Microfracture for Osteochondral Lesions of the Talus: Perspective 1
Hajo Thermann
Christoph Becher
DEFINITION
The terminology of osteochondral lesions is not uniform: Transchondral fractures, osteochondral fractures, flake fractures, and osteochondritis dissecans (OCD) are used to describe the same entity. Most recently, “osteochondral lesions of the talus (OLT)” has emerged as the most common term used to describe these lesions.
OLTs are characterized by aseptic separation of a fragment of articular cartilage, with or without attached subchondral bone.
The causes for OLTs remain controversial. The most important distinction to make is if the lesion is acute or chronic.
ANATOMY
The talar body is trapezoidal. The anterior surface is on average 2.5 mm wider than the posterior surface. The dome is covered by the articular surface, which articulates with the tibial plafond. The medial and lateral facets articulate with the medial and lateral malleoli.
About 60% of the talar surface is covered by articular cartilage.
Most of the blood supply enters through the neck of the talus via the sinus tarsi.
Biomechanical studies have shown that the talar cartilage is softest at the posteromedial part, whereas the maximum thickness is found at the posterolateral corner.
The tibial cartilage is 18% to 37% stiffer than the corresponding sites on the talus.2
PATHOGENESIS
Lateral lesions are most frequently caused by acute trauma, with a common mechanism being a dorsiflexed ankle forced into inversion. This results in impaction of the talus on the fibula.
In our experience, lateral lesions are often located in the anterior part of the talar dome. They tend to be shallower than medial lesions.
Medial lesions are mostly associated with a single or repetitive supination trauma (microtrauma).
Impaction of the medial talus on the tibia with a plantarflexed ankle forced to hindfoot inversion combined with external rotation is regarded as the causative mechanism.
Medial lesions are more common (inversion ankle sprains are the most common sports injury) than lateral lesions and occur mostly in the middle or posterior third of the talus. These lesions appear cup-shaped and deeper than lateral lesions.
Injury to the talar dome associated with supination trauma to the ankle generally exhibits one of two trends in recovery:
In most, swelling and pain resolve expediently.
Occasionally, swelling and pain persist. In these cases, our investigations using magnetic resonance imaging (MRI) suggest that 20% of these ankles with persistent pain and swelling have an identifiable bone bruise on the medial talar dome.
The question is the long-term effect of an episode of subchondral effusion (hemorrhage?) on the cartilage layers: minor trauma on the tide zone with a prolonged separation?
In our experience, chronic ankle instability creates a medial talar dome lesion with an abrasive character that suggests a repetitive insult. Unlike the classic OCD with a subchondral origin of the pathology, these deteriorations of the cartilage derive from a classic mechanical overload. The long-term damage is a full-thickness cartilage lesion at the medial talus and tibia plafond with varus hindfoot alignment. Medial lesions may be detected bilaterally, mostly with coincidence of bilateral ankle sprains.
In contrast to chronic osteochondral lesions occurring as a result of repetitive trauma, acute osteochondral injuries result in an acute separation of an osteochondral fragment.
Other reported causes for OLTs are genetic predisposition and endogenous factors. These causes lack meaningful evidence-based support and represent little more than theories.
NATURAL HISTORY
Initially, the patient experiences ankle pain with impact activities such as jogging and sports that subsides immediately with rest.
With time, increasing ankle pain generally forces the patient to stop impact sports activities. The time frame varies from patient to patient based on the patient’s pain threshold and age.
Some cases have an identifiable traumatic incident (ie, ankle sprain) where an initially inapparent lesion is detected and the patient never returns to a pain-free state. (For us, this is an interesting phenomenon: Does the lesion cause the pain or is there a psychosomatic influence once the lesion is detected on the imaging study?)
Some OLTs are incidentally discovered with screening imaging studies (radiographs or MRI scans). For instance, an imaging study is obtained for an acute ankle sprain and an obviously nonacute OLT is noted. These patients have an anticipated normal healing course of the ankle injury with complete subsidence of pain and swelling and should never be treated for the asymptomatic OLT.
Over the past 20 years, our clinical experience (H.T.) in treating OLTs suggests that there is no evidence to support that the natural history of untreated OLTs is the development of osteoarthritis of the ankle. We thus view surgical management of OLTs as one of pain relief and not as a salvage procedure to prevent osteoarthritis of the ankle joint.
McCullough and Venugopal18 found that in five of six patients treated conservatively for OLTs, radiologic assessment at a mean follow-up of nearly 16 years (range 7 to 28 years) showed that the lesions had failed to heal and that in each instance the ankle joint was relatively asymptomatic, without evidence of diffuse degenerative changes.
PATIENT HISTORY AND PHYSICAL FINDINGS
Acute OLTs must be ruled out after traumatic events when an OLT or osteochondral fracture is suspected.
In most cases, patients complain of chronic ankle pain with or after sports activities. Swelling and stiffness are accompanied in advanced cases with more constant pain. Occasionally, but not always, mechanical symptoms are present, including catching, locking, and giving way.
The severity of symptoms may not correlate with the severity of the lesion.
Physical examination is relatively nonspecific in OLTs.
By having the patient plantarflex the foot and ankle, the anterior aspects of the talar dome can be palpated at the anteromedial and anterolateral joint space. Tenderness in the specific area may indicate an osteochondral lesion.
Tenderness behind the medial malleolus by having the patient dorsiflex the ankle may indicate a posteromedial lesion.
Range of motion of the ankle is tested with the knee flexed to eliminate restriction by shortened gastrocnemius muscles. Range of motion is limited only in case of ankle synovitis and effusion.
The examination should also include evaluation of associated pathology, taking into account the differential diagnosis.
Bony structures, tendons, ligaments, and soft tissue structures should be palpated and tested against resistance to discern tenderness of the specific anatomic part.
Ligamentous instability or laxity is assessed with the anterior drawer test and passive varus or valgus stress test.
Pushing the ankle against resistance helps identify inflammation or partial tears of tendons of the contracted muscles.
Palpation of pulses and neurologic assessment should be part of every examination.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard ankle plain film radiographs should include anteroposterior (AP), lateral, and mortise views. However, only 50% to 66% of osteochondral defects can be visualized by plain film radiographs alone.15 The radiologic signs vary from a small area of compression of subchondral bone to a detached osteochondral fragment.
The four-stage classification system by Berndt and Harty6 is still the gold standard based on radiologic appearance:
Stage I: compression lesion, no visible fragment
Stage II: fragment attached
Stage III: nondisplaced fragment without attachment (FIG 1)
Stage IV: displaced fragment
Stress view radiographs are frequently recommended if instability is suspected. However, a thorough clinical examination is more important and in most cases is sufficient for assessment.
A computed tomography (CT) scan offers more accurate staging and characterization of the lesion, with clear definition of the exact dimensions of the osseous portion of the lesion, but subjects the patient to relatively high radiation. We recommend and use limited CT studies with minimal radiation exposure to the patient and sufficient characterization of the OLT.
MRI is an ideal screening tool and, in our opinion, the method of choice for all patients with suspected OLTs. MRI defines occult injuries of the subchondral bone and cartilage that may not be detected with routine radiographs. Furthermore, the MRI is accurate in diagnosing associated stress fractures and stress reactions—for example, in the medial malleolus. Although MRI may demonstrate associated edema in the talar body, in our hands, accurate sizing of the OLT is feasible.
Dipaola et al9 developed an MRI classification system based on Berndt and Harty’s original radiographic system.
Stage I: thickening of articular cartilage and low signal changes
Stage II: articular cartilage breached, low signal rim behind fragment indicating fibrous attachment
Stage III: articular cartilage breached, high signal changes behind fragment indicating synovial fluid between fragment and underlying subchondral bone (FIG 2A,B)
Stage IV: loose body
DIFFERENTIAL DIAGNOSIS
Degenerative joint disease (any origin)
Soft tissue or bony impingement on the ankle joint
Ankle or subtalar instability
Subtalar joint pathologies (ie, chondral lesion, subtalar impingement lesion)
Tendinitis or partial rupture of the tibialis posterior, tibialis anterior, or peroneal tendons
Tarsal coalition (talocalcaneal)
Stress fracture (medial or lateral malleolus, talus)
NONOPERATIVE MANAGEMENT
The approach and objectives in nonoperative treatment of OLTs vary from those of surgical management.
In children and adolescents, the goal is to reverse the cartilage separation and to treat the pain. Partial weight bearing (not unloading) of about 15 kg for 2 to 3 months and nonsteroidal anti-inflammatory agents (NSAIDs) at
appropriate doses adjusted for age and weight for 1 to 2 months to relieve the patient’s pain are important from physical and psychological standpoints. Given the advantages shown in clinical and experimental trials, we recommend use of the combination of chondroitin and glucosamine sulfate for at least 6 months. We also encourage the daily use of moist heat to enhance vascularity to the ankle and talus. In select cases of extensive talar body edema, we have observed, based on anecdotal experience, that hyperbaric oxygen (HBO) therapy (20 dives, 20 minutes each) results in resolution of edema and pain. We favor low-impact exercise such as biking and swimming for about 1 year. Regardless of MRI findings, the young patient should gradually return to age-appropriate activities once she or he is pain-free. We recommend yearly serial MRI and clinical examinations to monitor talar body status.
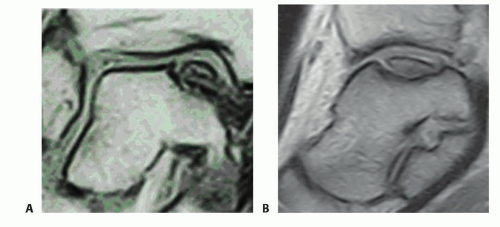
FIG 2 • A. Coronal MRI (T1-SE-540/20) showing an osteochondral lesion stage III. B. Sagittal MRI (T2-SE-2000/90) showing an osteochondral lesion stage III.
Although osteochondral transfer systems and autologous chondrocyte implantation (ACI) are accepted salvage procedures, to date, we lack an optimal reconstruction of an OLT. Nonoperative treatment for OLTs is the treatment of choice if the adult patient has minor complaints. The goal of nonoperative treatment is not to ameliorate the cartilage lesion but to make the ankle pain-free and resilient. We recommend NSAIDs, physiotherapy, ice or moist heat applications, well-cushioned shoes, biking, swimming, and cross-training for 6 months.
We allow our adult patients with OLTs activity to tolerance. Immobilization with partial weight bearing has healing potential only for fresh traumatic osteochondral lesions. In an area with little perfusion, some contact pressure is necessary to create a healing response.
We rarely use cast or walker boot immobilization because we believe that ankle motion is important. The occasional cast or boot is applied for only brief periods (2 weeks) to reduce pain and patient insecurity. Cast immobilization is associated with inferior results compared with restricting the activity of the patient by partial weight bearing.24 Flick and Gould10 concluded that therapy of 4 to 6 weeks with cast immobilization is inadequate immobilization, resulting in poor results for most transchondral fractures.
In summary, nonoperative treatment is applied for every patient who is opposed to surgical intervention. There is no time frame when a lesion has to be operated on to prevent deterioration. Pain is the benchmark, not the radiographic or MRI findings. In our opinion, an OLT that is primarily cystic and has an intact cartilage surface suggested on MRI (if detectable) should prompt nonoperative rather than operative management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









