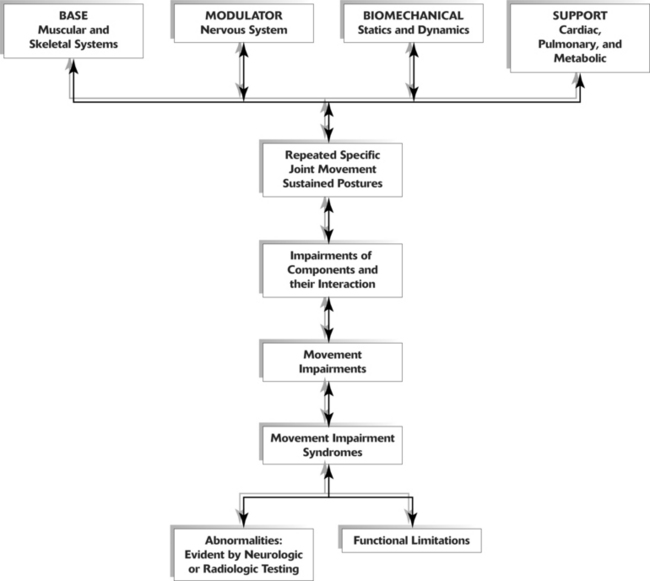
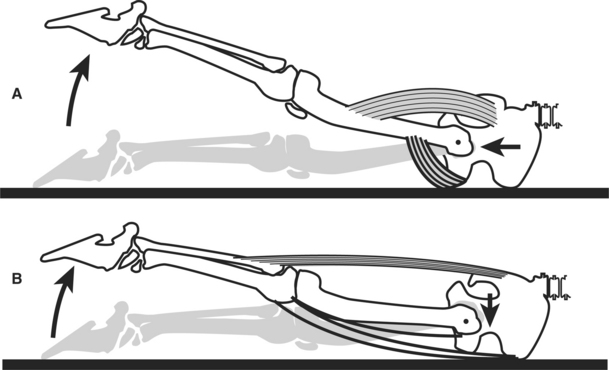
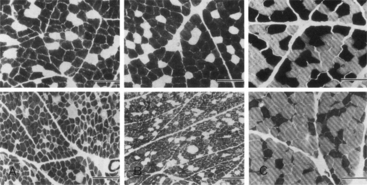
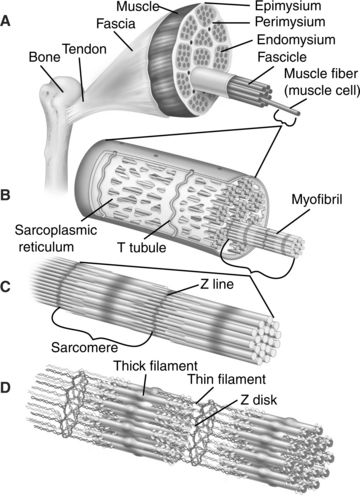
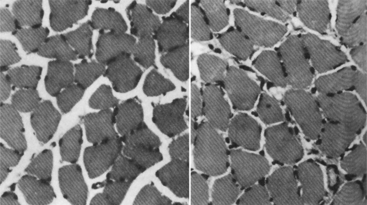
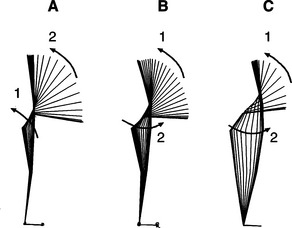
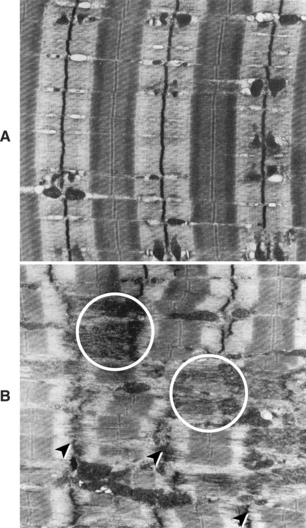
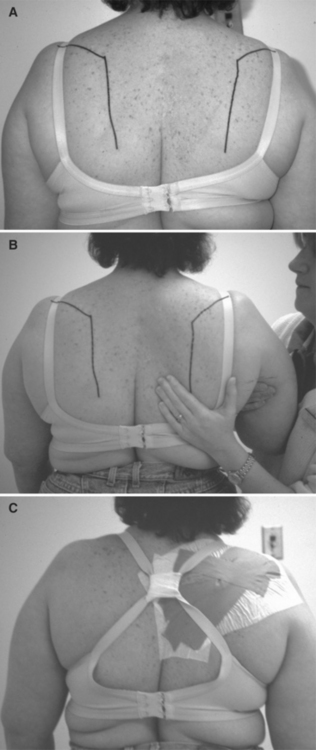
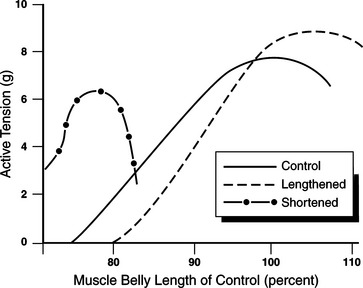
Chapter Two After reviewing this chapter, the reader will be able to discuss: 1 The components of and differences among the three models of the movement system. 2 How the muscular, nervous, and skeletal systems are affected by repeated movements and sustained postures. 3 How repeated movements and sustained postures contribute to the development of musculoskeletal pain syndromes. 4 The concept of relative flexibility, its relationship to muscle stiffness, and its implications in the role of exercise to stretch muscles. 5 The role of a joint’s directional susceptibility to movement in the development of a musculoskeletal pain syndrome. This text discusses musculoskeletal pain syndromes arising from tissue alterations that are caused by movement. Movement is considered a system that is made up of several elements, each of which has a relatively unique basic function necessary for the production and regulation of movement. Various anatomic and physiologic systems are components of these basic elements (Figure 2-1). To understand how movement induces pain syndromes, the optimal actions and interactions of the multiple anatomic and physiologic systems involved in motion must be considered. The optimal function and interaction of the elements and their components are depicted in the following kinesiologic model. Every component of the elements is essential to movement because of the unique contributions of each; however, equally essential is the interaction among the components. Each has a critical role in producing movement and is also affected by movement. For example, muscular contraction produces movement, and movement helps maintain the anatomic and physiologic function of muscle. Specifically, movement affects properties of muscle, such as tension development, length, and stiffness, as well as the properties of the nervous, cardiac, pulmonary, and metabolic systems. (The changes in these properties are discussed in detail later in this chapter.) Optimal function of the movement system is maintained when there is periodic movement and variety in the direction of the movement of specific joints. For example, a posture should not be sustained for longer than 1 hour, based on studies of the effects of sustained forces. McGill and associates have shown that 20 minutes in a position of sustained flexion can induce creep in the soft tissues, requiring longer than 40 minutes for full recovery.41 Two types of effect on soft tissues from sustained forces are described: (1) time-dependent deformation of soft tissues, and (2) soft tissue adaptations involving protein synthesis.23 A study by Light and colleagues demonstrates that 1 hour per day of sustained low-load stretching produces significant improvement in range-of-knee extension in patients with knee flexion contractures when compared with high-load stretching produced during short duration.37 The implication is that short duration stretching produces temporary deformation of soft tissues, but 1 hour of stretching may be a sufficient stimulus for long-term soft-tissue adaptations. When there is variety in the stresses and directions of movement of a specific joint, the supporting tissues are more likely to retain optimal kinesiologic behavior (defined as precision in movement) than when there is constant repetition of the same specific movement or maintenance of the same specific position. Pathokinesiology is described by Hislop as the distinguishing clinical science of physical therapy, and it is defined as the study of anatomy and physiology as they relate to abnormal movement.25 Based in part on word construction and in part on clarification of causative factors, pathokinesiology emphasizes abnormalities of movement as a result of pathologic conditions. The pathokinesiologic model (Figure 2-2) depicts the role of disease or injury as producing changes in the components of movement, which result in abnormalities of movement. In the Nagi model of disablement,45 disease leads to impairments that cause functional limitations with the possible end result of disability. Impairments are defined as any abnormality of the anatomic, physiologic, or psychologic system. Therefore abnormalities of any component system or of any movement are considered impairments. In the pathokinesiologic model, the pathologic abnormality is the source of component impairments, which then causes movement impairments, functional limitations, and often disability. Because of the interaction of the component systems as depicted in the model, identifying the secondary changes in each system is as important as understanding the primary pathologic effect on a system component. For example, in the case of hemiparesis, the movement dysfunction is the result of an abnormality involving the nervous system. Factors contributing to movement dysfunction include but are not limited to (1) an inability of the central nervous system to recruit and drive motor units at a high frequency,56 (2) the co-activation of antagonistic muscles,13 (3) a secondary atrophy of muscles that compromise contractile capacity,7 (4) the stiffness of the muscle,57 (5) a loss of range of motion from contracture,21 (6) the biomechanical alterations that are the result of insufficient and inappropriate timing of muscular activity,12,51 and (7) an internal sensory disorganization.12 In addition, the alterations of metabolic demands during activity and the aerobic conditioning of the patient must all be considered as contributing factors in the movement impairment. The degree of involvement of each of these factors and their influence on function varies from patient to patient. Physical examination formats should address all these factors and their relative importance to the patient’s functional problem. Decisions that lead to the formation of the management program must be based on the potential for remediation of each of the contributing factors and ranked according to their relative importance to the functional outcome of the patient. A common belief is that movement impairments are the result of pathologic abnormalities, but the thesis of this text is that movements performed in daily activities can also cause impairments that eventually lead to pathologic abnormalities. Therefore a different model is proposed to characterize the role of movement in producing impairments and abnormalities. The empirical basis of this model stems from observations that repetitive movements and sustained postures affect musculoskeletal and neural tissue. The cumulative effect of repetitive movements is tissue damage, particularly when the movements deviate from the optimal kinesiologic standard for movement. Human movements involve similar internal and external forces as do mechanical systems.49 In mechanical systems, maintaining precise movement is of such importance that the science of tribology is devoted to the study of factors involved in movement interactions. Tribology is defined as the study of the mechanisms of friction, lubrication, and wear of interacting surfaces that are in relative motion.1 Based on the similarities of biomechanical and mechanical systems, the premise for ensuring the efficiency and longevity of the components of the human movement system is maintaining precise movement of rotating segments. Although the adaptive and reparative properties of biological tissues permit greater leeway in maintaining their integrity than do nonbiologic materials, it is reasonable to assume that maintaining precise movement patterns to minimize abnormal stresses is highly desirable. A useful criterion for assessing precise or balanced movement is observing the path of instantaneous center of rotation (PICR) during active motion (Figure 2-3). The instantaneous center of rotation (ICR) is the point around which a rigid body rotates at a given instant of time.48 The PICR is the path of the ICR during movement. In many joints the PICR is not easily analyzed and radiologic methods are necessary to depict the precision of the motion (Figure 2-4). These radiologic methods use movements that are performed passively and under artificial conditions. The joints in which the PICR is difficult to observe clinically include those of the knee and spine. The PICR of the scapulothoracic (Figure 2-5) and glenohumeral (Figure 2-6) joints can be observed visually, but it cannot be easily quantified. Knowledge of the PICR and range of motion of the joint both guide observations and judgments about movement. Although it is rarely referred to specifically, the observation of the PICR is the guideline that physical therapists use to judge whether the joint motion is normal or abnormal. Anatomic and kinesiologic factors that determine the PICR and the pattern of joint movement are (1) the shape of joint surfaces, (2) the control by ligaments, and (3) the force-couple action of muscular synergists.73 With normal or ideal movement of joints, the question arises, “What is the cause of deviations in joint movement when a pathologic condition or specific injury is not the problem?” Suggested causes of deviations in joint movement patterns are repeated movements and sustained postures associated with daily activities of work and recreation. For example, baseball pitchers and swimmers perform repeated motions and commonly experience shoulder pain.16,31 Prolonged sitting has been cited as a factor in the development of back pain.52 Cyclists who spend 3 hours riding their bicycles in a position of lumbar flexion have a reduced lumbar curve when compared with control subjects who do not ride bicycles.10 Therapists and other clinicians involved in exercise prescription believe that repeated movements can be used therapeutically to produce desired increases in joint flexibility, muscle length, and muscle strength, as well as to train specific patterns of movement. All individuals who participate in exercise accept the fact that repeated movements affect muscle and movement performance. Thus these individuals should also accept the idea that repeated motions of daily activities, as well as those activities of fitness and sports, may also induce undesirable changes in the movement components. Stretching and strengthening exercises performed for shorter than 1 hour are believed to produce changes in muscular and connective tissues. However, repeated movements and sustained postures associated with everyday activities that are performed for many hours each day may eventually induce changes in the components of the movement system. The inevitable result is the development of movement impairments, tissue stress, microtrauma, and eventually macrotrauma. In accordance with this proposed theory, the effects of repeated movements and sustained postures modify the kinesiologic model so that it becomes a kinesiopathologic model (Figure 2-7), that is, a study of disorders of the movement system. If pain is present, the kinesiopathologic model can be used to identify all the contributing factors that must be addressed in a therapeutic exercise program. Reversal of the deleterious sequence requires the identification and correction of the movement and component impairments. More important than developing a therapeutic exercise program, the performance of functional activities that cause pain must be identified and corrected. Movements repeated at the extremes of frequency (either high or low) and movements that require the extremes of tension development (either high or low) can cause changes in muscle strength, length, and stiffness. Similarly, sustained postures and particularly those postures that are maintained in faulty alignments can induce changes in the muscles and supporting tissues that can be injurious, especially when the joint is at the end of its range.70 The following example illustrates how repeated movements can alter muscle performance and lead to movement impairments. When the gluteus maximus and piriformis muscles are the dominant muscles producing hip extension, their proximal attachments provide more optimal control of the femur in the acetabulum than do the hamstring muscles. The attachments of the piriformis and gluteus maximus muscles onto the greater trochanter and intertrochanteric line of the femur provide control of the proximal femur during hip extension. The gluteus maximus through the iliotibial band also attaches on the tibia distally. Therefore this muscle is producing movement of both the proximal and distal aspects of the thigh, which reinforces the maintenance of a relatively constant position of the femoral head in the acetabulum during hip extension (Figure 2-8). The normal pattern can become altered, particularly in distance runners who develop weakness of the iliopsoas and gluteus maximus muscles. In contrast, the tensor fascia lata (TFL), rectus femoris, and hamstring muscles often become stronger and more dominant in distance runners than in nonrunners. The lack of balance in the strength and pattern of activity among all the hip flexor and extensor muscles can contribute to movement impairments, because each muscle has a slightly different action on the joint to which it attaches. When one in the group becomes dominant, it alters the precision of the joint motion. In the scenario where the activity of the hamstring muscles is dominant and the gluteus maximus muscle is weak, the result can be hamstring strain and a variety of hip problems that are painful. One plausible reason hip joint motion becomes altered is that the hamstring muscles, with one exception, originate from the ischial tuberosity and insert into the tibia. (The exception is the short head of the biceps femoris muscle, which attaches distally on the femur.) Because the hamstring muscles, with the exception of the short head, do not attach into the femur, they cannot provide precise control of the movement of the proximal end of the femur during hip extension. When the hamstring muscular activity is dominant during hip extension, the proximal femur creates stress on the anterior joint capsule by anteriorly gliding during hip extension rather than maintaining a constant position in the acetabulum (see Figure 2-8). This situation can be exaggerated if the iliopsoas is stretched or weak and is not providing the normal restraint on the femoral head. These changes in dominance are not presumed; they are confirmed through manual muscle testing and careful monitoring of joint movement. Manual muscle testing32 is used to assess the relative strength of synergists and the identification of muscle imbalances. Carefully monitoring the precision of joint motion as indicated by the PICR is also necessary when the muscle imbalance has produced a movement impairment. For example, monitoring the greater trochanter during hip extension will identify which muscles are exerting the dominant effect. The greater trochanter will move anteriorly when the hamstrings are the dominant muscles. In contrast, the greater trochanter will either maintain a constant position or move slightly posteriorly when the gluteus maximus and piriformis muscles are the prime movers for hip extension. Muscular force is in proportion to the physiologic cross-sectional area.36 The physiologic cross-sectional area is a function of the number of contractile elements in the muscle (Figure 2-9). Muscle will atrophy, or lose contractile elements, when it is not routinely required to develop other than minimal tension. Conversely, the muscle cells hypertrophy when routinely required to develop large amounts of tension, as long as the tension demands are within the physiologic limit of its adaptive response. The change in size (circumference) of a muscle occurs either by a decrease in sarcomeres (atrophy) (Figure 2-10) or an increase in sarcomeres (hypertrophy) (Figure 2-11). In hypertrophy the addition of sarcomeres in parallel is accompanied by the addition of sarcomeres in series, though to a lesser extent than those added in parallel. The decreased number of sarcomeres and the decreased amount of connective tissue can affect both the active36 and passive9 tension of a muscle, which affects the dynamic and static support exerted on each joint it crosses. The effect is diminished capacity for the development of active torque and less stability of the joint controlled by the muscle. For example, if the peroneal muscles of the leg are weak, the motion of eversion will be weak and the passive stability that helps restrain inversion will be diminished. The passive tension of muscles also affects joint alignment. When the elbow flexor muscles are weak or have minimal passive tension, the elbow remains extended when the shoulder is in neutral. When the elbow flexors are hypertrophied from weight training, the resting position of the elbow joint is often one of flexion. Because atrophy means a deficiency of contractile elements, the size of a muscle (cross-sectional area) and its firmness can be used as guides to assess strength. For example, poor definition of the gluteal muscles is usually a good indication that these muscles are weak, particularly when the definition of the hamstring muscles suggests hypertrophy. Examiners should not rely solely on observation, but they should perform a manual muscle test to confirm or refute the hypothesis. Another example of altering the use of specific muscles is seen in the individual who returns to an upright position from a forward flexed position by swaying the hips forward rather than maintaining a relatively fixed position of the hips. The individual with the relatively fixed position of the hips lifts the length of the pelvis and trunk by extending the hips and back (Figure 2-12). Typically, individuals who sway their pelvis forward have weak gluteus maximus muscles. There are numerous ways in which slight subtleties in movement patterns contribute to specific muscle weaknesses. The relationship between altered movement patterns and specific muscle weaknesses requires that remediation addresses the changes to the movement pattern; the performance of strengthening exercises alone will not likely affect the timing and manner of recruitment during functional performance. To initiate the reversal of muscle atrophy, the patient’s ability to activate the muscle volitionally is augmented. Studies indicate that after 2 weeks of training, 20% of the change in muscle tension development can be attributed to muscular factors (contractile capacity) and 80% from enhanced neural activation.43 Training specific muscles is particularly important when the problem is an imbalance of synergists rather than generalized atrophy. Approximately 4 weeks of strengthening exercises are required to verify the morphologic increase in muscle cross-sectional area.43 Studies at the cellular level suggest that change may be occurring earlier than 4 weeks, which is consistent with the metabolic properties of other proteins. Because 4 weeks is required for changes in the number of contractile elements, early improvements in muscle performance are attributed to neuromotor recruitment. The rate of recruitment and the absolute frequency of activation of muscles are important factors in the performance of producing, improving, and maintaining the tension-generating properties of muscles. Strain can result from excessive stretching for short duration or excessive physiologic loading usually associated with eccentric contraction.35 (Additional discussion of the cellular manifestation of strain is found in the section on increased muscle length in this chapter.) Unless there is an actual tear of muscle fibers and obvious signs of hemorrhage, strain is not readily recognized as a source of muscle weakness. The intervention is different than when the muscle is strained and not merely atrophied. Studies have shown that when a muscle is subjected to overload conditions, the response is the addition of contractile and connective tissue proteins. The value of hypertrophy in increasing the tension-generating capability of muscle is well known and frequently used by those involved in rehabilitation and athletics. Less appreciated is the effect of hypertrophy on the passive-tension properties of muscle and other connective tissue. Many tissues respond to stress by adapting (see Figure 2-11), which for muscle is hypertrophy. The quantity of connective tissue proteins of ligaments, tendons, and muscle also increases with hypertrophy. Tendons and ligaments become stronger and stiffer when subjected to stress, but they grow weaker when they are not subjected to stress.64,67,72 The result is an increase in the passive tension of these tissues, not just the active tension that is generated by muscle during contraction. (The cellular factors are described in the section on muscle stiffness in this chapter.) A muscle can become lengthened by one of the following three mechanisms: 1. Prolonged elongated position. Muscle may remain in an elongated position during a prolonged period (hours or days) of rest or inactivity (e.g., elongation of the ankle dorsiflexors by the tension of bed covers during bed rest). This condition is similar to over-stretch weakness and a mild form of strain that does not involve eccentric contraction under load as described by Kendall.32 2. Injurious strain. Muscle may be subjected to injurious strain, which is the disruption of the cross bridges, usually in response to a forceful eccentric contraction. The muscle may then be subjected to continuous tension. 3. Sustained stretching. Muscle may respond to sustained (many days to weeks) stretching during immobilization in a lengthened position with the addition of sarcomeres in series.71 Another example is the prolonged stretch of the posterior gluteus medius that occurs while sleeping. This condition is seen particularly in the woman with a broad pelvis who regularly sleeps on her side with her uppermost leg positioned in adduction, flexion, and medial rotation. During manual muscle testing, this patient is unable to maintain the hip in abduction, extension, and lateral rotation—the testing position—or at any point in the range, as the resistance is continually applied by the examiner. The resultant lengthening of the muscle can produce postural hip adduction or an apparent leg length discrepancy when the patient stands. There are several characteristics of muscles with over-stretch weakness: 1. Postural alignment that is controlled by the muscle indicates that the muscle is longer than ideal, as in depressed shoulders or in a postural alignment of the hip of adduction and medial rotation. 2. Muscle tests weak throughout its range of motion and not only in the shortened muscle test position. History.: 20-year-old female college student has developed back pain that is partially attributable to working as a waitress. Radiologic studies indicate she has a C-curve of her lumbar spine with a right convexity. Her left iliac crest is 1 inch higher than her right, and she stands with a marked anterior pelvic tilt. Symptoms.: The patient complains that her slacks are not fitting correctly. Although she is slender, the patient has a very broad pelvis. She sleeps on her right side with her left leg positioned in hip flexion, adduction, and medial rotation. Muscle Length and Strength.: Muscle length testing indicates a shortened left TFL. Manual muscle testing indicates that the posterior portion of her left gluteus medius muscle is weak, grading 3+/5. Her external oblique abdominal muscles also test weak, grading 3+/5. In the side-lying position, her left hip adducts 25 degrees and rotates medially to the extent that the patella faces the plinth. A home exercise program that emphasizes strengthening her posterior gluteus medius muscle in the shortened position is prescribed. In the supine position with her hips and knees flexed, she performs isometric contraction of her external oblique abdominal muscles while maintaining a neutral tilt of her pelvis. She then extends one lower extremity at a time. The position for hip flexor length testing is used to stretch the TFL. She also performs knee flexion and hip lateral rotation in the prone position. She is instructed to stand with her hips level and to contract her external oblique abdominal and gluteal muscles. She is also asked to use a body pillow to support her left leg while sleeping to prevent the adduction and medial rotation of her left hip when lying on her right side. Outcome.: On her second visit 3 weeks later, the patient’s symptoms have greatly improved to only an occasional incident of discomfort. Her iliac crests are level, and her spinal lateral curvature is no longer clinically evident. The anterior pelvic tilt has resolved. She states she no longer has back pain. Increased Muscle Length Secondary to Strain Strain is discussed because of the importance of differentiating whether the cause of muscle pain is muscle shortness or excessive muscle length. A common approach to the treatment of painful muscles, particularly those of the shoulder girdle, is applying a cold spray and stretching the muscle.60 Pain is attributed to spasm in the shortened muscle,60 but often the actual length of the muscle is not assessed before applying stretching techniques. Lengthened muscles can also become painful and should not be stretched. For example, when a muscle is subjected to injurious tension by lifting a heavy object, it can become strained. If the muscle remains under continuous tension, it will become elongated and painful. When the postural alignment examination indicates a muscle is elongated, then strain, rather than shortness, is considered the likely cause of pain. Strain is a minor form of a tear in which the filaments of the muscle have been stretched or stressed beyond their physiologic limit resulting in disruption of the Z-lines to which the actin filaments attach (Figure 2-13). Disruptions that alter the alignment of the myofilaments interfere with the tension-generating ability of these contractile elements.35 The consequence is muscular weakness and, in many cases, pain when the muscle is palpated or when resistance is applied during contraction of the muscle. History.: A 32-year-old woman, whose job requires her to load food trays on a conveyor belt at shoulder height, has a sudden and severe onset of pain between the vertebral border of the right scapula and thoracic spine. The pain began after she attempted to lift a filing cabinet at work. She is seen immediately by a physician who refers her to a physical therapist, prescribing heat to the affected area and shoulder exercises three times a week. After 1 week, the patient returns to light duty at work, but 6 weeks later she still complains of severe pain and she is unable to return to her normal job. A magnetic resonance image of her thoracic spine does not indicate an abnormality. Symptoms.: She is referred to a second physical therapy clinic. During her initial visit the patient is observed to be approximately 60 pounds overweight, with large arms and breasts and deep indentations on the tops of her shoulders from the pressure of her bra straps. Her facial expression and the manner in which she holds her right arm close to her body with her elbow flexed indicate that she is still in pain. She rates her pain as 6 to 8 on a scale of 10 when attempting any type of shoulder motion and 4 to 5 out of 10 with her arm at rest. (The 10 rating is the most severe.) Muscle Length and Strength.: An examination indicates that the right scapula is greatly abducted and tilted anteriorly (Figure 2-14, A). Her scapula is manually positioned in the correct alignment, and her arm and forearm are supported by the physical therapist. After she is instructed to relax the musculature of her right shoulder girdle, she reports her pain has subsided (Figure 2-14, B). A manual muscle test indicates the strength of all components of her trapezius muscle as weak, graded 3—/5. Weakness and pain limit her ability to move through the normal range of motion even in a gravity-lessened position. Tape (Leukotape P with cover roll underwrap) is applied to the posterior aspect of the right shoulder girdle to support and maintain the scapula in a neutral position and to reduce some of the strain on the trapezius muscle by decreasing the abduction and depression of the scapula. The case report written by Host demonstrates that scapular position can be altered by the application of tape to the posterior shoulder girdle.28 Her bra straps are taped together, bringing them closer to her neck to reduce the downward pull on the lateral aspect of her shoulders. She is also instructed to support her arms on pillows whenever she sits and to support her right arm with her left arm to reduce the downward pull on her shoulder girdle whenever she stands. All shoulder exercises are eliminated for the next 5 days (Figure 2-14, C). Outcome.: On her second visit 4 days later, the patient reports a significant decrease in pain. She has kept her shoulder taped for 2 days. Her skin does not show signs of irritation, and she indicates that the extra support has eliminated her pain at rest. As a result, the tape was reapplied. On her third visit 1 week later, the patient no longer complains of pain at rest, and she can perform 160 degrees of shoulder flexion without pain in the gravity-lessened side-lying position with her arm supported on pillows. In this position the scapula rotates upwardly and adducts during shoulder flexion, in contrast to the limited scapular motion observed during the same movement performed in the standing position. Her shoulder girdle is taped to support the scapula in the neutral position relative to abduction or adduction, elevation or depression, and rotation. The tape remains in place for 2 additional days. She has been taped three times over a 2-week period. 1. Gravity-lessened side-lying shoulder flexion 2. Shoulder flexion facing a wall with her elbow flexed and hand gliding up the wall 3. Shoulder flexion with the elbow extended 4. Shoulder flexion and abduction while lifting light weights Lengthened Muscle Secondary to Anatomic Adaptation—the Addition of Sarcomeres Numerous investigators have demonstrated that when a muscle is maintained in a position of elongation (usually by casting), additional sarcomeres are added in series within the muscle cell. A study by Williams and Goldspink60,72 demonstrates that when such adaptation of the anatomic length occurs, the muscle’s length tension curve is shifted to the right because of the addition of sarcomeres in series.71 However, with both muscles in the same shortened position, the control muscle develops greater tension than the lengthened muscle (Figure 2-15).
Concepts and Principles of Movement
Kinesiologic Model
Clinical Relevance of the Model
Pathokinesiologic Model
Clinical Relevance of the Model
Kinesiopathologic Model
Clinical Relevance of the Model
Base Element Impairments of the Muscular System
Decreased Muscle Strength Caused by Atrophy
Clinical Relevance of Muscle Atrophy
Decreased Muscle Strength Secondary to Strain
Increased Muscle Strength Caused by Hypertrophy
Muscle Length
Over-Stretch Weakness
Case Presentation 1
Case Presentation 2
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Concepts and Principles of Movement