Essentials of Diagnosis
- Vasculitis associated with mixed cryoglobulinemia (MC) involves both small- and medium-sized vessels. The skin is the most commonly involved organ.
- Other frequently affected organs include the joints, peripheral nerves, and kidneys. The central nervous system, gastrointestinal tract, and lungs are involved rarely or very rarely in MC.
- Virtually all patients are rheumatoid factor (RF) positive.
- Lower survival rates are observed with age over 60 years, male sex, and renal involvement.
General Considerations
Cryoglobulins are immunoglobulins (Ig) that precipitate from the serum at low temperatures (see method of collection under Laboratory Findings). Cryoprecipitates are composed most commonly of IgG and IgM (either singly or, in the case of mixed cryoglobulinemia, together). Occasionally IgA may be associated with clinically relevant cryoglobulin syndromes, as well. Cryoglobulinemia is divided into three clinical subsets—Types I, II, and III (Table 36–1)—based on two features: the clonality of the IgM component and the presence of RF activity. RF activity, by definition, is the reactivity of an IgM component with the Fc portion of IgG. This chapter focuses on cryoglobulinemia types II and III. (Type I cryoglobulinemia is usually not “mixed,” being associated with only a monoclonal IgG or IgM in the setting of a malignancy.)
| Subtype | Rheumatoid Factor Positivity | Monoclonality | Associated Diseases |
|---|---|---|---|
| Type I | No | Yes (IgG or IgM) | Hematopoietic malignancy (multiple myeloma, Waldenström macroglobulinemia) |
| Type II | Yes | Yes (polyclonal IgG) | Hepatitis C (other infection, Sjögren syndrome, monoclonal IgM, systemic lupus erythematosus) |
| Type III | Yes | No (polyclonal IgG and IgM) | Hepatitis C (other infection, Sjögren syndrome, systemic lupus erythematosus) |
Formerly referred to as “essential” MC, hepatitis C virus (HCV) infections are now known to be associated with approximately 90% of all cases of MC. Latency periods of up to 15 years between the occurrence of HCV infection and the development of clinical signs of MC have been reported. In some cases, the presentation of HCV may be the development of the clinical features of MC (usually palpable purpura). Cryoglobulins also occur in the setting of other types of infections as well as in connective tissue disorders (eg, Sjögren syndrome) and hematopoietic malignancies.
The presence of cryoglobulins is not always associated with clinical disease, but these proteins may result in a wide variety of immune complex–mediated complications. The term “mixed cryoglobulinemia” was coined to differentiate types II and III (both of which contain mixtures of both IgG and IgM) from type I (which contains only a single monoclonal antibody).
When an underlying infection, autoimmune disorder, or malignancy can be identified, the preferred treatment approach is to direct therapy toward the underlying condition. B cell depletion strategies are often coupled with antiviral therapies in patients with HCV-associated cryoglobulinemia. Occasionally, in patients with rampant systemic vasculitis, generalized immunosuppression or measures designed to remove immune complexes (ie, plasma exchange) may be required for limited periods.
Clinical Findings
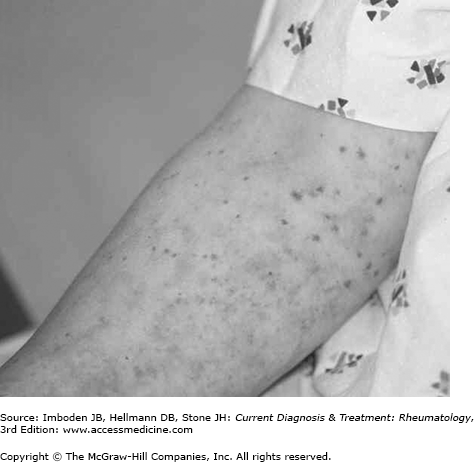
The symptoms and signs of MC-associated vasculitis are caused by the vascular deposition of cryoprecipitate components. In type II MC, the cryoprecipitate contains polyclonal IgG, a highly restricted monoclonal IgM that has RF activity, low-density lipoprotein and, in cases of HCV-associated disease, HCV RNA. In general, the diagnosis of MC is made by some combination of the following: (1) recognition of a compatible clinical syndrome, accompanied nearly invariably by cutaneous vasculitis of small blood vessels (Figure 36–1); (2) isolation of cryoglobulins from serum; (3) detection of antibodies to HCV or HCV RNA; and (4) biopsy of other apparently involved organs as necessary to exclude other diagnoses. Because assays for cryoglobulins are not 100% sensitive and because HCV does not cause all cases of MC, all four of these conditions are not required.
A major hallmark of MC is a small-vessel vasculitis of the skin. Medium-vessel vasculitis may also be present, but this type of involvement generally does not occur without small-vessel disease. Biopsy of the skin with immunofluorescence studies shows an immune complex–mediated leukocytoclastic vasculitis, with deposition of IgG, IgM, C3, and other immunoreactants in and around the walls of small- and medium-sized vessels. Vascular thrombi are also prominent in many cases. Palpable purpura with a predilection for the lower extremities is the typical skin rash, but the rash is also found sometimes on the upper extremities, trunk, or buttocks. In addition, a host of other types of vasculitic rashes may be encountered, depending on the size of blood vessel involved. Such findings may include macules, papules, vesiculobullous lesions, urticarial lesions in the setting of small-vessel involvement, and ulcers above the malleoli—potentially extensive—in the context of medium-vessel disease.
Arthralgias are a prominent symptom in most cases of MC. The typically involved joints are the proximal interphalangeal and metacarpophalangeal joints and the knees. Frank arthritis, much less common than arthralgias, occurs in a small minority of patients. The arthritis of MC is nondeforming. Raynaud phenomenon and acrocyanosis may also complicate MC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree