Metaphyseal Engaging Femoral Components
Kamal Bali
Richard McCalden
Douglas D. R. Naudie
Introduction
Total hip arthroplasty (THA) has become one of the most successful orthopedic procedures for managing end-stage arthritis of the hip (1). Implant longevity plays a major role in determining the eventual long-term success of THA, and this is dependent on various factors like surgical technique, implant design, implant material, and the type of fixation. With the introduction of low-friction arthroplasty by Charnley, bone cement became the standard for femoral stem fixation. However, early 1980s witnessed emerging concerns surrounding the use of cement fixation especially in young active patients (2,3,4,5,6). As a result, considerable work has been performed over the last few decades to eliminate the need for cement and to promote cementless biologic fixation of femoral components.
Cementless implants aim to achieve biologic fixation through either bone ingrowth into a porous coating or ongrowth of bone on a roughened (nonporous) surface. The two essential requirements for biologic fixation include immediate mechanical fixation and intimate contact between the implant surface and the viable host bone. As such, the design of a cementless implant is of utmost importance so as to fit the medullary canal of the femur as closely as possible. Also, the femoral endosteal cavity must be prepared to some extent so as to match the implant that is being inserted. Thus, for a cementless femoral fixation, surgical technique and implant design play an important role in eventually achieving the goal of biologic fixation.
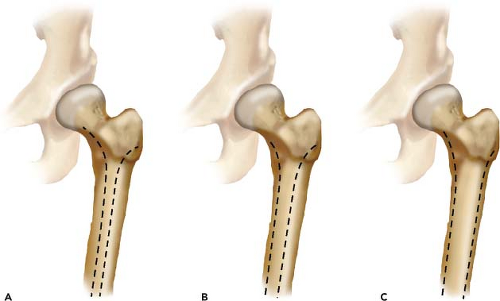
In general, cementless stems are grouped into three broad designs: (a) cylindrical, (b) tapered, and (c) anatomic. In a cylindrical stem, the proximal cross-sectional anatomy is tapered but changes to a cylindrical design in the distal portion of the stem which is fixed in the diaphysis. Tapered stems have a cross-sectional anatomy with a two-dimensional (2D) or three-dimensional (3D) taper over their entire length. The 2D tapered stems have a coronal taper over the entire length with a nontapered rectangular border. The 3D tapered stems are tapered both in the coronal and sagittal planes. The 2D and 3D tapered stems have also been described as flat tapered and double tapered stems, respectively. Anatomic stems may be tapered or cylindrical distally. However, the proximal cross section of anatomic stems has a metaphyseal flare, which is basically a 3D taper that is asymmetric in sagittal and coronal planes and has an anteverted femoral neck.
Different cementless stem designs for primary THA differ not only in shape, but also in metallurgy (titanium alloys vs. cobalt-chrome alloys), type of coating (ongrowth vs. ingrowth), extent of coating (proximal vs. fully coated), and surface properties (hydroxyapatite, sintered beads vs. fiber mesh, plasma sprayed vs. grit blasted). However, it is the geometry of the femoral stem that largely determines the area of fixation within the femoral canal and it is the site of fixation that in turn primarily determines the outcomes (7).
Khanuja et al. (8) have proposed a comprehensive classification of various cementless stems based on their shapes (Figs. 61.1–61.8). This classification system, summarized in Table 61.1, defines six general types of stems and is a modification of the four categories originally described by Berry et al. (7). Types 1 to 5 are essentially straight stems in which the primary fixation area and the amount of osseous contact move from proximal to distal. Type 6 are the anatomic designs and are side specific. This classification system does not include the newer short metaphyseal engaging stems that have been recently introduced into the marketplace. These short metaphyseal stems can be divided into two categories: (a) shortened versions of cementless stems with a standard neck resection and (b) femoral neck sparing (high femoral neck resection designs).
The intent of this chapter is to provide an illustrative description of the design rationale, implantation technique, and results of tapered metaphyseal engaging stems in primary THA. The major focus will be on the single flat and the double wedge design tapered stems, which are arguably the workhorse for today’s cementless primary THA. A brief discussion will also follow on the short metaphyseal stem designs.
Historical Context
The history of successful biologic fixation dates back to the early 1950s with the use of a fenestrated femoral implant developed by Austin-Moore that achieved macrointerlock
with the bone through placement of bone graft within the fenestrations (9). The 1970s saw further experimentation with macroporous stems as well as production of microporous surface implants (10,11). As the understanding of cementless fixation evolved, two basic prerequisites were delineated for achieving biologic fixation: (a) immediate mechanical stability at the time of surgery and (b) intimate contact between the implant and viable host bone.
with the bone through placement of bone graft within the fenestrations (9). The 1970s saw further experimentation with macroporous stems as well as production of microporous surface implants (10,11). As the understanding of cementless fixation evolved, two basic prerequisites were delineated for achieving biologic fixation: (a) immediate mechanical stability at the time of surgery and (b) intimate contact between the implant and viable host bone.
Table 61.1 Classification of Cementless Stems | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In 1983, the Food and Drug Administration (FDA) approved the use of the first cementless femoral stem. This stem, the anatomic medullary locking (AML, Depuy, Warsaw, IN), was a fully porous-coated cylindrical stem that was designed to achieve primarily distal diaphyseal fixation (Type 4 stem). Encouraged by the initial success of this stem design, the hip replacement market was flooded with a plethora of cementless femoral stem designs, which included more anatomically shaped stems that achieved primary fixation by proximal ingrowth.
The AML is a fully porous-coated cylindrical stem made of CoCr with a sintered bead porous surface. The extensively porous-coated stems like AML have a long track record and have been studied more thoroughly than most other cementless stem designs. Various authors have reported excellent long-term survivorship with this stem design (12,13,14,15). Despite good survivorship, these stems have been associated with a high incidence of proximal stress shielding and activity limiting thigh pain, both of which are thought to result from the mismatch of the modulus of elasticity of host bone with the much stiffer CoCr stem. Proximal femoral osteolysis has been seen in as many as 37% of patients (15) and the incidence of thigh pain has been reported to be around 8% (13). Although design modifications have been made in the second-generation type 4 stems (like the Prodigy stem [Depuy, Warsaw, IN] with decreased stiffness), the incidence of proximal stress shielding and thigh pain continues to be a cause of concern with these stem designs (16).
The first generation of anatomic stem designs, which paralleled the evolution of extensively porous-coated stems, in general poorly performed (17,18,19,20,21,22). Most of these were associated with a high prevalence of thigh pain and loosening. Experience in our own institution with the porous-coated anatomical (PCA) stem revealed a very high prevalence of thigh pain (36%) in the 311 PCA hip replacements reviewed with a mean follow-up of 12 years (23). Although various design modifications have been made to obtain a more reliable fixation in these stems, the results have not been uniformly satisfactory and are largely design dependent (24,25,26). Femoral endosteal cavity preparation is also less forgiving with these kinds of stems, which require machining a close match of the shape of the femoral canal to the shape of the implant. The last decade has witnessed a sharp fall in the use of the anatomical femoral components, especially with reports of excellent outcomes with tapered femoral stems.
The tapered cementless stems were designed to provide graduated load transfer to the proximal femur so as to reduce proximal stress shielding, which was common with nontapered designs. The reduced diameter of the distal part of these stems along with use of titanium alloys decreases the stiffness of these stems, helping reduce the incidence of activity-related thigh pain. These stems have so far shown promising outcomes with respect to stem survival and are increasingly the stems of choice for many if not most surgeons performing primary THA (27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50).
Design Rationale for Metaphyseal Engaging Tapered Femoral Components
Tapered cementless femoral stems achieve fixation in two phases. The first stage is the phase of initial mechanical stability. This is achieved with press-fit and three-point self-locking fixation of the tapered femoral stem with posterior contact proximally in the calcar region, anterior contact at the metaphyseal–diaphyseal junction, and posterior contact distally. The second stage of fixation involves osteointegration, which occurs primarily in the metaphysis and is dependent on the presence of a circumferential porous ingrowth or roughened ongrowth surface.
Early mechanical stability minimizing micromotion under load is a prerequisite for implant osteointegration with studies showing that component micromotion of more than 40 μm adversely affects bony ingrowth (51,52,53). When a tapered femoral stem is inserted into the cylindrical medullary canal of femur, it produces hoop stresses in the bone, which leads to press-fit fixation of the stem. By virtue of being viscoelastic, the host bone begins to relax in time. This slowly decreases the press fit of the stem and implant stability at this stage is primarily provided by three-point fixation and the frictional fit of the porous/roughened portion. This initial mechanical stability plays an important role for the first 3 months of implant life. By this time osteointegration usually develops in the porous-coated metaphyseal region and provides eventual long-term biologic fixation to the femoral component.
The tapered design of the stem provides initial axial stability to the implant. This initial axial stability is primarily achieved in the upper diaphyseal region. The initial rotational stability, on the other hand, is primarily achieved in the metaphyseal region of proximally coated stems. Older tapered stem designs, especially the ongrowth titanium stems like the Zweymuller and CLS (Zimmer, Warsaw, IN) were rectangular in cross section and provided initial four-point rotational stability in the diaphyseal region. Wagner (Zimmer, Warsaw, IN) cone type stems are also diaphyseal engaging and have longitudinal flutes that provide initial rotational stability. However, most of the proximally coated stems have polished diaphyseal areas that contribute little to initial rotational stability. Most of these stems (e.g., the Synergy [Smith and Nephew, Warsaw, IN] stem) have wedge-shaped proximal geometries that resist rotation; a few have other additional features like antirotation lateral ridges (for instance, the Taperloc [Biomet, Warsaw, IN] stem).
By virtue of predominant metaphyseal osteointegration, the proximal porous-coated stems create a loading profile designed to decrease the proximal stress shielding observed with extensively porous-coated and stiffer designs (27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50). Also, most of these stems are now made up of titanium alloy with aluminum and vanadium (Ti-6Al-4V). Ti-6Al-4V is almost 50% less stiff than CoCr alloys and this dramatically reduces the incidence of thigh pain (27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50). In addition, Ti alloys can be coated with bioactive hydroxyapatite (HA), which is osteoconductive and promotes osteointegration (54,55,56,57,58). But to date studies have not demonstrated any difference in the long-term outcomes of stems with and without HA coating (59,60,61). In general, fixation surfaces need to be circumferential and continuous. Partially circumferentially coated stems have been found to have higher failure rate (62,63,64,65,66). The circumferentially coated surfaces minimize distal osteolysis by providing a seal against migration of wear particles distally (66,67,68).
Dorr et al. (69) proposed a radiologic classification of proximal femoral bone quality (Fig. 61.9). Dorr type A
femurs have thick medial and lateral cortices with a large posterior cortex giving a champagne flute–like appearance. Dorr type B femurs have bone loss at the medial and posterior cortices resulting in an increased width of the femoral canal. The shape of femur is funnel like and does not compromise implant fixation. Dorr type C femurs give a stovepipe-like appearance indicating complete loss of both medial and posterior cortices with a widened medullary canal. This type of bone is seen in older postmenopausal women. Dorr type A and B bones with tapered medullary shapes are ideally suited for tapered cementless implants; Type C femurs represent a less favorable environment for implant fixation. However, long-term success has been reported in Dorr type C femurs using tapered cementless stems (60,70,71,72).
femurs have thick medial and lateral cortices with a large posterior cortex giving a champagne flute–like appearance. Dorr type B femurs have bone loss at the medial and posterior cortices resulting in an increased width of the femoral canal. The shape of femur is funnel like and does not compromise implant fixation. Dorr type C femurs give a stovepipe-like appearance indicating complete loss of both medial and posterior cortices with a widened medullary canal. This type of bone is seen in older postmenopausal women. Dorr type A and B bones with tapered medullary shapes are ideally suited for tapered cementless implants; Type C femurs represent a less favorable environment for implant fixation. However, long-term success has been reported in Dorr type C femurs using tapered cementless stems (60,70,71,72).
Double Tapered Cementless Stems
Double tapered or 3D tapered cementless femoral stems, often called “proximally porous-coated tapered” stems, are generally straight stems with a proximal to distal taper in both the anterior–posterior (AP) and mediolateral (ML) planes. Unlike the so-called “flat tapered” designs, these stems tend to fill the metaphysis in both the AP and ML planes. Like all cementless femoral stem designs, the goal of these double tapered stems is to obtain both axial and rotational stability leading to eventual osseous integration. By being wedge shaped in both coronal and sagittal planes, these stems obtain both rotational and axial stability within the metaphysis but also obtain overall stability by three-point fixation. Depending on the specific design, additional fixation can be obtained proximally through fins or ribs within the metaphysis or distally by a combination of splines, slots, or flutes, which enhance distal fixation. Almost universally, insertion of these double tapered stems involves a combination of a straight reamer distally and a tapered broach proximally. Because femoral reaming invariably opens up the distal medullary canal, these stems do not carry a risk of “potting” in the diaphysis in Dorr type A femoral morphology, and are ideal stems in these circumstances.
Stem Examples
There are a number of double tapered stem examples, all of which have demonstrated excellent mid- to long-term clinical success. The first of these designs was the Mallory–Head stem (Biomet, Warsaw, IN), which was introduced in the mid to late 1980s. This stem was a titanium proximally porous-coated (plasma-sprayed) long double tapered stem. Other designs have followed, including the Omni-Fit (Howmedica, Rutherford, NJ), the Secure-Fit (Howmedica, Rutherford, NJ), as well as the Synergy stem (Smith and Nephew, Memphis, TN). The Synergy stem was the first of these stems to introduce dual offsets available in all stem sizes. More recently, the Summit stem (Depuy, Warsaw, IN) has been introduced.
Surgical Technique
Preoperative planning plays an important role in THA. Good quality anteroposterior and lateral radiographs are a prerequisite to assess leg length, femoral morphology, level of neck cut, size and offset of the femoral stem. Understanding the anatomic relationship of the greater trochanter with the medullary canal is important to identify an overhanging greater trochanter. This will avoid erroneous medial reaming of the canal intraoperatively that can result in varus stem position and undersizing of the stem. Neck cut can also be adjusted depending upon the preoperative templating. In general, a lower neck cut is required for varus femoral necks and a higher neck cut is needed for valgus neck–shaft angles. Offset estimation can also be done based on preoperative templating.
Insertion of these double tapered cementless stems is relatively straightforward although success is dependent on proper surgical technique. These stems can be inserted through any surgical approach providing one has adequate visualization and access to the proximal femur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree