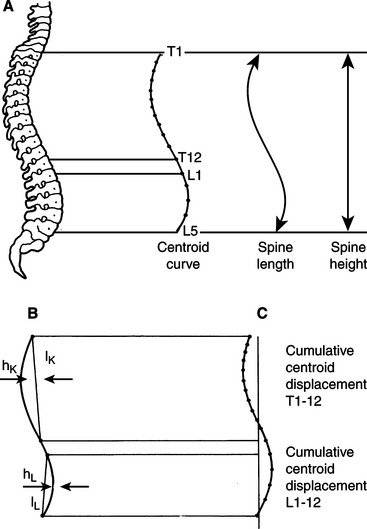
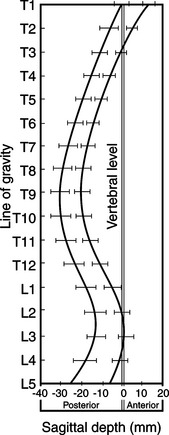
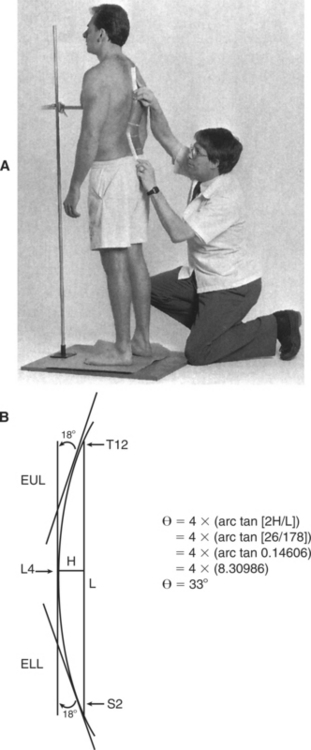
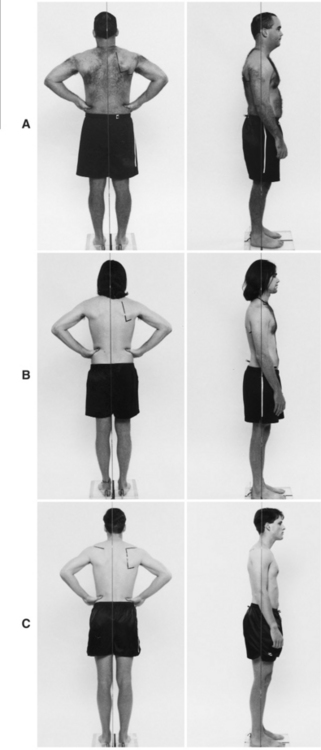
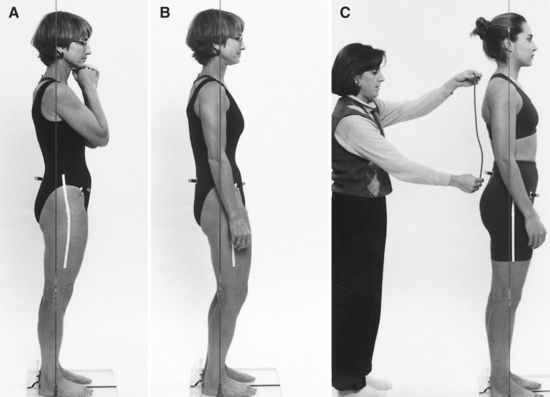
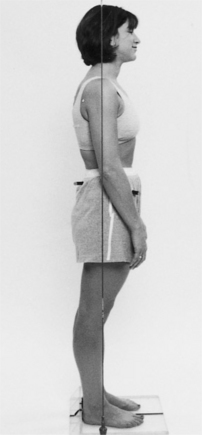
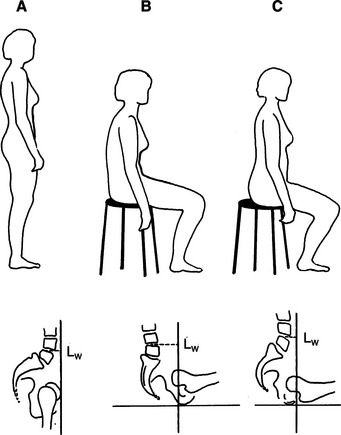
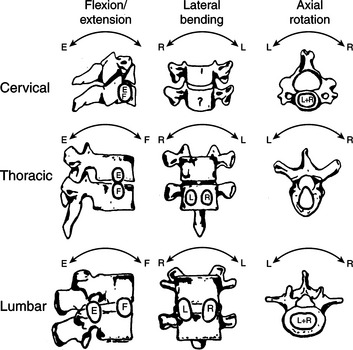
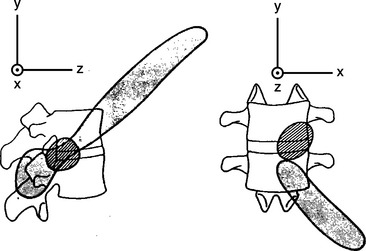
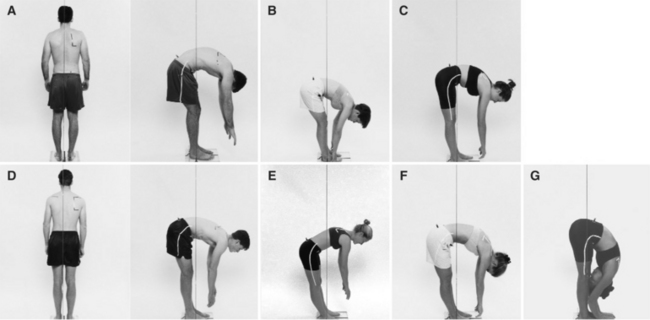
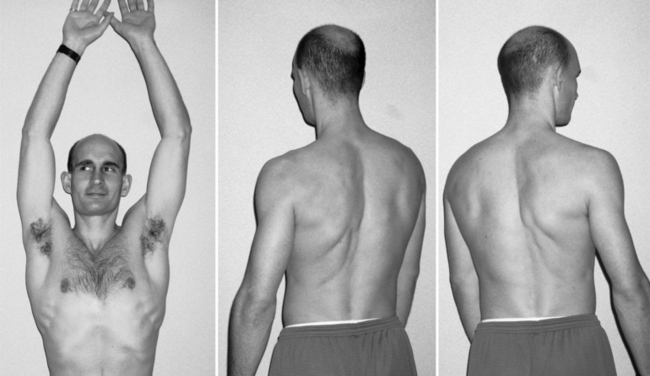
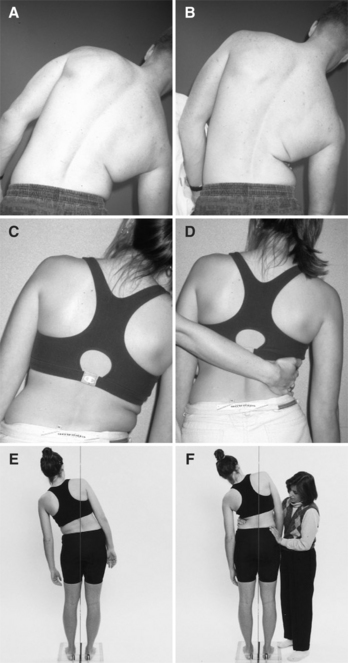
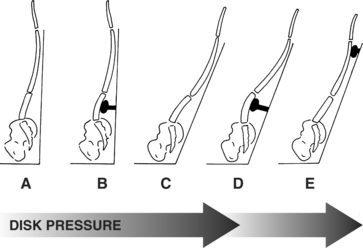
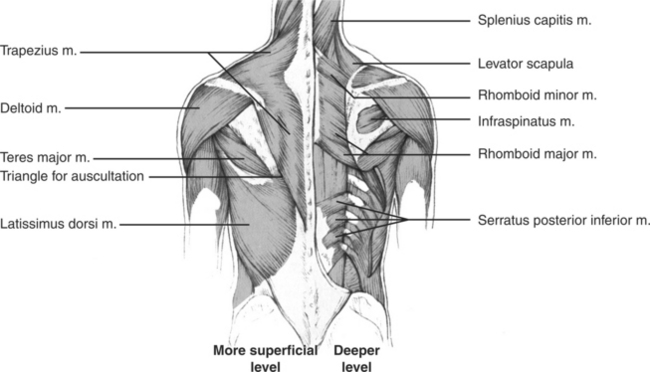
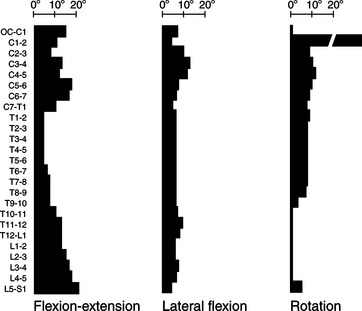
Chapter Three After consideration of the information presented in this chapter, the reader will be able to: 1 Describe the standards for ideal alignment and identify structural variations of the spine and pelvis. 2 Describe the standards for the normal ranges of the motions of the spine. 3 Identify the contributions of each abdominal muscle to the movements and to the stability of the trunk and pelvis and prescribe appropriate exercises. 4 Understand the characteristics of each movement impairment syndrome of the low back. 5 Perform an examination of the patient with low back pain, consider the contributing factors, and establish a diagnosis. 6 Develop and instruct the patient in a diagnosis-specific intervention program of exercise and modification of life activities, which contributed to formation of the movement impairment syndrome. The keys to preventing and alleviating spinal dysfunction are (1) to have the trunk muscles hold the vertebral column and pelvis in their optimal alignments and (2) to prevent unnecessary movement. To achieve these goals, the muscles must be the correct length and strength and be able to produce the correct pattern of activity. During movement of the extremities, optimal isometric contraction of the trunk muscles is needed to appropriately stabilize the proximal attachments of the limb muscles. A forward convex curve of the lumbar spine is the normal or neutral position. A study of 14- to 15-year-old adolescents, using an estimation of vertebral bodies from the external profile of the spine in the sagittal plane, calculates the lumbar curve from the vertebral centroid curve. Male adolescents have a curve of 25.6 degrees, and female adolescents have a curve of 30.8 degrees.45 The curvatures calculated from vertebral centroids located on the bodies of the vertebrae are expected to differ from those observed from external landmarks, such as the spinous processes (Figures 3-1 and 3-2). Inclinometers and flexible rulers can be used to measure external lumbar curves. Because two different methods are used to calculate the curve obtained by these devices, there is some variation in the reported values. The study by Youdas uses a flexible ruler to measure the lumbar curve of five men and five women with a mean age of 25 years. This study reports values ranging from 21 to 49 degrees and a mean value of approximately 34 degrees using both tangent and trigonometric methods to calculate the curves59 (Figure 3-3). Thus a general assumption can be made—the lumbar curve in young individuals ranges from 25 to 30 degrees. Ohlen and colleagues use an inclinometer as their measurement device. Their study reports that the thoracic curve ranges from 30 to 33 degrees.41 Loebl also uses an inclinometer to measure the thoracic spine. He reports similar values of 32 to 37 degrees for the individual younger than 40 years and values of 40 to 41 degrees for the individual older than 60 years.29 Acquired impairments in the sagittal plane are either a decreased lumbar curvature resulting in a flat back or an increased lumbar curvature resulting in a lordosis. Judging the depth of the lumbar curve is not always easy. The reference for the ideal curve is provided in Figure 3-4, and an example of good lumbopelvic alignment is shown in Figure 3-5. The lumbar curve is affected by the tilt of the pelvis. A correlational between the lumbar curve and pelvic tilt has not been shown, nor should one be expected for both statistical and anatomical reasons. However, as demonstrated, tilting the pelvis anteriorly increases the lumbar curve, whereas tilting the pelvis posteriorly decreases the lumbar curve (Figure 3-6 on page 55). Lumbopelvic alignment is often used for clinical assessment of the patient with lower quarter pain, but the measures used for this assessment can be misleading. Typically, the following three different measures are used to assess lumbopelvic alignment: (1) the lumbar curve, (2) the deviation from the horizontal line between the posterior superior iliac spine (PSIS) and anterior superior iliac spine (ASIS), and (3) the hip joint angle. Examples of each measure can vary because of factors other than acquired impairments in lumbopelvic alignment. For example, a man often has structural variations in the curvature of his lumbar spine in the standing position. When the iliac crest is obviously higher than his belt line, he will consistently have a flat lumbar spine (Figure 3-7 on page 56). This patient is not standing in a posterior pelvic tilt because his PSIS is not lower than his ASIS and his hips are not in extension, which would be the finding if his flat lumbar spine had been an acquired impairment of posterior pelvic tilt. Often this patient also has retrotorsion of the hips. When the patient has a flat lumbar spine, the flexibility of the hips becomes particularly important. During forward bending, the individual with a flat lumbar spine must immediately flex the hips to avoid excessive flexion of the spine (Figure 3-8 on page 56). A tall man with relatively greater pelvic height to overall height is more prone to low back pain than the tall man who does not have a tall pelvis.36 Structural factors can also influence the measurement of the line between the PSIS and ASIS. In women the structure of the pelvis can vary dramatically. In some the ASIS is notably lower than the PSIS; however, the pelvis is not tilted anteriorly, the hip is not flexed, and the lumbar spine is not lordotic (Figure 3-9 on page 57). The hip joint angle is affected by the knee joint angle and by the pelvic tilt. When the knees are hyperextended, the hip joint is extended even though the pelvic tilt may be ideal (Figure 3-10 on page 57). Thus the assessment of lumbopelvic alignment should be based on a positive finding of two out of the three measurements. Symmetry of the lumbar paraspinal area is another alignment impairment that is particularly important in the patient with low back pain. A side-to-side difference of ½ inch or greater, which a trained therapist can reliably detect, is one of the tests used for the rotation category.54 Asymmetry can be attributed to either postural rotation of the lumbar spine to one side or to unilateral hypertrophy of the paraspinal muscles. (The movement tests that differentiate these two conditions are described in the section on motions of the lumbar spine.) In the normal sitting position, the pelvis posteriorly tilts relative to the standing position. As a result, the lumbar spine reverses its anterior curve and becomes flat (Figure 3-11 on page 58). When the spine becomes flat, increased pressure is exerted on the disks because the pressure is reduced on the facet joints, as compared with the pressure exerted on the disks in the standing position.39 If the inward curvature of the lumbar spine is increased while the patient is in a sitting position, the pressure on the disks decreases, but it is not as low as when the patient is in a standing position. Another subtle yet common impairment is the tendency for a person to sit leaning to one side, often leaning onto an arm rest that is too low for the trunk height or the length of the arms. This position of lateral flexion can contribute to back pain, particularly in the individual whose lumbar spinal movement is isolated to only one or two lower segments of the lumbar spine. In summary, sitting impairments include a number of alignment faults other than lumbar flexion. Ideally, the patient should sit all the way back in the chair to use the back support. The shoulders should be in line with the lumbar spine, and the hips should be at a 90-degree angle with the knees in the same horizontal plane as the hips. If the feet do not reach the floor, they should rest on a footstool. The patient should not lean to one side. Accommodation must be made for structural variations such as long tibias, short legs, large abdomen, large buttocks, and thoracic kyphosis. A patient may magnify his or her complaints by simply contracting the proximal thigh muscles while sitting. For example, a woman may hold her knees together when sitting, another individual may subconsciously arch the back when tense, and another may contract the hamstring muscles, which can tilt the pelvis posteriorly. Path of the Instant Center of Rotation As with movement of the limb joints, the motion between the surfaces of the adjacent bones of the spine are analyzed by determining the path of the instant center of rotation (PICR). The location of the PICR has been determined for the different motions of the spine and is shown in Figure 3-12. For flexion and extension, the axis of rotation lies in the posterior half of the disk. The location of the PICR is used to calculate the moment exerted by muscle fascicles on the lumbar spine.2 The degree of flexibility of the spine suggests that changes in the vertebral alignment may affect the location of the PICR and therefore affect the moments exerted by the different muscles. Such changes have not been reported, but the possibility exists. These changes may have important clinical implications. The alteration in the action of the sternocleidomastoid muscle from a cervical flexor (i.e., when the intrinsic neck flexors are contracting) to a cervical extensor (i.e., when the intrinsic neck flexors are not contracting) is one example of how changes in the alignment and stabilizing function of a synergistic muscle have important clinical consequences. An alteration in the PICR is associated with degeneration of the disks (Figure 3-13); this finding should be considered when developing exercise programs for the patient with low back pain. As discussed in Chapter 2, the alteration in the PICR is associated with changes in the surface motion of the two articulating segments, causing compression or distraction to occur during the motion. Compression or distraction may be a source of continued trauma to the joint. In the presence of disk degeneration, the patient should be instructed to perform exercises that limit the motion of the spine, rather than promote increased movement. Woolsey and Norton have analyzed the studies in which the lumbar range of motion is measured with an inclinometer.58 Based on their analysis, the mean range of motion of lumbar flexion is 56.6 degrees.58 The lumbar spine should not complete more than 50% of its motion into flexion before hip flexion is initiated.40 At the completion of flexion there should be a straightening or flattening of the lumbar spine. The straight spine is described as flat rather than flexed.27 The final degrees of lumbar flexion is even more important than the range of motion of the lumbar spine. Studies using inclinometers positioned over L1 (with the appropriate subtraction of the number of degrees of hip flexion) indicate an average final flexed position between 20 and 25 degrees.10 The final degree of lumbar flexion curvature is a more important value than the range of motion, because initial alignment is a major factor in the range-of-motion measurement. The range-of-motion value is based on the lumbar spine aligned at the starting position in approximately 20 to 30 degrees of extension. Consequently, when the range of motion is 50 degrees, the lumbar spine reaches a maximum flexion curvature of 20 degrees. In the patient with a flat back, a lumbar alignment in standing of 0 degrees and the same total range of motion of 50 degrees are both dangerous. There are two important questions to ask. 1. Is the lumbar spine reversing its curve and becoming flat? 2. Is the lumbar spine flexing beyond the optimal anatomic limits and therefore excessively stretching the posterior supporting tissues? In addition to the issues of total range of motion of the lumbar spine and maximal degree of lumbar flexion is the motion of each vertebral segment. White and Panjabi report the flexion-extension range between the vertebral segments is approximately 4 degrees in the upper thoracic spine, 6 degrees in the midthoracic spine, and 12 degrees in the lower thoracic spine. The motion between the vertebral segments in the upper lumbar spine is approximately 12 degrees, and then it increases approximately 1 degree for each lower segment, reaching the maximum range of motion of 20 degrees between L5 and S156 (Figure 3-14). In maximum flexion, the erector spinae muscles become inactive, and thus the stress is on the passive elements of the muscles and ligaments.14 Approximately 20 minutes of stretching at the end of flexion increases the range by 5 degrees, which is attributed to the creep properties of the soft tissues. Approximately 50% of the original stiffness is recovered within 2 minutes after resuming normal alignment. However, longer than 30 minutes is required to recover the normal amount of soft-tissue stiffness.31 These findings support the concept that sustained positions can alter the properties of soft tissues and can become contributing factors to altered alignment. A final flexed position greater than 25 to 30 degrees is excessive lumbar flexion. Also considered an impairment is lumbar flexion greater than 50% of its total range before any amount of hip flexion is observed. Esola and associates report that subjects with low back pain move more in the lumbar spine than at the hips during the 30- to 60-degree phase of forward bending.12 Another factor contributing to mechanical low back pain is the failure of all segments to maintain their contribution to motion. When failing to do so, the consequence of such failure is that the other segments move more than their optimal range of motion (Figure 3-15). Because of these compensatory motions, exercises must be carefully performed, ensuring against some segments becoming hypermobile while others remain hypomobile. Based on the concept of relative flexibility, which proposes that the least stiff segment moves more readily than stiffer segments, developing a program that improves the mobility of restricted segments in the multisegmental spine is a challenge. Even when the stiffest segment is passively moved, for that movement to occur during activity, the segment has to move as easily as the most flexible segment. Alignments at the end of the forward bending motion are illustrated in Figure 3-16. Typically, men tend to flex more readily in the lumbar spine, and women flex more easily in the hips. In a study by Thomas and associates,51 subjects in a standing position are asked to perform two reaching tasks using two different target heights. Men move more in the spine than in the hips (spine/hip ratio is 1:20) and women move more in the hips than the spine (spine/hip ratio is 0:20). These ratios are not end-range motions, but they demonstrate that initial movement patterns vary and can be sex specific. The report of these movement patterns supports the belief that patients need to be retrained to move correctly and that these sites of movement are not determined by reaching the limits of a muscle’s length. The return from forward bending can also be a factor in the patient’s pain. As with forward bending, a variety of strategies are used. During the return from forward bending, ideally the initial part of the motion should be hip extension, and then both the hips and spine should concurrently continue their extension motions until the patient is in the upright position (see Figure 2-12). Because the range of hip motion is 70 to 80 degrees and the range of the lumbar motion averages between 30 to 50 degrees, the hips move more than the spine. The motions should be smooth and relatively concurrent versus consecutive, other than during the initiation of the motion with hip extension. With the motion initiated at the lumbar spine or immediately after a short period of hip extension, the return from forward bending is an impairment found in some patients who have pain caused by extension (see Figure 2-12). This type of motion increases the compressive forces on the spine.34 When a patient with low back pain demonstrates this type of motion, he or she often performs daily activities with only a few degrees of repeated lumbar flexion and extension motions. The movements are confined to the lumbar spine instead of the hip joints, which should be the site of motion. Extension of the lumbar spine is an increase in the anterior curve. According to Kendall, the range is highly variable; consequently, a standard for reference measurement is difficult to establish.27 The reported value for the maximum lumbar extension curve is approximately 50 degrees.59 When considering functional activities, there is not a demand for a large range of motion into extension. The problems arising from impairments of the lumbar spine stem more from excessive extension stresses that are focused on one or two spinal segments than from the lack of range of motion. The back extensor muscles, which restrain lumbar flexion, are located on the posterior aspect of the spine. In contrast, the abdominal muscles, which restrain lumbar extension, are located on the anterior surface of the abdomen. The location of the abdominal muscles is much further away from the site of the motion than that of the back extensor muscles. Studies on the spinal motion segment and the adjoining vertebrae and interposed disk have shown that the spinous processes, disks, and apophyseal joints are primary restraints to hyperextension.1 Hyperextension, like hyperflexion, damages the interspinous ligaments and can cause sudden disk prolapse and long-term structural damage to the disks.1 Although the anterior longitudinal ligament is not considered strong enough to resist large extension forces,52 anatomically it should contribute to the prevention of an extension alignment of the lumbar spine. As the disks degenerate, the anterior longitudinal ligament is no longer pulled as taut as when the disks are at full height, thus compromising the extension restraint from this ligament. Spinal stenosis is relatively common in the individual older than the age of 65 and is another example of a problem associated with lumbar extension. Even without structural changes in the spine, extension movements significantly decrease the central canal area and the midsagittal and subarticular sagittal diameters, whereas flexion has the opposite effect.23 These findings support the concept of dynamic stenosis, in addition to the well-accepted concept of static stenosis caused by degenerative and hypertrophic structural changes. The repeated hyperextension performed by gymnasts is cited as a cause of low back pain41,42 and spondylolysis.24 Active back extension, in particular, and, to a lesser extent, simultaneous shoulder and hip extension performed in the quadruped position cause high levels of compression forces.5 When the abdominal muscles are taut, limiting the excursion of the thoracic spine, the extension movement primarily occurs in the lower lumbar spinal segments rather than throughout all of the lumbar segments. The overall range of lumbar rotation is calculated to be approximately 13 degrees. The rotation between each vertebral segment from T10 to L5 is 2 degrees. The greatest rotational range is between L5 and S1, which is 5 degrees (see Figure 3-14). The vertical orientation in the transverse plane and the 45-degree angle orientation in the frontal plane of the facet joints are the reasons for limiting the rotational range in the lumbar spine.56 In contrast, greater range of rotation at the lumbosacral joint is possible because of the oblique orientation of its facet joints.30 The thoracic spine, not the lumbar spine, should be the site of the greatest amount of rotation of the trunk. When an individual practices rotational exercises, he or she should be directed to “think about the motion occurring in the area of the chest” and not the waist. Stiffness or shortness of the oblique abdominal muscles restricts the rotational motion (Figure 3-17). Some patients with low back pain have asymmetry in the appearance of the lumbar paraspinal muscles, which can be reliably detected if the side-by-side difference is ½ inch or greater.54 Asymmetry is attributed to either a postural rotation of the lumbar spine to one side or a greater bulk of the paraspinal muscles on one side. When differential muscle development causes the asymmetry, lateral flexion to the side opposite the larger muscle is more limited than lateral flexion toward the same side. The reason for this asymmetry in motion is the greater stiffness of the larger muscle. If the paraspinal asymmetry is the result of postural rotation, the lateral flexion movement pattern is restricted range of motion to the same side as the asymmetry and normal range of motion to the opposite side. Studies by Pearcy show that the greatest amount of rotation occurs when an individual is in a sitting position and the lumbar spine is flexed and the supporting tissues are relaxed.43,44 Rotational ranges of 3½ degrees have been shown to tear the annulus of the disk.43,44 Based on clinical observations, one of the greatest contributors to excessive rotation of the lumbar spine is repetitive rotational motion while sitting at a desk. Many individuals rotate the trunk to get to a computer, to answer the telephone, to open file drawers, or to reach an adjacent counter. In the sitting position the lumbosacral junction is most vulnerable to repeated stretching by the rotational activities. Sports, such as golf, racquetball, and squash, are the most common contributors to excessive rotation of the lumbar spine, particularly because the feet are planted during the motion. Tennis and volleyball do not contribute as much to rotational problems because the feet are not fixed at the time of rotation and the whole body is used in the follow-through motion. Rotation of the pelvis precipitating rotation at the lumbosacral joints is another factor. When muscles such as the tensor fascia lata (TFL) or other hip flexors become short, the restraint for hip extension imposed by these muscles often causes compensatory pelvic rotation during the stance phase of gait. The rotation of the pelvis causes motion to occur at the lumbosacral junction and not throughout the thoracic spine, as should occur during gait. Unilateral shortness of the TFL muscle can be a particularly important contributor to excessive pelvic rotation because of its hip medial rotation and flexion action. When the TFL is short, it can act as a major source of restraint to both hip extension and lateral rotation during the stance phase of gait. The range of motion of lateral flexion or side-bending range is reported to be greatest (8 to 9 degrees) in the lower thoracic segments because they are not restricted by the ribs. The average degrees of lateral flexion for the other thoracic segments and for the lumbar vertebrae is 6, except for the lumbosacral segment, which has only 3 degrees of lateral flexion.56 Lateral flexion is associated with rotation of the lumbar vertebrae toward the convexity of the curve. With lateral flexion occurring to the right, the rotation of the lumbar vertebrae is to the left. In the thoracic spine, the coupled motion causes rotation of the vertebrae toward the side of the concavity.57 Based on 6 degrees of motion at each lumbar segment, the total motion from L1 to S1 is 27 degrees. Although limited by the ribs, the thoracic lateral flexion has a potential greater than 75 degrees, depending on the number of vertebral segments of the thoracic spine, participating in the motion. Another sign of lateral flexion impairment is evident when, during the motion, the lumbar spine appears straight with an axis of rotation at only one segment rather than a relatively smooth curve throughout the entire lumbar spine. Most often this type of motion occurs at the lower lumbar segments in the individual who has well-developed lumbar paraspinal muscles. One explanation is that the stiffness of the hypertrophied paraspinal muscles restricts the excursion of these muscles; consequently, motion occurs at the interface of the musculotendinous junction, which is at approximately L4-5 and S1. Support of this hypothesis is found when resistance is applied to the lateral trunk at the level of the lower lumbar segments on the side to which the lateral flexion is performed. With support preventing the motion at the lowest lumbar segments, the lumbar spine demonstrates a lateral curve rather than a straight line. The explanation is that the paraspinal muscles are stiffer than the musculotendinous junction. Rather than allow the motion to occur at the site of least resistance, blocking this site forces the paraspinal muscles to stretch, allowing motion to occur at the other lumbar segments (Figure 3-18, A and B). Some patients are unable to flex laterally when motion is prevented at the lumbosacral junction (Figure 3-18, C–F). Although compression is not a motion of the lumbar spine, compression forces are altered by muscle position and contraction, as well as during changes in position and during activities such as carrying objects. When the disk is normal, the vertebral body or endplate will fracture before the disk is damaged11; however, when the disk is degenerated or damaged, compression is an important contributing factor to the patient’s symptoms. For example, a patient may have radiating symptoms when sitting but not when recumbent, standing, or walking. Further, when he or she sits in lumbar extension, the symptoms are often eliminated. Sitting with an increased curve decreases the compression on the disk because part of the force is distributed to the facet joints (Figure 3-19). The facet joints share 30% of the total load when the spine is hyperextended.28 Compression is less when the patient is recumbent, standing, and walking than when sitting. Walking at a fast rate can increase the compressive load to 2.5 times the body weight on the spine at L3-4, whereas walking at a slow rate keeps the compressive load close to body weight.6 The alignment of the spine affects the forces on the spine and the degree of muscular activity. The movements of the spine are complex and multidirectional, even when motion seems to be occurring in a specific direction. Because movements of the spine involve multiple segments, it becomes difficult to both assess the dysfunction and develop exercise programs that will ensure optimal participation of each segment in the motion. As stated by Nordin, “Restriction of motion of one part of the spine causes increased motion of another part of the spine.”39 It is difficult to develop exercise programs that will provide stability of the spine, prevent compensatory motions, and improve the strength and control of the trunk musculature without causing undesirable compressive or shear forces or without contributing to malalignment of the spine. Correction of subtle malalignments, compensatory motions, or stress imposed on the spine, particularly when localized to a few segments by daily activities, is the key to remediation of mechanical low back pain. Therefore the therapist must become proficient at observing the subtle deviations in movement patterns at specific segments and must not simply focus on overall excursions of motion. The latissimus dorsi is the most superficial of the back muscles and has a broad attachment through the thoracolumbar fascia from the lower six thoracic spinous processes, all of the lumbar spinous processes and sacrum, and the iliac crest. The fibers then converge superiorly and laterally to attach to the humerus (Figure 3-20). The thoracolumbar fascial attachment of the latissimus dorsi muscle provides the mechanism for this muscle to affect the lumbopelvic alignment. Contraction of the latissimus dorsi muscle creates an extension force on the spine and tilts the pelvis anteriorly. If the muscle is short, the back extends as a compensatory movement when shoulder flexion stretches the muscle to the limits of its length. Consistent with the concept of relative flexibility, if the latissimus dorsi is stiffer than the abdominal muscles, which limit lumbar extension, the back extends when the latissimus dorsi stretches, even when the muscle is not short. In the patient with low back pain that occurs with extension, the shortness or stiffness of this muscle contributes to pain when he or she reaches over head.
Movement Impairment Syndromes of the Lumbar Spine
Introduction
Normal Alignment of the Lumbar Spine
Normal Position
Impairments
Sitting
Impairments
Motions of the Lumbar Spine
Flexion: Forward Bending
JB Lippincott
Impairments
Return from Flexion
Impairments
Extension
Impairments
Rotation
Impairments
Lateral Flexion or Side Bending
Impairments
Compression
Summary
Muscular Actions of the Lumbar Spine
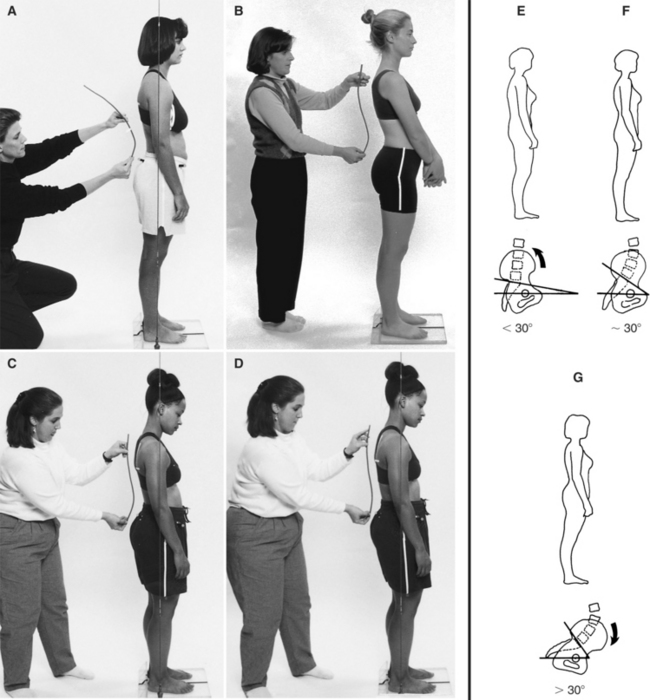
Latissimus Dorsi
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Movement Impairment Syndromes of the Lumbar Spine