16. Meningitis
Bacterial meningitis
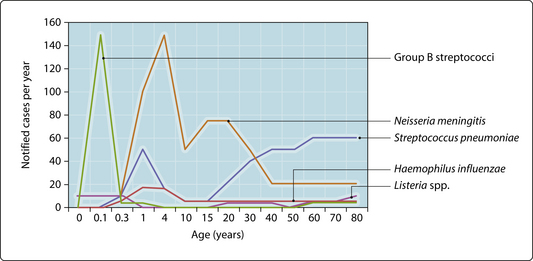
In contrast to viral forms, bacterial meningitis may be life threatening and have serious sequelae for those who survive. While it may be impossible to predict the causative agent from the clinical features, some pathogens are more common at certain ages (Fig. 3.16.1). Neonatal meningitis may be early (within 7 days of birth) or late (occurring between 1 week and 3 months) onset. Early infections are acquired from the mother, whereas late infections may result from cross-infection after birth. The commonest causes of early-onset disease are group B β-haemolytic streptococci and coliforms such as Escherichia coli. Listeria monocytogenes and group B β-haemolytic streptococci can cause late-onset disease. Most bacterial meningitis occurs in childhood. The introduction of Hib vaccine against type B strains of Haemophilus influenzae has significantly reduced the incidence of invasive infections caused by this organism. The commonest cause is now Neisseria meningitidis. The three common serotypes A, B and C vary in prevalence, but B and C are commonest in western Europe and A in Arabic countries. The introduction of conjugated meningococcal C vaccine in the UK significantly reduced the incidence of meningococcal meningitis. Meningitis caused by Streptococcus pneumoniae occurs at all ages but particularly in children under 2 years, the elderly and those with immune defects (e.g. HIV infection, sickle-cell disease and postsplenectomy). Meningitis in adolescents and young adults is most commonly caused by meningococci. In later life, pneumococci are more likely. L. monocytogenes is a relatively rare cause but should be considered particularly in pregnant and immunocompromised patients. Tuberculous meningitis occurs more commonly in immigrants from developing countries.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree