CHAPTER 6 Meniscal Resection
ANATOMY
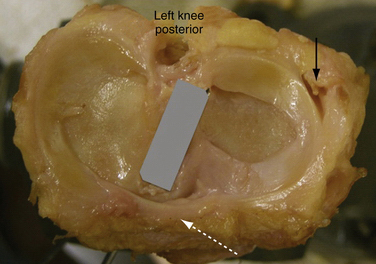
Menisci are discs of fibrocartilage interposed between the femoral condyles and tibial plateau. The articular surface of the medial condyle of the tibia is oval, with the longer axis being in the anteroposterior plane (Fig. 6-1). The central portion of the articular surface is not covered by meniscus and represents the articular area. The lateral meniscus plateau is almost circular and less concave. The menisci cover the peripheral two thirds of the tibia, and serve to deepen its articular surface and stabilize the joint. The upper borders of the menisci are concave and the undersurfaces are flat. Peripherally, the menisci thicken and are attached to the synovium and capsule. Centrally, the border is thin and exists as a free edge.
The medial meniscus is oval, 3.5cm in length, and wider posteriorly from its peripheral to its central aspects in the knee. Its anterior horn attaches to the tibial plateau just anterior to the attachment of the ACL. Some posterior fibers originating from the anterior horn cross the knee joint anteriorly, attaching to the lateral meniscus and forming the transverse ligament (see Fig. 6-1). Posteriorly, the meniscus is anchored to the intercondylar fossa of the tibia between the posterior cruciate ligament (PCL) and lateral meniscal attachment. Along its periphery, the medial meniscus is attached to the joint capsule and the deep medial collateral ligament (MCL). The medial meniscus has less mobility than the lateral meniscus, and moves almost 10 mm from extension to flexion.
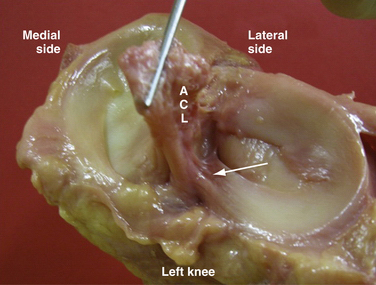
The lateral meniscus is circular, covering a larger portion of the articular surface than its medial counterpart. It is the same width anteriorly and posteriorly. The anterior horn attaches near the intercondylar spine posterior to the attachment of the ACL, with which it partially blends (Fig. 6-2). The posterior horn attaches just posteriorly to the intercondylar spines, anterior to the attachment of the medial meniscus. The lateral meniscus does not attach to the lateral collateral ligament but is attached loosely to synovium along much of its length. The anterior (ligament of Humphrey) and posterior (ligament of Wrisberg) meniscofemoral ligaments run from the posterior horn of the lateral meniscus to anterior and posterior, respectively, to the PCL attachment on the medial femoral condyle. Moreover, the tendon of the popliteus muscle, on its way to insert into the lateral condyle, crosses the joint through a hole on the lateral meniscus called the hiatus popliteus (see Fig. 6-1). This area along the popliteal hiatus is described as the avascular region.
Biomechanics and Meniscal Function
A complete meniscectomy has been shown to decrease the contact area by approximately 50%.1 A partial or total meniscectomy has been clinically demonstrated to result in degenerative changes in the knee.2 This has been postulated to result from the increase in contact pressures in the knee. Even a minor meniscectomy, removing 15% to 34% of the meniscus, increases contact pressures in the knee by up to 350% and can result in degenerative changes. In meniscectomized knees, a significant reduction in contact area of about 55% is observed, and peak contact pressures increase an average of 260.4% compared with those of nonmeniscectomized knees.3
Knee joint stability is enhanced by the menisci in a similar manner to the glenoid or acetabular labrum. The intact meniscus serves as a secondary restraint to anteroposterior knee motion.4 The ACL-deficient knee can place abnormal stress on an intact medial meniscus, resulting in a meniscal tear. The increased anteroposterior motion created by meniscectomy in the ACL-deficient knee can lead to increased instability.
Regenerative Capacity of the Meniscus
King’s 1936 experiment on a canine model represents the historical origin of the interest in meniscal healing.5 Later experimentation demonstrated the necessity of a peripheral blood supply to support the inflammatory cascade required for meniscal healing.6
Studies have shown that when a radial tear extends into the synovium, it can heal spontaneously by 10 weeks.7 The strength of this tissue is 33% normal at 8 weeks, 52% at 4 months, and 62% at 6 months. It is this inherent healing ability of the meniscus that clinical initiatives exploit in efforts to preserve as much meniscal tissue as possible.
CLASSIFICATION
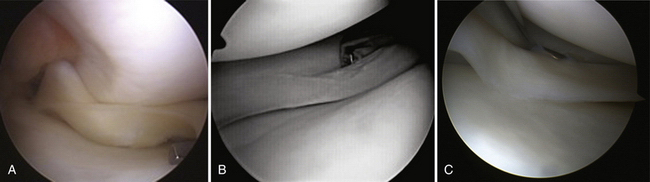
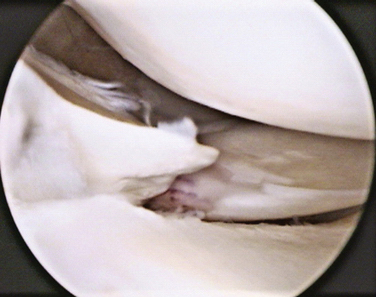
In addition, meniscal tears can be classified depending on their stability (Box 6-1). A tear is considered unstable when it is more than half the length of the meniscus and subluxes under the femoral condyle when probed with a hook (Fig. 6-3A). This concept is especially important to help decide the treatment options—left alone, trephinated, resected, or repaired.
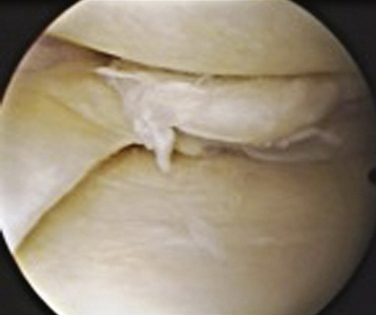
Stable tears, which occur particularly in the posterior aspect of the meniscus and do not subluxate into the joint may be left alone (see Fig. 6-3B and C). Fitzgibbons and Shelbourne8 have found that of 189 patients whose stable meniscal tears of the posterior horn of the medial meniscus were left alone, no patient was symptomatic at 2.6 years following surgery. Also, a stable longitudinal tear of the lateral meniscus, posterior to the popliteus, may be left alone, even in association with a torn ACL.
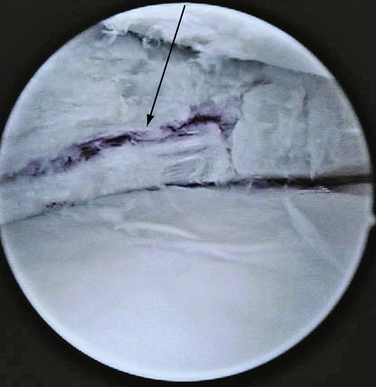
Tears can be described depending on their morphology and based on their configuration. Under these criteria, tears could be vertical or horizontal, according to whether the line of the lesion goes from superior to inferior (vertical) or from inside to outside (horizontal), commonly called open book or fishmouth tear (Fig. 6-4). Moreover, tears can be described as longitudinal if the pattern is from anterior to posterior (Fig. 6-5; also see Fig. 6-3), or transverse, also called a radial or parrot beak tear (Fig. 6-6). Combinations of these four basic patterns make up the others types of tears; the oblique tear is vertical and radial, and the so-called bucket handle tear is a vertical longitudinal tear that is unstable and subluxes completely under the condyle (Fig. 6-7; also see Fig. 6-3A). Finally, the complex tear is a combination of all of these, usually in a degenerative setting, located in the posterior horn of the medial meniscus (Fig. 6-8).
Horizontal-shaped tears usually begin as intrasubstance degeneration in the middle of the meniscus, and migrate toward the free surface. Often, they also extend to the capsular junction and can cause the formation of a cyst. Because of the increasing size of the cyst over time, the patient may experience pain and tenderness. They usually appear more frequently in the lateral meniscus and are filled with a gel-like substance chemically similar to synovial fluid. These cysts have been reported to be 1% to 10% of meniscal pathology.9
Complex tears appear mainly in older patients and are usually associated with cartilage degeneration. They are considered to be part of the process of arthrosis and degenerative arthropathy. Because of their complex pattern, the fragments can be unstable and cause mechanical symptoms. The pain associated with these tears is an added element to the generalized inflammation involved in the osteoarthritic knee. The associated histologic pathology is myxoid degeneration, hyaline acellular degeneration, and dystrophic calcification.10
Finally, tears can be classified depending on the side—that is, the medial or lateral meniscus. Metcalf and colleagues11 have observed that 69% of tears affected the medial meniscus, whereas the lateral was affected 24% of the time. In their review, both menisci were torn at the same time in 7% of patients. Moreover, 80% of the tears were vertical or oblique and affected the posterior medial part of the meniscus.
In summary, the most common meniscal tears are as follows:
PATIENT EVALUATION
Physical Examination
The patient is examined for signs of an effusion, loss of quadriceps bulk, and decreased range of motion. Tenderness to palpation along the medial or lateral joint line is among the most sensitive signs of a meniscal tear (Fig. 6-9A). Studies have shown it to be as sensitive as 74%, with a positive predictive value of 50%.12 The collateral and cruciate ligaments need to be assessed to determine whether additional injury is present. In the setting of an ACL-deficient knee the sensitivity of joint line tenderness has been shown to decrease to approximately 50%.
The McMurray test is preferred because it is easy, fast, and reliable. In addition, complementary knee tests may be done in the same position. This provocative test is performed with the patient supine, the hip flexed to 90 degrees, and the knee in forced maximal flexion. The foot is grasped by the heel, the knee is steadied, and the joint line is palpated with the other hand. As the knee is slowly brought into extension, an external rotation stress will test the medial meniscus and an internal rotation stress will test the lateral meniscus (see Fig. 6-9B). As a mnemonic rule, the heel of the foot points toward the injured meniscus. The test is considered positive when the patient feels pain in the appropriate joint line, accompanied by a thud or click. When the clunk is present, the test has a sensitivity of 98% but, because it is not always possible to evoke the clunk, its specificity is only 15%.13
In conclusion, the hallmarks of a meniscal tear are presence of an effusion, joint line tenderness, and a positive McMurray test. When the history and physical examination are considered together, the overall sensitivity to diagnose a meniscal tear, confirmed with arthroscopy, is approximately 95% and specificity is 88%.14
Diagnostic Imaging
Evaluation of the patient with a meniscal tear should include routine anteroposterior (AP) and lateral x-rays of the knee. If degenerative changes are expected, standing views, including a 45-degree flexion AP view, should be obtained to assess the degree of joint space narrowing. Assessing osteoarthritis is important to counsel the patient about expectations of success. It has been proven that the degree of arthrosis before surgery correlates with worse postoperative results in the short- and long-term periods.15,16
Although not clinically indicated for all patients, magnetic resonance imaging (MRI) plays a valuable role in the evaluation of the full range of meniscal pathology, including the primary diagnosis of a meniscal tear, detection of a recurrent tear after resection or repair, and demonstration of associated injuries. MRI shows the relative locations of the tears, and is able to determine the presence of a meniscal tear with an accuracy of over 90%.17 These results indicate that MRI is an accurate noninvasive technique for evaluating meniscal tears.
Image results should be combined with pertinent history and physical examination. It has been proven that meniscal tears in young adults can be completely asymptomatic.18 In these cases, MRI may modify the therapeutic plan. For example, if an athlete suffers an ACL during the season and the MRI demonstrates no tear, one may be inclined to let the athlete finish the season with a brace. If there is a meniscal tear associated with the ACL tear, the preference would be for early reconstruction.
TREATMENT
Indications and Contraindications
Meniscectomy is indicated when the type of tear has no chance to heal spontaneously or repair is not possible. Although technology is improving and the indications for repair are increasing, arthroscopic partial meniscectomy is currently still indicated in 80% of tears (Table 6-1).
TABLE 6-1 Indications for Meniscectomy: Situations in Which Meniscectomy Is Preferred Over Repair
| Factor | Features |
|---|---|
| Meniscal Tear Factors | |
| Location | White-white |
| Morphology | |
| Size | >20 mm |
| Chronicity | >8-12 wk |
| Patient Factors | |
| Age | >40 years old |
| ACL acute deficient knee | Small posterior flap tear in lateral meniscus |
| ACL chronic deficient knee | All types of tears |
| Rehabilitation | Noncompliant patient |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree