Meniscus Allografts
Walter R. Shelton MD
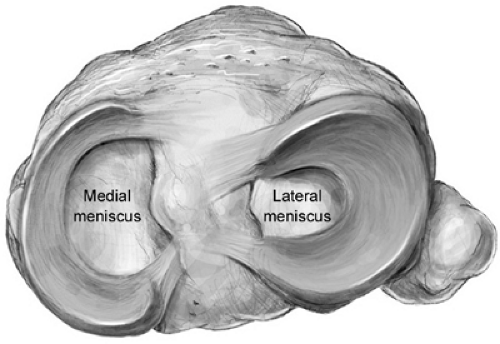
The medial meniscus is a C-shaped triangular structure that is relatively more fixed than the lateral meniscus and is thicker posterior than anterior. The lateral meniscus is semi-circular, uniform from anterior to posterior, and more mobile.
Candidates for meniscal allografts should be under 45 years old and have persistent pain after at least six months of conservative treatment following meniscectomy. The pain is usually oriented toward the side where the meniscus was removed.
Extremity alignment and range of motion are critical when considering meniscus allograft surgery. Any abnormal valgus or varus or significant limitation of flexion or extension should be corrected prior to meniscus surgery.
A cruciate deficient knee provides an opportunity to replace both the ligament and the meniscus with one surgery.
Patients over age 45, with grade 4 arthritis, or with little or no pain are better suited for long-term conservative treatment.
Meniscus allograft transplantation is a formidable procedure and complications can be significant. Deep vein thrombosis, post-surgical infection, and damage to articular surfaces are possible. Allografts also have the potential to transmit infectious diseases.
Long-term data supporting the concept that a meniscus allograft will decrease the incidence of degenerative arthritis seen after meniscectomy is not yet available.
Many insurance carriers still consider meniscal allograft surgery to be an experimental procedure and refuse to approve reimbursement.
In rehabilitation, patients are started on full range of motion immediately. Patients usually go to one crutch at three weeks and are off crutches at six weeks, but are cautioned to avoid jumping, cutting, or running sports for at least six months.
The anatomy of both the medial and lateral menisci have been well documented over the last 25 years. Recognition of their critical function of load distribution from femur to tibia has promoted investigation into every aspect of their makeup. The medial meniscus is a C shaped, triangular structure that is relatively more fixed than its counterpart and is thicker posterior than anterior (Fig 39-1). The lateral meniscus is semi-circular, uniform from anterior to posterior, and is more mobile. Both menisci attach to bone posteriorly
at the back edge of the tibial spine. Anteriorly the medial meniscus inserts at the front edge of the tibial plateau; the lateral meniscus’ anterior insertion is more posterior, opposite the anterior cruciate ligament (ACL) footprint. The lateral meniscus’ capsular attachment is interrupted by the popliteus tendon in the posterolateral aspect of the joint.
at the back edge of the tibial spine. Anteriorly the medial meniscus inserts at the front edge of the tibial plateau; the lateral meniscus’ anterior insertion is more posterior, opposite the anterior cruciate ligament (ACL) footprint. The lateral meniscus’ capsular attachment is interrupted by the popliteus tendon in the posterolateral aspect of the joint.
Both menisci play a critical role in load-bearing and weight distribution from a relatively circular femoral condyle to a more flat tibial plateau. Pressure studies have shown that with normal menisci the load transmitted from the femur to the tibia throughout a full range of motion is evenly distributed over the tibial plateau. The lateral meniscus carries 70% of the load across the lateral compartment while the load is shared equally between meniscus and articular cartilage in the medial compartment. (The lateral meniscus is much more mobile than the medial meniscus.) (1) After meniscectomy the stress is highly concentrated toward the center of the tibial plateaus (2).
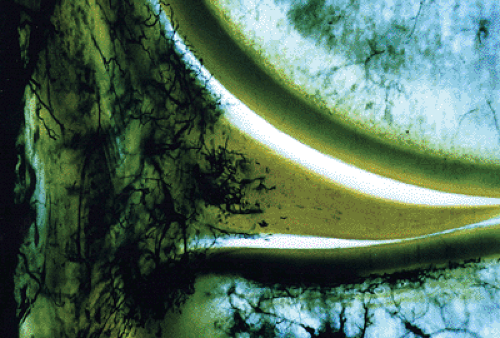
Most of the meniscus is composed of water. The remainder is made up of cells known as fibrochondrocytes and an extra-cellular matrix of proteoglycans. Blood supply of both menisci have been well documented by Arnoczky (Fig 39-2) and are composed of an outer one third that has an excellent blood supply (the red/red zone), a middle third where the blood supply becomes sparse (the red/white zone), and an inner third that is avascular (the white/white zone).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree