Megaprosthesis of the Knee for Non-Neoplastic Conditions
Bryan D. Springer
The primary use for megaprostheses about the knee has been for reconstruction of the distal femur and proximal tibia after resection of a neoplasm (1,2,3,4). Complex primary and revision total knee arthroplasty (TKA) in patients with massive bone loss, ligamentous instability, or both is a significant challenge. Prosthetic knee design with articular constraint often is needed and hinged knee implant may be required in complex situations (5,6,7).
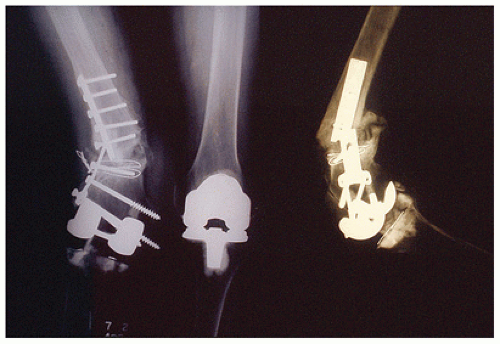
Previous fixed hinge designs have been associated with high failure rates because of increased transmission of stress to the bone-cement interface (Figs. 15.1 and 15.2) (8). With the advent of a rotating hinge design, the rotational freedom allows for dissipation of stresses from the bone-cement interface and a more anatomically matched prosthesis (9,10,11). The purpose of this chapter is to evaluate the current indication, surgical techniques, and results of a megaprosthesis of the knee in nonneoplastic conditions.
INDICATIONS
Megaprosthetic replacement of the knee is utilized as a salvage procedure for complex primary or revision TKA. The use of a megaprosthetic component in primary and revision knee surgery is relatively uncommon. Reports in the literature range form 0.14% to 13% of all revision knees (12, 13).
The ideal candidate for the use of a megaprosthesis is an elderly, low-demand patient with extensive distal femoral or proximal tibial bone loss. These patients may benefit substantially from early mobilization. Cemented megaprosthetic replacement allows for immediate weight bearing and transfers as early as postoperative day 1. Specific indications include
Limb salvage following periarticular tumor resection
Severe bony deficiency with associated collateral ligament disruption
Extensor mechanism disruption
Significant flexion and extension gap mismatch
Acute treatment of supracondylar femur fractures with substantial bone loss in elderly patients
Treatment of periprosthetic fractures about the knee with associated severe bone loss and/or poor bone quality (osteoporosis) in low-demand patients (Fig. 15.3)
Salvage of previous nonunion/malunion of periprosthetic fracture about the knee (Fig. 15.4)
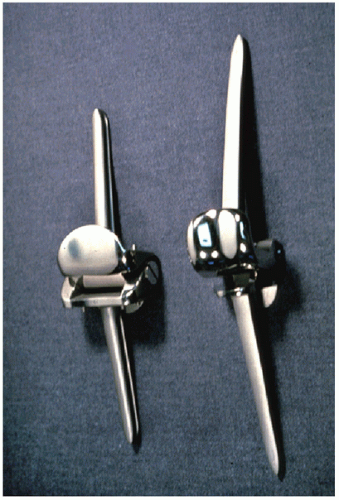 FIGURE 15.1 Early hinge designs were fixed hinges that only allowed motion in flexion and extension. |
CONTRAINDICATIONS
Contraindications for the use of megaprosthetic replacement in TKA include
Patients medically unfit to undergo surgery
Active infection of the limb
Poor soft tissue coverage
Higher demand patients in whom the limb can be reconstructed with allograft or standard primary or revision components
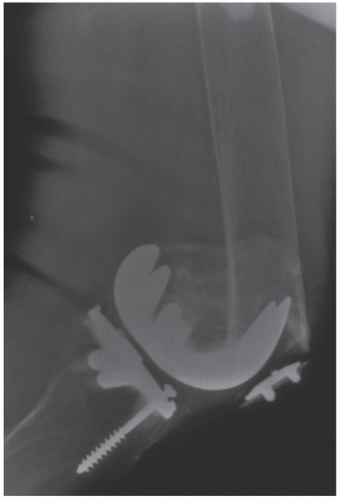 FIGURE 15.3 Distal femoral periprosthetic fracture above a TKA. The bone is of poor quality (osteoporotic) and there is little remaining host bone to allow for distal fixation. |
PREOPERATIVE PREPARATION
As with any primary or revision TKA, preoperative planning is essential.
Imaging
Appropriate radiographs should include a standing anterior-posterior view, lateral view and merchant view. Each of these x-rays should be evaluated to assess bone loss and quality of remaining host bone. In addition, a long leg hip to ankle view may be utilized to asses the overall mechanical alignment of the extremity and to asses for other hardware that may interfere with placement of a long stemmed hinged TKA (e.g., total hip arthroplasty above a TKA). Preoperative examination should include
Examination of skin for color, temperature changes and effusion that would indicate infection
Evaluation of old incisions
Vascular and neurologic status of the limb
Range of motion
Collateral ligament stability
Function of the extensor mechanism
Recurvatum deformity
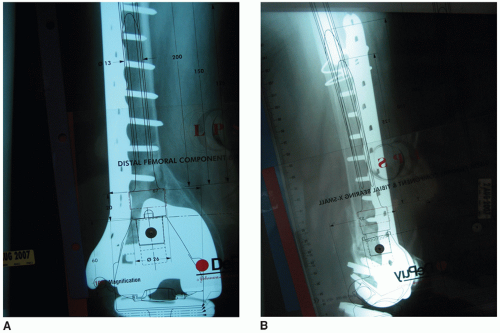 FIGURE 15.5 A,B: Preoperative templating to determine length of distal femoral resection as well as length and diameter of intramedullary stems is a crucial part of preoperative planning. |
Templating of both the femoral and tibial components are mandatory. In addition to estimating the size of the components, templating is utilized to estimate bone resection levels and the need for augmentation as well as the length, position, and size of intramedullary stems (Figs. 15.5 A,B).
TECHNIQUE
Position and Draping
Patients should be placed supine on the operative table and all bony prominences well padded. A nonsterile tourniquet can be placed proximally on the upper thigh. The positioning should allow for free mobility of the operative limb throughout the full range of flexion and extension. A leg positioner should be used to allow the knee to flex and rest at 90 degrees and to assist in femoral and tibial preparation. In cases where large resections of the distal femur or proximal tibia are required, the entire extremity to include the groin and pelvis should be prepared and draped free.
Incision and Exposure
The approach to the knee is determined by the previous surgical incisions and the condition of the soft tissue around the knee. Whenever possible, prior incision should be utilized. When multiple incisions are present, use the most laterally based incision. Any flaps that are created should be full thickness to avoid compromise of the blood supply to the skin. Standard medial parapatellar approach or extensile exposures may be required. Once exposed, removal of the failed tibial and femoral components should proceed, preserving as much of the remaining bone as possible. Remove all cement and debris and debride all bony surface down to good quality bone.
Tibial Preparation
Prepare the tibial canal and establish a proximal tibial supportive bony platform perpendicular to the mechanical axis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree