CHAPTER 8 Meniscal Transplantation
Surgical treatment of meniscus lesions has changed significantly over time. Meniscal tears were traditionally treated with meniscal excision, but it became understood that loss of the meniscus alters the biologic and biomechanical environment of the knee.1,2 The resulting degenerative changes in the involved compartment led us away from meniscus removal and toward meniscus preservation. Partial meniscectomy and meniscus repair procedures have become the standard of care. For patients for whom meniscal preservation is not an option, meniscal allograft transplantation can be done for a select subset of patients who have become symptomatic from their meniscal deficiency. This offers restoration of anatomic and biomechanical function.
ANATOMY
The menisci are semilunar-shaped fibrocartilaginous structures that function in shock absorption,3 load transmission,4–6 secondary mechanical stability,7,8 joint lubrication,9 and nutrition.10 Circumferentially oriented collagen fibers provide resistance to hoop stresses whereas radially oriented fibers hold the circumferential fibers together and provide resistance to shear.11,12 The anterior and posterior horns attach to bone by interdigitating collagen fibers oriented to transmit load and shear optimally from the meniscus to the tibia.13
The menisci are composed of 74% water,14 allowing for optimization in force transmission. The lateral meniscus carries 70% of the lateral compartment load, compared with 50% by the medial meniscus.6,15 The menisci transmit 50% of the joint load when in knee extension and 90% when the knee is in flexion.6,15 Loss of the meniscus, therefore, increases the load on the articular cartilage surfaces and facilitates the development of early degenerative changes. Loss of just 16% to 35% of the meniscal tissue can lead to a 350% increase in contact forces.4 Clinical studies support meniscus preservation, because a greater size of meniscal resection is associated with a poor clinical outcome.16–19
PATIENT EVALUATION
Physical Examination
Examination often reveals full range of motion. Depending on recent activity, a joint effusion may be present. Joint line or femoral condyle tenderness is occasionally found. A thorough physical examination is essential to reveal malalignment, ligament deficiency, or articular cartilage lesions that would modify the treatment plan. These findings need to be addressed, either as a concurrent or staged procedure.
TREATMENT
Indications and Contraindications
Although not absolute contraindications, chondral defects, malalignment, or ligamentous instability all require consideration for concurrent or staged procedures to ensure that all joint pathology is addressed. In the past, full-thickness chondral defects were considered a contraindication; however, cartilage degeneration is not a significant risk factor for meniscal allograft failure.20 Outcomes of many concurrent procedures, including meniscal transplantation with concurrent autologous chondrocyte implantation (ACI)21,22 and osteochondral allograft32 have shown excellent results in the carefully selected patient.
Concurrent or staged corrective osteotomy is indicated for patients with deviation toward the involved compartment. Axial malalignment can exert abnormal pressure on the newly placed graft, which can lead to loosening, overload, degeneration, and failure.23–25
Anterior cruciate ligament (ACL)–deficient patients who have had a prior medial meniscectomy may benefit from concomitant ACL reconstruction (ACLR) and meniscal transplantation. Many studies have shown that meniscectomized ACL-deficient knees lead to worsening degenerative changes. The more aggressive approach of combination ACLR and meniscal transplantation has good long-term follow-up as opposed to untreated (left alone) knees. In addition, the posterior horn of the medial meniscus is an important secondary stabilizer to anterior translation and may be important in preventing secondary “stretch” of the ACL reconstructed knee.7,26–28
Conservative Management
Patients who have had a prior meniscectomy should have a trial of conservative treatment before consideration of operative measures. Activity modifications, anti-inflammatory medications, and occasionally injections can be recommended to help determine which patients can function without surgical intervention. More aggressive management of the relatively young patient following lateral meniscectomy might be considered, especially in female athletes with slight valgus who are at significant risk for the development of progressive lateral compartment arthritis.29
Arthroscopic Technique
Preoperative Planning
Allograft Sizing.
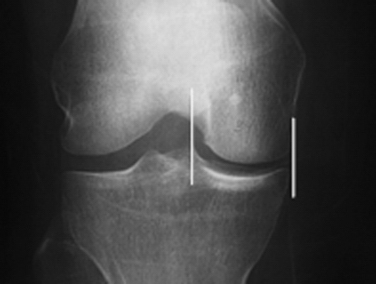
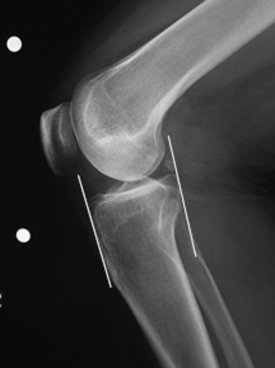
The success of meniscal transplantation is dependent on careful size matching of the meniscus allograft to the native meniscus. Meniscal allografts are compartment- and size-specific. Anteroposterior and lateral preoperative radiographs with sizing markers are important for meniscal sizing (Figs. 8-1 and 8-2). Allograft sizing is of significant importance, because oversized meniscal allografts lead to greater forces across the articular cartilage.30 On the other hand, undersized allografts result in greater forces seen by the meniscal tissue.30 The meniscus width is determined on the AP radiograph by measuring from the edge of the ipsilateral tibial spine to the edge of the tibial plateau. Meniscal length is determined on the lateral radiograph as determined by the AP dimension of the ipsilateral tibial plateau. These measurements, after correction for magnification, are multiplied by 0.8 for medial and 0.7 for lateral meniscus. Other methods using height and weight have been proposed, but are not routinely used.31,32
Meniscal Graft Processing and Preservation.
Meniscal allografts are harvested using sterile surgical technique ideally within 24 hours after death and frozen to −80° C. Although other graft preservation methods are used, including secondary sterilization methods, fresh-frozen grafts remain the most commonly used allograft preservation method.33–35
Stringent donor selection is based on comprehensive medical and social history. The risk of disease transmission is further reduced by screening for human immunodeficiency virus (HIV), human T-cell lymphotropic virus (HTLV), hepatitis B and C, and syphilis. Blood cultures for aerobic and anaerobic bacteria, as well as lymph node sampling, may be performed. Graft processing, including débridement, ultrasonic-pulsatile washing, and use of ethanol to denature proteins, further lowers the risk of disease transmission.36
Surgical Anatomy, Incisions, and Portals
Important surgical landmarks to be identified are the patella, patellar tendon, tibial plateau, and fibular head. Portals and incisions include inferomedial and inferolateral arthroscopy portals, an accessory outflow portal, a posterolateral or posteromedial incision, and a miniarthrotomy adjacent to or splitting the patellar tendon on the transplant side (Fig. 8-3).
Caution should be taken while making incisions because many structures are at risk, depending on the approach. These include the peroneal nerve and lateral collateral ligament with the posterolateral approach, the saphenous nerve and medial collateral ligament with the posteromedial approach, and the patellar tendon with the anterior miniarthrotomy. In addition, the posterior neurovascular bundle can be damaged during needle passage when suturing the meniscus in place, especially on the lateral side.