Chapter 19. Metabolic disease, dysplasias, osteochondritis and neurological disorders
Abnormalities of bone structure
Many disorders of bone occur as a result of the way it is made rather than attack by a disease. These conditions are complex, but learning can be simplified by looking at the different components of bone and the factors that influence their growth.
Bone growth is influenced by the following hormones and vitamins:
Factors affecting bone growth
Factors affecting bone growth
1. Growth hormone.
2. Sex hormones.
3. Thyroid hormones.
4. Parathyroid hormone.
5. Vitamin C.
6. Vitamin D.
7. Calcitonin.
Growth hormone is responsible for growth until the epiphyses close. Excess secretion after growth is complete causes the thickening of the bones seen in acromegaly; excess secretion before growth is complete causes gigantism.
Sex hormones are involved in the growth spurt of puberty. Release of testosterone causes a rapid increase in growth followed by epiphyseal closure. If testosterone is not released, the epiphyses grow for longer than normal and the patients are tall; hence the legendary giant eunuchs.
Thyroid hormone permits normal growth and deficiency retards it, which is the reason that hypothyroid cretins are small. Thyrotoxicosis does not cause an increase in size but can lead to osteoporosis.
Parathyroid hormone is a polypeptide released when the serum calcium falls. Parathormone acts to increase the serum calcium in two ways:
1. Mobilization of calcium from bone.
2. Increased tubular resorption of calcium.
Vitamin C is necessary for collagen synthesis. Without it, osteoid cannot be properly formed at the epiphyses and children with scurvy have transradiant bands at the epiphyses.
Vitamin D has three actions:
1. It is essential for the absorption of calcium from the gut.
3. It affects muscle tone; patients with vitamin D deficiency have muscle weakness.
Calcitonin is secreted in the thyroid. Its exact function is unclear but it is secreted if the serum calcium is high and it affects release of calcium from bone.
Bones have four main constituents which can affect growth. Disorders of growth can be considered according to the structure affected (Fig. 19.1).
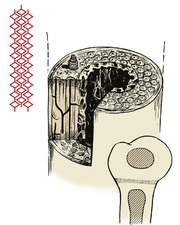 |
| Fig. 19.1 Constituents of bone. Bone consists of crystals arranged along collagen fibres, cartilage, and osteons or haversian systems. |
Constituents of bone
1. Collagen.
2. Crystals of calcium hydroxyapatite arranged in an orderly manner along the collagen fibres. Osteoid is the uncalcified precursor of normal bone.
3. Osteons. Long bones are made up of long tubular units – the haversian systems or osteons. The osteocytes lie in cavities inside dense cortical bone and communicate with other osteocytes by prolongations of the cell body which run through canaliculi. This contact enables the osteocytes to react to abnormal stresses.
4. Cartilage. Growing bones develop from cartilage, which contains proteoglycans.
Abnormalities of collagen
Scurvy
The manifestations of scurvy include abnormal calcification at the epiphyses, and capillary fragility which leads to subperiosteal haemorrhage.
Treatment. Ascorbic acid (vitamin C).
Osteogenesis imperfecta
Osteogenesis imperfecta, or fragilitas ossium, is often sporadic, but can be inherited through either autosomal recessive or autosomal dominant genes (Fig. 19.2). Although the brittleness of bone is the most obvious feature, it is essentially a disorder of type 1 collagen synthesis.
 |
| Fig. 19.2 Gross osteogenesis imperfecta. |
There are four common types:
Type 1. Mildest form with fractures in childhood but less frequent with age. Patients have a slight blue discoloration to the sclera of the eyes. Hearing loss is common in adults.
Type 2. Most severe form with patients having fractures in utero or being stillborn.
Type 3. Severe. Frequent fractures in childhood and adults. Short stature, hearing loss and blue sclera common. Patients will often also have problems with their teeth development.
Type 4. Moderate form with fractures in child and adulthood. Sclera are often white but there is often hearing loss, short stature and possible teeth problems.
The brittleness of the bones is only part of the syndrome (Fig. 19.3). The teeth may also be affected and are often discoloured and abnormally thick – dentogenesis imperfecta. The ground substance in the sclerae of the eye may be abnormal, so that the retinal pigmentation is seen through the sclerae, producing a characteristic bluish discoloration. This is characteristic of the condition but not present in every patient. Mutations in the COL1A1, COL1A2, CRTAP and LEPRE1 genes appear to be the cause.
 |
| Fig. 19.3 (a), (b) Fractures in osteogenesis imperfecta (note the bowing). (c) Gross bowing of the femora in osteogenesis imperfecta. |
Bones affected by osteogenesis imperfecta are more plastic than normal and bowing is a recurring problem needing correction by multiple osteotomy and internal fixation.
There are three grades of severity:
1. Some patients are so badly affected that they have multiple fractures in utero and do not survive.
2. Others have multiple fractures during childhood and develop a pigeon chest and scoliosis.
Although fragilitas ossium does occur, many parents believe that their accident-prone children must have a bony abnormality to account for their fractures and require firm reassurance. In other patients the diagnosis of a non-accidental injury must be considered.
Abnormalities of mineralization
Bone loss
Bone can be lost in three ways:
1. Osteomalacia – decreased mineralization.
2. Osteolysis – increased removal by osteoclasts.
3. Osteopenia – decrease in osteoid tissue. In practice, ‘osteopenia’ is more often used in the description of radiologically thin bones without implying a specific cause.
These three processes usually occur together in varying degree. The resulting loss of bone is called osteoporosis, of which there are three common types:
1. Idiopathic osteoporosis.
2. Disuse osteoporosis.
3. Steroid osteoporosis.
Idiopathic osteoporosis
Lack of oestrogen causes a reduction in the amount of collagen in the bones of postmenopausal women, which become thin and ‘porotic’. Affected bone, particularly cancellous bone, is weaker than normal and susceptible to fractures (Fig. 19.4). Fractures of the femoral neck and crush fractures of the vertebrae are common after trivial injuries in elderly women with senile osteoporosis.
 |
| Fig. 19.4 Osteoporosis with crush fractures of the lumbar vertebrae. |
Clinical and radiological features. The patients experience pain in the bones, especially the back. A kyphosis gradually develops. Radiologically, the bones look ‘thinner’ than normal and pathological fractures may be present.
Treatment. The treatment of osteoporosis is generally unsuccessful because the condition takes so long to appear that, by the time it is recognized, it is too late to treat it. If recognized early, hormonal treatment can be instituted, which can, at best, reverse the osteoporosis and restore normal bone texture.
The first line of treatment has been hormone replacement therapy (HRT) with special emphasis on oestrogen. The second line is low dose bisphosphonates (etidronate) given intermittently.
The ideal treatment has yet to be found but there has been a drive to make people and clinicians aware of the problems. Screening programmes have been started and these will hopefully allow earlier detection; this, together with the newer treatments, may help reduce the morbidity suffered by patients.
Disuse osteoporosis
Disuse osteoporosis is seen in bones that are not stressed normally. Patients confined to bed are particularly affected, as are paralysed limbs and fractures that are treated as non-weight-bearing. Astronauts undergo gross disuse osteoporosis.
Treatment is by mobilization and load-bearing.
Steroid osteoporosis
Steroid osteoporosis is seen in patients receiving large doses of steroids for rheumatoid arthritis or following transplantation, and in Cushing’s disease. The consequences include pathological fractures and vertebral collapse.
Treatment is by reducing the dose of steroids or treating the underlying disorder.
Rickets
Rickets is due to deficiency of calcium and phosphate in childhood (Fig. 19.5). Although much less common than in former times, rickets still occurs widely in developing countries. There are four causes:




1. The commonest is vitamin D deficiency due to inadequate diet or lack of natural vitamin D from exposure to sunlight.
2. Malabsorption of calcium due to steatorrhoea.
3. Renal osteodystrophy due to renal abnormality, which affects vitamin D metabolism and causes renal failure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








