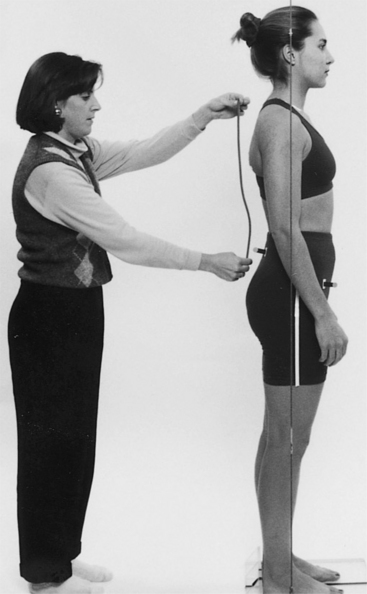
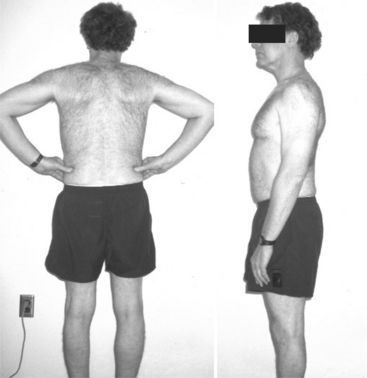
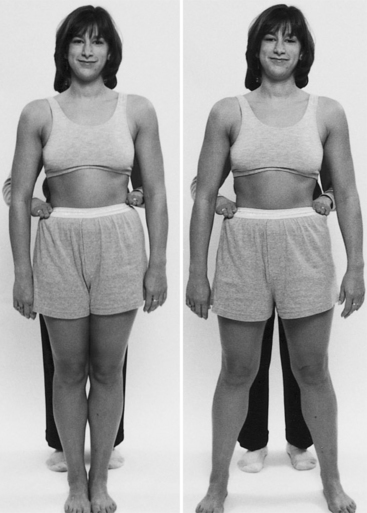
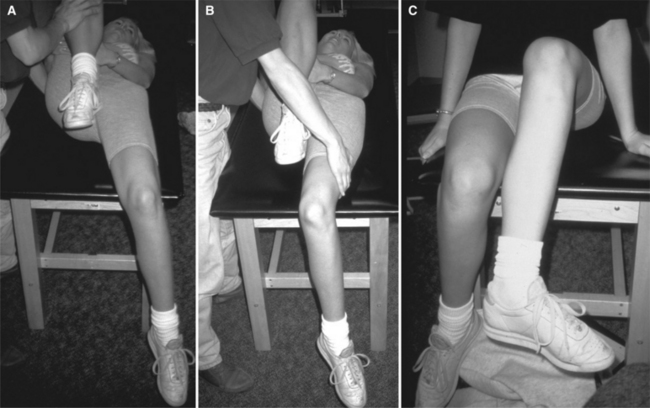
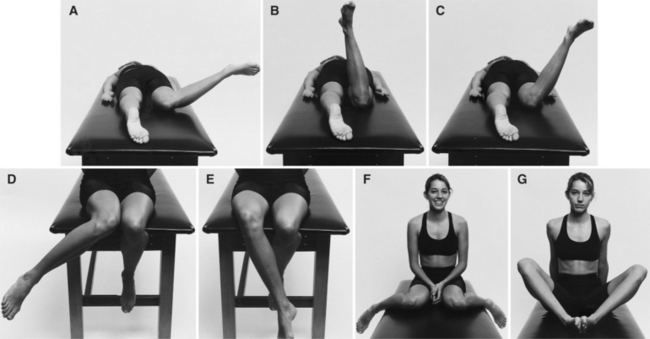
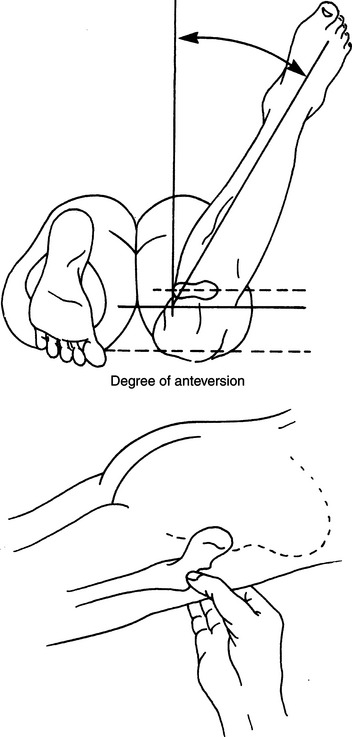
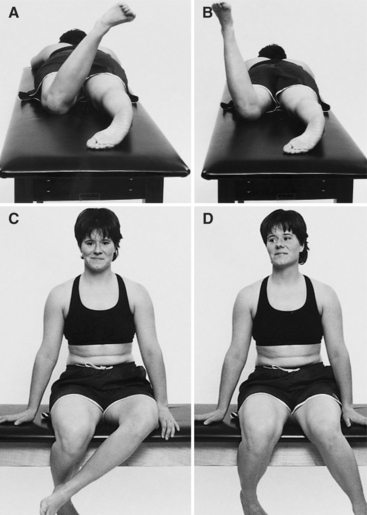
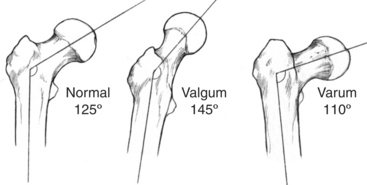
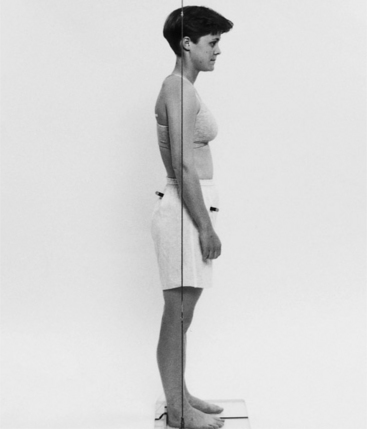
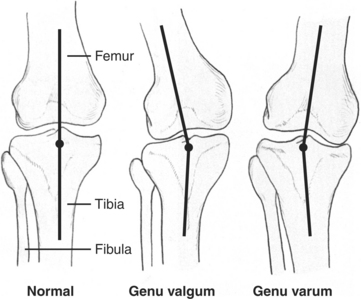
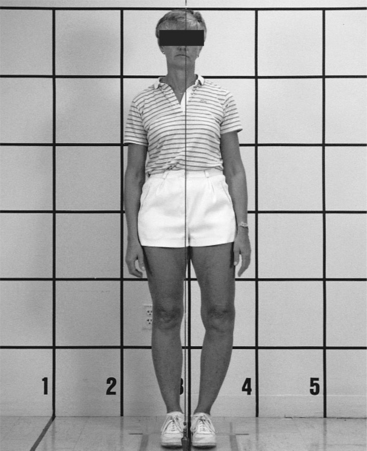
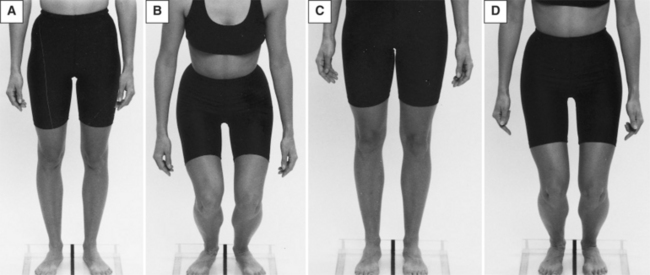
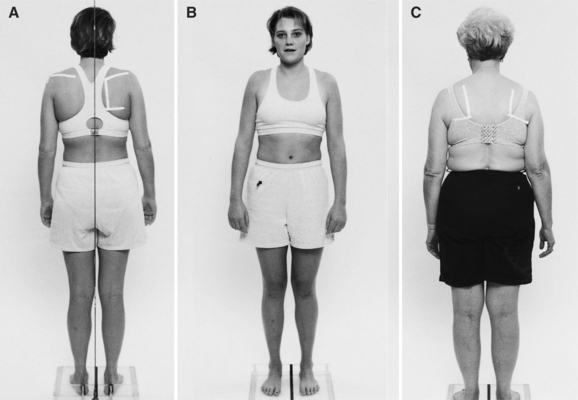
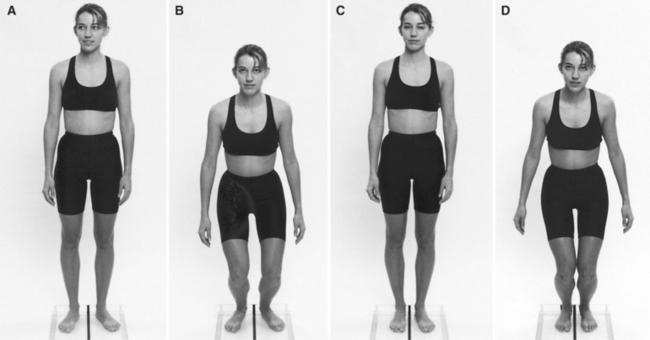
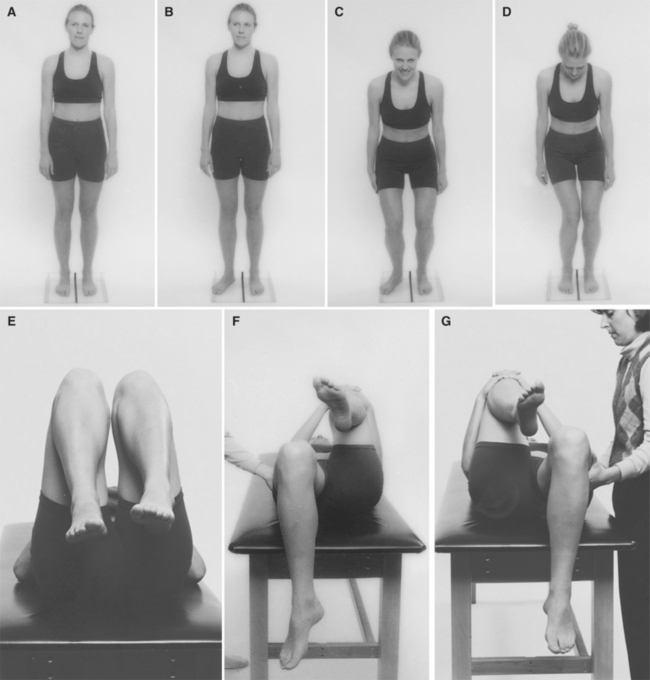
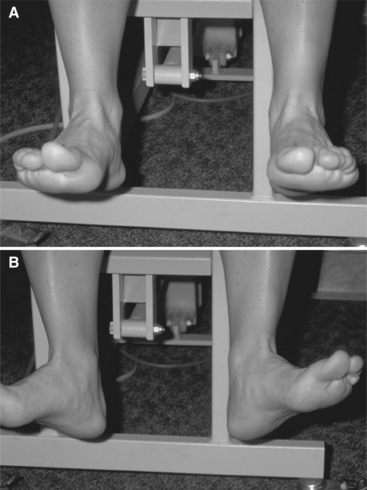
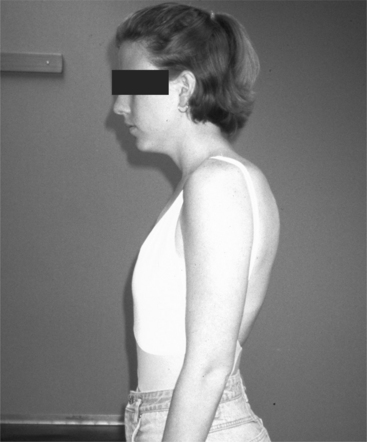
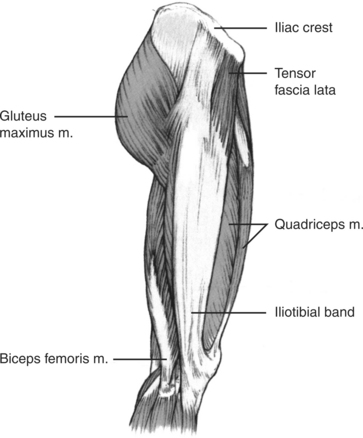
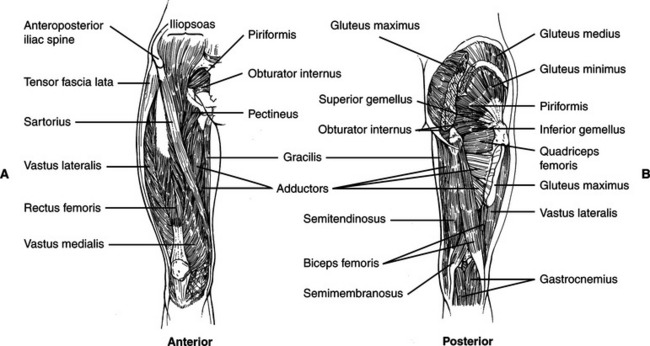
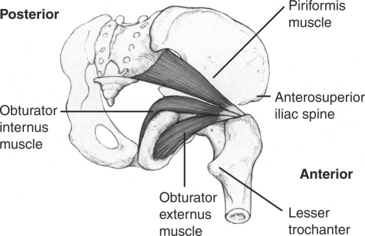
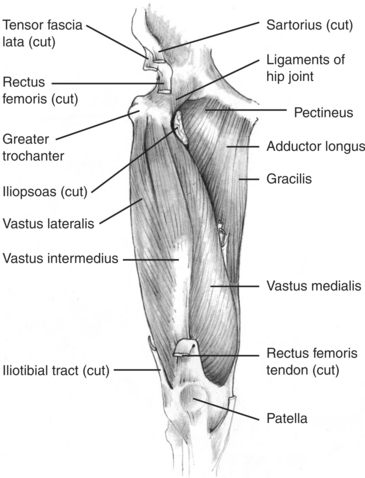
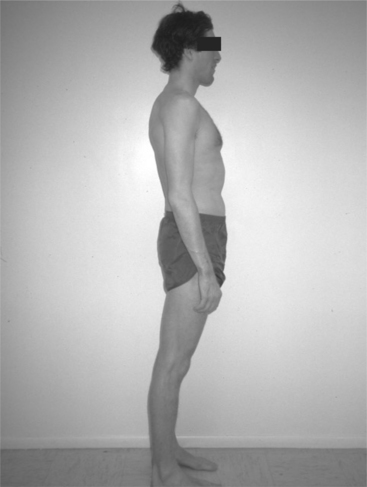
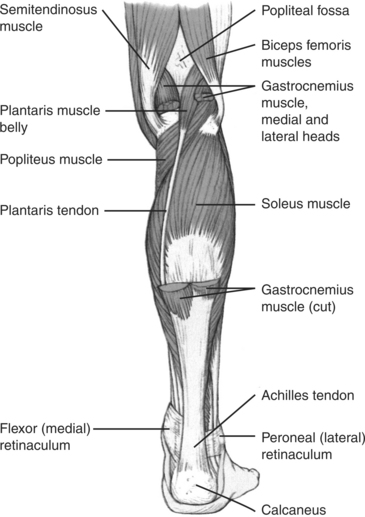
Chapter Four After consideration of the information presented in this chapter, the reader will be able to: 1 Describe acquired postural impairments and structural variations of the lower extremity that contribute to movement impairment syndromes. 2 Identify the specific muscle actions related to movement impairments. 3 Recognize the differences between diagnoses named for physiologic movement and those named for accessory movements. 4 Identify the characteristics of each movement impairment syndrome of the hip. In treating the patient with hip pain, the reader will be able to: 1 Perform an examination, consider the contributing factors, and establish a diagnosis. 2 Develop and instruct the patient in a diagnosis-specific treatment program and modification of the life activities, which contribute to the formation of the movement impairment syndrome. Two types of syndromes are discussed in this chapter. The first type is believed to arise from pain directly related to the hip joint. It is usually characterized by a movement impairment of an accessory motion of the femur. Thus these syndromes are identified by the name, femoral, and the offending accessory motion. The other type of syndrome is named for the physiologic motion that is painful because of musculotendinous dysfunction. This type of syndrome is identified by the name, hip, and impaired physiologic motion. Using the physiologic motion rather than the name of the muscle as the diagnosis for muscle dysfunction places the emphasis on correcting the pattern of muscular movement that performs the motion and not only on the palliative treatment of the painful muscle (Table 4-1). According to Kendall11 the ideal alignment of the pelvis is present when the anterior superior iliac spine (ASIS) is in the same vertical plane as the symphysis pubis. The angular deviation between the horizontal plane and a line connecting the ASIS with the posterior superior iliac spine (PSIS) is a frequently used clinical assessment of pelvic tilt. A common belief is that this angle should be very small, usually less than 5 degrees. A study performed on cadaver pelves indicates that when the ASIS is in the same vertical plane as the symphysis pubis, the angle between the horizontal plane and the plane between the ASIS and the PSIS varies as much as 12 degrees.2 Therefore the examiner should not expect a perfectly horizontal line between the ASIS and PSIS to be an indication of optimal alignment. In some women the ASIS is much lower than the PSIS, but not because of an anterior pelvic tilt (Figure 4-1). Such extreme variation in the relationship between the ASIS and the PSIS has not been observed in men. The pelvic structural variation that has been reported in men is that of a tall pelvis. A tall pelvis is one in which the height of the pelvis, as measured from the ischial tuberosity to the peak of the iliac crest, is a greater percentage of the overall height than the average percentage.3,13 Another structural variation that has been clinically observed is one in which a man’s beltline is at least 1 inch lower than the top of his iliac crest, rather than just above it (Figure 4-2). Men with high iliac crests have flat backs that are not associated with posterior pelvic tilts. Therefore two fairly common structural variations can be misinterpreted as acquired postural impairments: (1) a low position of the ASIS in women, which can be interpreted as anterior pelvic tilt; and (2) a structurally flat back in men with high iliac crests in relation to their beltline, which is often incorrectly interpreted as an acquired alignment of lumbar flexion. The hip joint angle is not always an accurate indication of pelvic tilt. This angle is affected by knee joint alignment and by pelvic alignment. When the knee is flexed the hip will be flexed, even if the pelvic tilt is neutral. When the knee is hyperextended the hip will be extended, even if the pelvic tilt is neutral (Figure 4-3) or slightly anterior. When pelvic tilt is present, there should be corresponding changes in the alignment of the spine and hip joint. If correcting the pelvic alignment causes an undesirable change in the alignment of the spine or the hip joint, the impairment is probably structural, not acquired. For example, a structural variation is present when (1) the ASIS appears low in relation to the PSIS, and (2) when tilting the pelvis posteriorly causes the lumbar spine to lose its normal inward curve (see Figure 3-9). Pelvic rotation around the vertical axis is often present in patients with hip pain. The examiner can assess pelvic rotation while he or she stands behind the patient and places his or her fingers parallel to and on the ASIS. From this position, deviations from the frontal plane of the line between the left and right iliac spines are fairly readily perceived. The examiner must be certain to observe the alignment of the patient’s feet to confirm that malalignment of the lower extremities is not the source of the pelvic rotation. If one foot is forward of the other, the pelvis may be rotated because of lower extremity alignment, not because of a pelvic rotation that is altering the alignment of the hip joints or spine. Hip flexion while standing erect can be present because of weakness or excessive length of the external oblique or rectus abdominis muscles. The hip flexor muscles can also be short or stiff. During gait the hip should extend 10 degrees.8 However, when the hip flexor muscles are short or stiff in relation to the abdominal muscles, instead of the compensation being reflected in hip motion, there may be exaggerated anterior pelvic tilt and increased lumbar extension. Although great emphasis is placed on stretching hamstring muscles, little attention is given to maintaining the length of the hip flexor muscles or ensuring that the abdominal muscles are preventing anterior pelvic tilt. Every step taken during gait requires maximal excursion of the hip flexor muscles, but only minimal excursion of the hamstring muscles is required. Maintaining adequate hip flexor muscle length and optimal performance of the abdominal muscles is important in preventing increased lumbar lordosis and excessive anterior pelvic tilt, particularly under dynamic conditions such as walking and running. Hip joint lateral asymmetry or apparent leg-length discrepancy is a fairly common postural fault (Figure 4-4). In this postural alignment, the hip on the side of the high iliac crest is in adduction and the other hip is in abduction.11 The difference between the heights of the iliac crests should be at least 1/2 inch to have clinical significance. Few individuals have true structural leg-length discrepancies in which either the femur or tibia is longer on one side. In individuals with structural differences, there is usually a history of congenital unilateral dislocation of the hip, a history of injury when they were younger that resulted in excessive bone growth, or a traumatic injury as an adult that caused a loss of bone length. An acute change in hip height in the patient with low back pain and radiation into the hip may be the result of weakness of the hip abductor muscles. Hip adduction on one side and abduction on the other can contribute to hip pain, to back pain, and even to the occurrence of ankle sprain. When one iliac crest is high, the lateral pelvic tilt causes lateral lumbar flexion at the lowest segments. Lateral flexion is associated with spinal rotation, which is a common factor in low back pain (see Chapter 3). The neck of the femur and the transverse axis of the femoral condyles (see Figure 2-22) form the angle of torsion or declination in the frontal plane. The normal angle is approximately 14 degrees anterior in the average adult, but there can be variation. Antetorsion (anteversion) is a pathologic increase in the angle of torsion. Retrotorsion (retroversion) is a pathologic decrease in the angle of torsion.15 At birth the angle of torsion is 30 to 35 degrees and the femoral head faces relatively anteriorly in the acetabulum. From birth to approximately 6 years of age the angle of torsion decreases and the orientation of the femoral head changes so that it faces more medially in the acetabulum. Children with antetorsion tend to prefer to sit in the W or “reverse tailor” position. Individuals with antetorsion that may be unilateral or bilateral tend to be pigeon-toed unless tibial torsion is also present. In the W-sitting position the tibia is rotated laterally, and thus it may undergo rotational changes that compensate for the medial rotation of the femur. In the uncompensated position when the foot appears pigeon-toed, correcting the foot alignment rotates the hip laterally, causing the head of the femur to point anteriorly in the joint, which can then become a source of hip pain depending on the amount of rotation. Also, when correcting the foot position by rotating the hip laterally, the limit of hip lateral rotation range of motion may be reached. Consequently, the hip may be forced into excessive rotation, or pelvic rotation will be exaggerated during walking. During gait the hip normally rotates 10 degrees laterally from the midstance phase until the swing phase.8 The patient with antetorsion can appear to be in excessive hip medial rotation and may have genu valgus (knock-knees). If this patient continues to sit with the hip maximally rotated medially, hip pain can develop because of excessive medial rotation. If the patient forces the hip to rotate laterally by exerting pressure on the knees when sitting in the “tailor” or “cross-legged” position, hip pain can also develop because of pressure into the anterior joint structures by the femoral head. The physical therapist can provide a useful screening service by assessing the presence of antetorsion in young girls who are participating in ballet or any dance discipline that requires the ability to rotate the hips laterally so that the feet point 90 degrees laterally. If the antetorsion is not identified, young girls participating in ballet in which maximum hip lateral rotation is required can compensate with excessive rotation at the knee joint (Figure 4-5). Retrotorsion can also contribute to low back pain if the patient participates in sports that require rotation with the feet relatively fixed, such as golf or racquetball. If the patient stands with the feet pointing straight ahead to hit a golf ball, he or she may reach the end of his or her hip medial rotation range and need to compensate with lumbar rotation because of the limited motion at the hips. To hit a golf ball correctly requires good hip medial rotational range.17 If the patient has retroversion, he or she should stand with the feet pointing laterally so that more hip medial rotational range is available than if he or she stands with the feet pointing straight ahead and the need to compensate with excessive lumbar rotation is avoided. Walking with the foot turned laterally can contribute to hallus valgus if, during the stance phase, the patient brings his or her weight line over the medial aspect of the great toe, pushing it into a valgus-oriented direction. The assessment of the angle of torsion needs to be performed carefully. Gelberman and colleagues6 report that assessment of antetorsion should be performed in the prone position with the hip joint in neutral and in the sitting position with the hip flexed. In this prone position, hip medial and lateral rotation can be measured. If the medial rotational range seems excessive (i.e., greater than 50 degrees) and lateral rotation is limited (i.e., less than 15 degrees from the vertical), antetorsion is suggested (Figure 4-6). With the patient remaining in the prone position, the examiner can also perform the Craig test. The Craig test is performed by rotating the hip through the full ranges into medial and lateral rotation while palpating the greater trochanter and determining the position in the range at which the trochanter is the most prominently lateral (Figure 4-7). At this point of rotation, the femur is optimally situated in the acetabulum. If the angle is greater than 15 degrees in the direction of hip medial rotation when measured from the vertical and long axes of the tibia, the femur is considered to be in antetorsion. By performing this test the examiner will have an indication of the degree of antetorsion of the femur. One study reported that the Craig test is more reliable than radiologic techniques.20 In the prone position with the hip extended and in neutral abduction/adduction, shortness of the hip abductor/medial rotator muscles can limit the lateral rotational range (Figure 4-8). In the hip flexed position, muscles cannot limit the lateral rotational range. In the Gelberman study, the structural antetorsion of the hip (as verified by magnetic resonance imaging) was present when the asymmetry of medial rotational range of motion was much greater than the lateral rotational range in both the hip flexed and the hip extended positions.6 In the case of retrotorsion, the range of lateral rotation should be greater than the range of medial rotation in both the flexed and extended positions of the hip. With the hip extended and the knee flexed, none of the musculature that limits medial rotation is taut, therefore the finding in this position should be valid (Figure 4-9). In the hip flexed position the gluteus maximus is pulled taut and can limit the medial rotational range of motion. The angle of inclination needs to also be considered in the assessment. The neck of the femur forms an angle with the shaft in the frontal plane that varies during the life cycle, but it is approximately 125 degrees in the adult. At 3 weeks of age, the angle is 150 degrees.18 In the adult, coxa valgum is present when the angle exceeds 130 degrees and coxa varum is present when the angle is less than 120 degrees (Figure 4-10). Relationships between movement impairment syndromes of the hip and the angle of inclination have not been identified to date, but relationships between the contour of the thigh and the angle of inclination are suggested. In the presence of coxa vara, a reasonable assumption is that the greater trochanter may be particularly prominent and may be less flush with the lateral side of the pelvis. The patient with lateral prominence of the proximal thighs often believes there is excessive fat on the thighs, which may not be the case. In the side-lying position this patient is usually in marked lumbar lateral flexion because of the width of the pelvis and the exaggerated lateral prominence of the femur. In the side-lying position the same structural factors contribute to excessive hip medial rotation and adduction when the patient sleeps with the uppermost hip and knee flexed so that the knee is resting against the bed. If the pelvis is wide the posterolateral hip muscles will be in a position of excessive stretch, which can lead to weakness. When the patient with weak abdominal muscles rolls from a supine to a side-lying position, the amount of trunk rotation can be greater than the rotation of the lower half of the body because the wider pelvis and hips have greater resistance to rotation than the narrower pelvis and hips. Clinically, an increased tendency of the tensor fascia lata–iliotibial band (TFL-ITB) to become short in the patient with this type of structure has been observed, possibly because the band remains positioned anterior to the greater trochanter rather than lateral over it. Distinguishing structural variations from acquired faults at the knee can be challenging. In the sagittal plane, hyperextension and flexion can be acquired postural faults with hyperextension more common. In some patients the hyperextension is so exaggerated that even when attempting to stand correctly, the femur is anterior to the tibia rather than in the same plane (see Figure 2-36). With this degree of hyperextension, the posterior joint capsule is stretched, the anterior cruciate ligament is slacked, and the anterior articular surface of the tibia is altered by the compressive forces. In other patients the bowing of the tibia in the sagittal plane may suggest minimal genu recurvatum (Figure 4-11). In this condition the tibia is bowed, but the knee joint is not always in hyperextension. Careful examination is necessary to distinguish the presence of one or both of these malalignments. Postural knee flexion, particularly in the older individual, is usually a sign of degenerative knee joint disease. In the frontal plane, genu valgum (knock-kneed) and genu varum (bowlegged) can be either structural or acquired impairments (Figure 4-12). Although tibial varum, genu varum, and bowlegged are interchangeable terms,22 clinically these often appear as different conditions. In some patients the bowing appears to be confined to the tibia, and in others the knee joint appears to be bowed. As shown in Figure 4-13 the right tibia appears bowed (tibial varum), but the knee joint appears to be relatively well aligned. In contrast, the left knee appears to be bowed with a greater degree of tibial bowing. Standing on the left lower extremity increases the degree of varus, but standing on the right does not (Figure 4-14). Increased varus moment, such as that evident in the left lower extremity, can contribute to degenerative knee joint disease. Therefore radiologic analysis of the actual relationship of the femur to the tibia, as well as the shape of the tibia, is important to ascertain whether there are changes in the knee joint or simply a variation in the shape of the tibia. Exaggerated genu varum is most often an indication of degenerative knee joint disease (Figure 4-15). The patient with genu varum often walks with an antalgic gait, because this motion decreases the varus moment on the knee during the stance phase. When there is true genu varum at the knee joint and the patient does not shift his or her weight laterally during walking, the varum moment at the knee is increased, which can further contribute to the malalignment (see Figure 4-14). Hip medial rotation with knee hyperextension can give the appearance of genu varum (Figure 4-16). Genu valgum appears to be a variation in the angulation of the femur rather than the tibia (Figure 4-17). Acquired postural impairments such as hip medial rotation can also give the appearance of genu valgum (see Figure 4-17). If the problem is an acquired fault, the foot should be pronated so that correction of the rotation also corrects the foot position. If the foot is neutral or supinated, the rotation is most likely structural (i.e., femoral antetorsion). Tibial torsion, which is a structural rotation of the shaft of the tibia and not rotation of the entire tibia at the knee joint, is another structural variation (Figure 4-18). Tibial torsion is assessed with the knee flexed by determining the angle between the medial and lateral malleoli in relation to the horizontal plane. The normal angle is less than 20 to 25 degrees. Most often the torsion is in a lateral direction. If the foot is in the plane of the ankle, it will face laterally. Shortness of the iliotibial band (ITB) can contribute to lateral tibial rotation at the knee joint. If structural torsion is present and the ITB becomes short and the knee joint is flexible the pull of the band will laterally rotate the tibia (Figure 4-19). If the foot faces anteriorly, it is in inversion and the range into dorsiflexion may be limited because of this alignment (Figure 4-20, page 124). When the foot is pronated, proximal forces primarily originating at the pelvis and hip contribute to the alignment fault. Most commonly, poor control of the hip lateral rotator muscles allows the hip to rotate medially and exert a pronatory stress on the foot. When the foot is supinated and rigid, the forces are directed up the closed kinetic chain rather than down. In this situation as in many others, the body follows the path of least resistance for motion. If the foot is stiff and does not adequately dorsiflex, the stress can be at the knee joint or at the hip joint if the knee is stable. Most often the knee joint is affected, causing either a rotation- or posterior-directed stress. Often tibial bowing in the sagittal plane can be observed in the patient with rigid feet or in the frontal plane if the foot is markedly supinated. Anterior pelvic tilt.: The ASIS is anterior to the vertical plane through the symphysis pubis.11 Commonly used clinical indicators are when the ASIS is lower than the PSIS and the hip joint is flexed as indicated previously. The differences between the relative heights of the ASIS and PSIS should be greater than 15 degrees for clinical significance. Posterior pelvic tilt.: The ASIS is posterior to the vertical plane through the symphysis pubis.11 When measuring the anterior and posterior pelvic tilt, the angle formed between the line connecting the posterior and anterior iliac spines and the horizontal plane varies by ±12 degrees in normal individuals.2 Lateral pelvic tilt.: One iliac crest is higher than the other with differences of less than 1/2 inch considered within the normal range of variability. Rotation.: The vertical plane through one ASIS is forward of the vertical plane through the other ASIS. Clockwise rotation occurs when the left ASIS is forward of the right. When the pelvis is rotated clockwise and the lower extremities appear to be facing anteriorly, the right hip joint is in postural medial rotation while the left hip joint is in lateral rotation. Often these faults of postural alignment are consistent with the differences in muscle stiffness or length. For example, in the alignment described, the right TFL may be short and the right posterior gluteus medius (PGM) muscle may be long, which is consistent with the postural alignment. On the left side, the PGM muscle or the hip lateral rotator muscles, the obturators, gemelli, and piriformis could be short or stiff. Hip flexion.: Movement occurs in an anterior direction around a coronal axis. The full range through flexion is approximately 125 degrees. During hip flexion there is slight posterior glide of the femoral head. Hip extension.: Movement occurs in a posterior direction around a coronal axis. The normal range is approximately 10 degrees. Normal standing alignment is 0 degrees of hip extension. During hip extension there is slight anterior glide of the femoral head. When the pelvis is tilted posteriorly enough to flatten the lumbar spine, the hip is in 10 degrees of extension in most individuals. When an individual stands with the knees hyperextended (genu recurvatum), the hip is extended. Therefore when the posterior tilt flattens the lumbar spine and the individual has hyperextended knees, the hip joint extension may approach 20 degrees (see Figures 2-34). Hip medial rotation.: Movement occurs around a longitudinal axis with the anterior surface of the thigh turning toward the midsagittal plane. The accessory motion is posterior glide. Normal range of motion is approximately 45 degrees, but this range is highly variable. Structural conditions affecting the range of motion include femoral antetorsion and retrotorsion, which have been discussed. Medial rotational range appears excessive in the individual with antetorsion of the hips, which, based on clinical experience, has a higher incidence in women than in men. The finding of hip antetorsion on one side only is common. Hip lateral rotation.: Movement occurs around a longitudinal axis with the anterior surface of the thigh moving away from the midsagittal plane. The accessory motion is anterior glide. Range of motion is approximately 45 degrees, but this range is highly variable. In the individual with hip retrotorsion, the range into lateral rotation appears to be excessive. This condition is found more often in men than in women. Abduction.: Movement occurs away from the midsagittal plane in the lateral direction. Normal range is approximately 45 degrees. During abduction, the femoral head should move inferiorly. Anterior glide.: Movement occurs in an anterior (ventral) direction. According to the convex-concave rule, anterior glide occurs with hip extension and lateral rotation. Posterior glide.: Movement occurs in a posterior (dorsal) direction with hip flexion and medial rotation. Superior glide.: Movement occurs along the longitudinal axis in the cephalad direction. Superior glide occurs during hip adduction. Inferior glide (long axis distraction).: Movement occurs along the longitudinal axis in the caudal direction with the hip in the resting position. Inferior glide occurs during hip abduction. Anterior Trunk Muscles Affecting the Pelvis The external oblique abdominal muscle tilts the pelvis posteriorly when acting bilaterally (see Figure 3-26). When contracting unilaterally and acting with the contralateral internal oblique muscle, the action is rotation of the trunk or pelvis. For example, acting together the left external oblique and right internal oblique muscles rotate the trunk counterclockwise or the pelvis clockwise. Acting unilaterally, the lateral portion of the external oblique abdominal muscle moves the iliac crest on the same side cranially, causing a lateral tilt. This muscle commonly tests weak, particularly in women. Because of the critical role of the external oblique in tilting the pelvis posteriorly, flattening and supporting the lumbar spine, and controlling rotation, particularly with regard to preventing pelvic rotation, adequate performance is important. The external oblique muscle is often less dominant than the rectus abdominis muscle, which also tilts the pelvis posteriorly.9 Therefore specific training for adequate participation is often necessary. Bilateral contraction of the external oblique muscles narrows the infrasternal angle and compresses the ribs and thus can reduce the tendency for the ribs to flare. The rectus abdominis muscle flexes the thorax (curls the trunk) and tilts the pelvis posteriorly and is often more dominant than the internal and external oblique muscles.21 If the rectus abdominis becomes dominant and the performance of the obliques is compromised, control of trunk or pelvic rotation is compromised because the rectus abdominis cannot control rotation. Because it attaches to the sternum, shortness or stiffness of this muscle contributes to a depressed chest and thoracic kyphosis (Figure 4-21). The transversus abdominis muscle stiffens the spine and compresses the viscera. This abdominal muscle is another of those whose performance can be easily enhanced by a conscious effort to contract the muscle by “pulling the navel toward the spine.”7,19 The iliopsoas muscle (see Figure 3-24) flexes the hip or tilts the pelvis anteriorly when the lower extremity is fixed. In the erect position, the iliopsoas muscle exerts a weak extension moment on the upper lumbar spine and a flexion moment on the lower lumbar spine.1 When the lumbar spine is flexed, the iliopsoas muscle exerts a flexion moment on all segments of the lumbar spine. According to the study by Bogduk and associates3 the moments exerted on the lumbar spine are minimal. The major forces acting on the lumbar spine are compression and anterior shear forces. The lateral flexion moments exerted on the lumbar spine by the iliopsoas muscle are small.3 When acting bilaterally the erector spinae muscles cause anterior pelvic tilt. When acting unilaterally these muscles cause lateral pelvic tilt (see Figure 3-21). The quadratus lumborum muscle tilts the pelvis laterally; when the pelvis is fixed, it flexes the trunk laterally (see Figure 3-24). Because of its attachment to the transverse processes of lumbar vertebrae, the quadratus lumborum muscle contributes to lateral trunk flexion if it is short. The TFL-ITB flexes, rotates medially, and abducts the hip (Figure 4-22). When the knee is extended, the TFL-ITB can act to stabilize the knee, although it does not extend the knee.10,16 In patients with a short ITB, during muscle length testing, if the hip is adducted from the hip extended and abducted position, the knee will extend from the passive tension of the band. When a patient sits without using the backrest on a chair, he or she is using the hip flexor muscles, which can include the TFL to maintain the hip flexion position. The lateral attachment of the TFL onto the tibial tuberosity can contribute to lateral tibial rotation if the knee is not stable. The lateral slips of the band attach to the patella and thus contributes to lateral glide of the patella. The TFL commonly becomes short and stiff and is often mistaken for shortness of the iliopsoas muscle when, during hip flexor length testing, the hip is prevented from abducting. The TFL muscle tests strong when the iliopsoas or PGM muscle tests weak with the exception of when the TFL becomes strained. When the TFL becomes stiff or short and the lower extremity is fixed, its contraction can result in rotation of the pelvis because the TFL muscle is a medial rotator of the hip. If segments of the lumbar spine have become particularly flexible and easily rotate, the rotation of the pelvis will also cause rotation of the lumbar spine. The sartorius muscle flexes, rotates laterally, and abducts the hip. It also flexes and rotates the knee medially (Figure 4-23). The rectus femoris muscle flexes the hip and extends the knee. The gluteus maximus muscle extends and laterally rotates the hip (see Figure 4-23). The upper one half of the muscle abducts the hip; the lower one half adducts the hip. Approximately 80% of the gluteus maximus inserts into the ITB. Therefore this muscle exerts a strong influence on the band and can contribute to restricted hip adduction range. Shortness of this muscle can contribute to compensatory lumbar flexion when the individual is sitting with the hips flexed. The posterior portion of the gluteus medius muscle extends, abducts, and laterally rotates the hip (see Figure 4-23). This portion often becomes excessively lengthened or weak. Careful muscle testing allows the examiner to differentiate between the two conditions. If the patient cannot hold at the end of the range but is able to take strong resistance after the hip has adducted 10 to 15 degrees, the posterior portion of the gluteus medius muscle is probably excessively long. If the patient cannot hold at the end of the range and can tolerate only minimal resistance throughout the range of motion, the posterior portion is probably weak. The weakened muscle is usually associated with pain in the muscle belly, which is evident upon contraction or with palpation. If the muscle is long, the pain usually occurs during hip joint motions, because the pain source is the faulty control of the head of the femur in the acetabulum. This muscle is commonly affected by postural faults. The gluteus minimus muscle abducts, rotates medially, and assists in flexion of the hip (Figure 4-24). The gluteus minimus is another muscle that contributes to the abduction-medial rotation tendency of the hip. The piriformis muscle rotates laterally, extends, and abducts the hip when the hip is in flexion (see Figure 4-24). The length of this muscle needs to be considered carefully in the piriformis syndrome. Although the piriformis is commonly considered to be short when this syndrome is present, Kendall11 reports that symptoms of this syndrome can also be found in the patient who has a lengthened piriformis muscle. In the clinical experience of the author of this text, this syndrome is found more frequently in the patient with a lengthened piriformis than in the patient with the shortened piriformis. The therapist must carefully examine the length of the muscle before planning intervention for the syndrome. The obturator internus and externus and superior and inferior gemelli muscles are lateral rotators. They frequently become weak or stiff, but these muscles can also become excessively lengthened (see Figure 4-24). The obturator internus, superior and inferior gemelli, and piriformis muscles assist in abduction when the hip is flexed, whereas the obturator externus assists in the adduction of the hip. In the patient who stands in hip extension with the upper back in a swayback position, these muscles can become short or stiff and can create resistance to posterior gliding of the hip during flexion. Stiffness or shortness can contribute to anterior groin pain, which is a symptom of the femoral anterior glide syndrome described in this chapter. The lateral rotator muscles are commonly affected by postural faults. Dysfunctions of these muscles are commonly observed in the patient with dysfunction of the central nervous system. The pectineus muscle adducts, rotates medially, and assists in flexion of the hip (see Figure 4-23). The gracilis muscle adducts the hip and medially rotates and flexes the knee. The adductor longus muscle adducts and flexes the hip. The adductor brevis muscle adducts and flexes the hip. The adductor magnus muscle adducts the hip with the anterior fibers flexing the hip and the posterior fibers extending the hip. As discussed by Kendall, this muscle can participate in both medial and lateral rotation.11 The quadriceps femoris muscle consists of four major muscle groups: rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius (Figure 4-25). The rectus femoris muscle flexes the hip and extends the knee. The vasti arise from the anterior and posterior (linea aspera) surfaces of the femur. Because these muscles attach to the femur and tibia, they extend the knee and do not directly influence the hip joint. The vastus medialis oblique muscle has an important role in the medial glide of the patella.12 The semimembranosus and semitendinosus muscles extend and rotate the hip medially and flex and rotate the knee medially (see Figure 4-23). This pair of muscles can become stiffer or shorter than its synergist, the biceps femoris muscle. This condition is seen in the individual who has excessive hip medial rotation. The imbalance is most evident during knee extension performed while in the sitting position. In the presence of shortness of the medial hamstrings, if the femur is allowed to rotate medially as the knee extends, the range of motion is close to normal. If the medial rotation of the femur is prevented as the knee extends, the range of motion is limited. The biceps femoris muscle (see Figure 4-23) extends and rotates the hip laterally and flexes and rotates the knee laterally. The biceps femoris can become the dominant muscle for hip lateral rotation, the result of which is pain at the knee or the hip. The reason for this painful condition at the hip is that the biceps femoris muscle does not have attachments that extend from the pelvis to the femur. The short head of the biceps femoris muscle arises from the distal femur and inserts into the tibia. The distal origin of this muscle limits the effectiveness of its control on the proximal femur. If the knee is particularly flexible, contraction of the biceps femoris can contribute to lateral rotation of the tibia rather than just lateral rotation of the femur with the result being knee pain. The hamstring muscles contribute to a number of motions of the lower extremity. Because of their multiple actions, as well as their requirements of extensibility, the hamstring muscles are frequently subject to strain. This strain can be attributed in part to their overuse when synergists are underused. An example of this problem is the dominant use of the hamstring muscles and the underuse of the gluteus maximus muscles. Runners with swayback posture, who have an atrophy and a weakness of the gluteus maximus muscles, can be predisposed to hamstring muscle strain (Figure 4-26). The hamstring muscles can also produce knee extension, substituting for the quadriceps muscles. When the foot is fixed by contact with the floor, hip extension also produces knee extension. Discrepancies in the amount of participation of the medial versus the lateral hamstring muscles can also develop. For example, cyclists who keep their hip rotated medially while riding their bicycles tend to use the medial hamstring muscles more than the lateral hamstring muscles. The lateral hamstrings can become dominant lateral hip rotators and can diminish the activity of the intrinsic hip lateral rotators, obturators, gemelli, and piriformis muscles of the pelvic girdle. Observing the movement pattern and manual muscle testing are used to assess the presence of a change in dominance. For example, when a patient with persistent hamstring muscle strain has a swayback posture and poor definition of the gluteus maximus muscle, the results of the following tests are used to assess whether the hamstring muscles have become the dominant hip extensor: • In the prone position at the initiation of hip extension, a visible change occurs in the contour of the hamstring muscles. The change in the contour of the gluteus maximus muscle, however, does not occur until the hip is almost completely extended. • The manual muscle testing of the gluteus maximus muscle can confirm whether the muscle is weak or strong. The gastrocnemius muscle flexes the knee and plantar flexes the ankle (see Figure 4-23). Along with the soleus muscle (Figure 4-27), the gastrocnemius muscle is the primary plantar flexor of the ankle. However, in the individual involved in activities such as dance, this muscle may be weak. Weakness can also be found in the individual who has short heel cords and who uses the shortness to produce the force required for plantar flexion. To assess the presence of weakness, the therapist needs to provide resistance against plantar flexion at the ankle joint by holding at the calcaneus with the subtalar joint in neutral rather than at the metatarsal heads. When there is weakness of the gastrocnemius-soleus muscle group, the patient is unable to plantar flex the ankle to overcome the resistance applied by the therapist. The same patient generates a stronger plantar-flexion force against pressure applied at the level of the metatarsal heads. The explanation is that the patient is recruiting additional plantar flexors, such as the peroneus longus, tibialis posterior, flexor hallucis longus, and flexor digitorum longus muscles, to plantar flex the ankle and joints of the foot (Figure 4-28). To encourage use of the gastrocnemius-soleus group, the patient should “lift the heels” when performing plantar flexion rather than continuously repeating the faulty movement pattern of “going up on the toes.”
Movement Impairment Syndromes of the Hip
Introduction
Normal Alignment of the Hip
Pelvis
Hip Joint
Knee Joint
Sagittal Plane
Frontal Plane
Foot
Motions of the Hip
Hip Joint Motions
Hip Joint Accessory Motions
Muscular Actions of the Hip
Posterior Muscles Affecting the Pelvis
Anterior Muscles Affecting the Hip Joint
Posterior Muscles Affecting the Hip
Medial Muscles Affecting the Hip
Anterior Muscles Affecting the Hip and Knee
Posterior Muscles Affecting the Hip and Knee
Posterior Leg Muscles Affecting the Knee and Ankle
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Movement Impairment Syndromes of the Hip