Megaprosthesis after Tumor Resection
Peter F.M. Choong
The femur is a common site for primary and secondary malignancies of bone. In the majority of cases, proximal and distal tumors can be adequately treated by wide resection and prosthetic reconstruction utilizing proximal or distal femoral prostheses. Extensive tumor involvement, however, can give rise to a challenging surgical situation where wide resection of bone is likely to leave insufficient residual bone for safe and stable fixation of standard proximal or distal femoral prosthetic replacements. The minimum length of proximal or distal femur required for fixation of a tumor endoprosthesis is approximately 130 mm. Therefore, extension of a distally located tumor above the lesser trochanter or a proximally located tumor below the diaphysiometaphyseal junction of the distal femur is unlikely to leave adequate bone stock for stem fixation. Diaphyseal tumors such as Ewing sarcoma can also be so extensive as to involve both proximal and distal parts of the femur requiring total femoral resection for safe removal.
Previously, extensive femoral tumor that would normally require total or near total femoral resection would be treated by hip disarticulation. In comparison to femoral resection and reconstruction, hip disarticulation is simpler and the risk of violating tumor margins is considerably less. To reduce the impact of hip disarticulation, biologic reconstructions have been designed to utilize the bone distal to the knee in a reconstruction that converts a hip disarticulation effectively to a through knee or long above knee amputation (1,2). However, patient expectations have increased in the last 2 decades and the functional deficit and the psychosocial impact of amputation are now far less acceptable, particularly, when an alternative surgical solution includes limb sparing surgery.
Advances in diagnostic imaging have improved dramatically and now facilitate the planning of critical surgical margins that underpin limb sparing surgery. Advances in chemotherapy and radiotherapy have also contributed to the success of limb sparing surgery by increasing survivorship and improving local control of disease. Greater sophistication in prosthetic design that incorporates modularization of component parts permits bespoke assembly of total femoral prostheses to fit almost all adult patients. The alternatives for total femoral prosthetic replacement other than amputation include massive osteoarticular allograft transplantation, allograft prosthetic composites, and custom stem prosthesis. These options are dominated by complications that are associated with biologic reconstructions including fracture, nonunion, infection, prolonged restricted weight bearing, and instability, thus making total femoral prosthetic replacement a very attractive option when considering total femoral resection.
INDICATIONS
Total femoral replacement is indicated after resections of diaphyseal tumors with long proximal and distal intramedullary extension of disease, after resection of proximal or distal tumor with extension to within 130 mm of the opposite epiphysis, and with extensive bone loss from widespread metastasis in patients with stable disease.
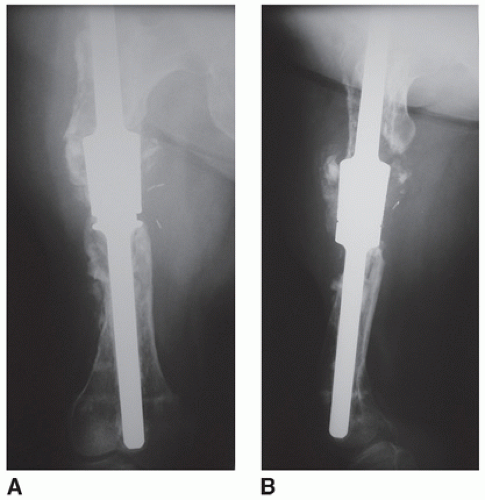
Total femoral resection and replacement may also be indicated in patients with widespread intramedullary or compartmental contamination of primary tumor. For example, a classic situation is seen with the patient who presents with a presumed solitary metastasis who undergoes prophylactic fixation with an intramedullary rod. The preparation of the femur for rod fixation results in the contamination of the marrow cavity and also the soft tissue around the entry portal for the rod (Fig. 11.1).
Occasionally, this procedure may be further compounded by a pathologic fracture, which results in a contained hematoma that requires wide soft tissue resection as well.
Some very large soft tissue sarcomas that encircle an extensive length of femur may also be treated by total femoral resection.
Total femoral resection may also be indicated in patients who have previously been treated with a proximal or distal femoral tumor endoprosthesis who now have the complication of aseptic loosening, periprosthetic fracture, or severe bone lysis.
Total femoral replacement may be indicated where previous diaphyseal reconstruction has failed (Fig. 11.2A,B).
The versatility of tumor endoprostheses for nononcologic causes is also well known.
Total femoral replacement may be indicated for patients who have undergone multiple complex revisions and are now left with minimal bone stock in the setting of gross osteolysis, aseptic loosening, or periprosthetic fracture.
Total femoral replacement may also be indicated in complex comminuted fractures, although this may be more appropriate in the setting of chronic and difficult nonunions of fractures.
Bone softening diseases such as Paget disease and fibrous dysplasia may result in such deformity and stress fractures that total femoral replacement may be the only option for management.
Some have suggested that chronic osteomyelitis may be an indication for resection and reconstruction. This should be considered with great caution in light of the very high risk of reinfection that may necessitate subsequent amputation.
CONTRAINDICATIONS
Total femoral resection is contraindicated for primary malignancies when either contamination or extraosseous tumor growth is so extensive as to make oncologically sound margins difficult to achieve.
This procedure is also contraindicated in patients who have widespread metastatic disease from sarcoma.
A total femoral prosthesis relies on stability at the hip and knee joint for proper functioning. The inherent instability of the prosthesis at the knee may be significantly exacerbated by femoral nerve palsy. Therefore, involvement of this nerve may preclude total femoral reconstruction.
Tumor resection that includes total quadriceps excision causes weakness in extension in much the same way as femoral nerve palsy. Inability to hold the knee in extension can lead to a loss of support in extension and collapse of the affected limb when trying to bear weight. An alternative solution would be the use of custom devices that arthrodesed the knee while permitting hip arthroplasty (3).
Femoral vessel compromise by tumor is a relative contraindication because these structures may be resected with the tumor and reconstructed by end-end anastamosis or bypass operations. However, major arterial and venous reconstructions are also associated with significant morbidity and limb loss from obstructive complications must be recognized as a potential risk of the operation.
Prosthetic reconstruction is contraindicated in the setting of systemic or regional sepsis. Delay in surgery is advocated until sepsis is overcome. If persistent limb sepsis prevents safe resection and reconstruction then amputation should be considered to minimize interruptions to systemic chemotherapy.
PREOPERATIVE PREPARATIONS
Total femoral resection is a complex procedure with many associated risks. The purpose of preoperative assessment is to exclude a contraindication to surgery, to define the surgical anatomy, and to plan the surgical margins in oncologic cases. In the setting of previous surgery or radiotherapy, significant fibrosis, thickening, and tethering of neurovascular structures may occur and should be anticipated. Vulnerable areas such as the popliteal fossa and around the femoral neck should be carefully imaged and closely inspected.
Plain Radiographs
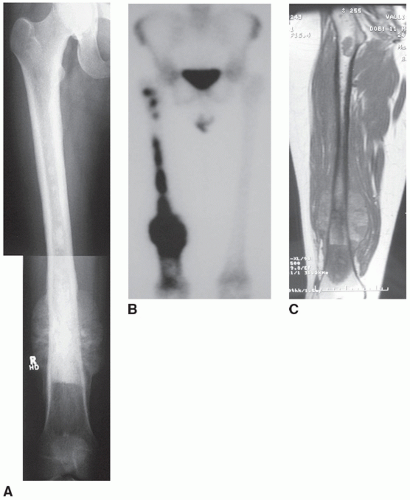
Plain radiography is important for preselecting a range of hip and knee sizes for this procedure (Fig. 11.3A). Templating using 1:1 radiographs allows a close estimation as to the appropriate sizes of prosthesis to have
available during the procedure. It is important to ascertain if extremes of sizes (very small or very large) are required. With the move toward digital imaging, true size images may be difficult to obtain in certain settings. Plain radiographs may also give an indication of intraosseous spread of tumor (Fig. 11.3B).
available during the procedure. It is important to ascertain if extremes of sizes (very small or very large) are required. With the move toward digital imaging, true size images may be difficult to obtain in certain settings. Plain radiographs may also give an indication of intraosseous spread of tumor (Fig. 11.3B).
Nuclear Medicine Imaging
Technetium methylene diphosphonate is an excellent screening test for identifying skip lesions in adjacent bones such as the pelvis and tibia (Fig. 11.3C). While some skip lesions may be able to be included in the resection, for example, proximal tibial skip lesions, other skip lesions such as in the pelvis may preclude total femoral resection and reconstruction. Newer investigational equipment now combine nuclear with computed tomographic scanning. This permits co-registration of functional and anatomic imaging for greater specificity of diagnosis and more accurate targeting for image guided biopsy. Tests for the presence of acute and chronic infections is critical for avoiding postoperative perioprosthetic infections.
Functional Nuclear Imaging
Thallium and PET scanning are two modalities that assess the metabolic activity of tumor tissue. When obtained at the time of diagnosis, the results form a good baseline measure against which to assess the response to neoadjuvant therapy. This is important because a poor response to chemotherapy for bone sarcomas requires far wider margins than those with an excellent response.
Computed Tomography
This technique is excellent for assessing the degree of cortical bone loss in metastatic carcinoma. If the extent of destruction is considered to be significant, a decision may be made to undertake total femoral resection and prosthetic reconstruction. Computed tomography is excellent also for assessing trabecular destruction, which can be subtle. Marrow extension or infiltration can be detected by the change in the marrow signal. Fat in the marrow provides an excellent contrast against which to highlight marrow deposits. Pulmonary scans should always be obtained as pulmonary metastases may preclude a major resection and reconstruction procedure.
Magnetic Resonance Imaging
This modality allows unsurpassed soft tissue contrast, which is capable of highlighting the subtle changes that may accompany any extraosseous extension, which is critical for planning surgical margins (Fig. 11.3D). This is also an excellent modality for scrutinizing any potential skip lesions. The excellent contrast between fat and tumor tissue together with contrast enhancement should allow delineation of any suspicious lesions. Careful attention should be paid to the pelvis and periacetabulum.
Angiography
Information on the course of the superficial femoral artery and vein and their significant branches through the thigh is critical when planning a total femoral resection and reconstruction. The vessels pass close to the femur at a number of locations such as the femoral neck, in the adductor canal, and through the hiatus in the distal part of adductor magnus. The profunda femoris vessels also tether the trunk proximally. Expansion of a soft tissue component may cause compression at any of these points leading to vascular obstruction and thrombosis. Advice on the quality of patent vessels should be sought and the potential for bypass surgery identified early.
Bladder Function
In the majority of cases, bladder catheterization is performed to allow urinary measurements and bladder care during and after surgery. Patients who have received thigh radiotherapy, particularly to the adductor compartment or proximal femur, may develop urethral stenosis at the bladder neck. This may result in difficult and traumatic catheterization. In some cases, endoscope-assisted catheterization may be required to safely pass a urinary catheter prior to surgery. Patients who are developing an acute stricture will describe impairment of urinary flow and if suspected, urodynamic studies done prior to surgery are advisable. Resolution of urethral stenosis prior to definitive limb surgery will minimize bacteremia of traumatic catheterization and reduce the risk of hematogenous infection.
PREPARATION
Position and Draping
Access to the hip and the knee is required for total femoral resection (Fig. 11.4). Unlike proximal femoral resection, which can be performed in the lateral position, additional knee resection and reconstruction requires
the patient in the supine position to allow access to both sides of the knee to achieve adequate dissection of the popliteal neurovascular structures and also to facilitate preparation of the tibia to receive the tibial component.
the patient in the supine position to allow access to both sides of the knee to achieve adequate dissection of the popliteal neurovascular structures and also to facilitate preparation of the tibia to receive the tibial component.
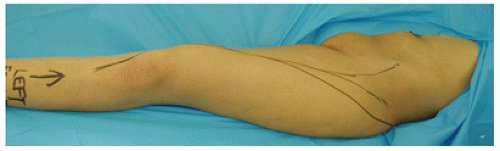 FIGURE 11.4 Preparation of entire limb for surgery with exposure from above iliac crest. Patient is in the supine position with a sandbag underneath the buttock. |
The patient is prepared in the supine position with no lateral support. A foot rest is used to keep the knee flexed at about 90 degrees and a sandbag is placed under the ipsilateral buttock to lift the buttock and trochanter off the operating table. The patient is draped with the lower limb completely free from the iliac crest down.
Anesthetic Considerations
Total femoral resection and reconstruction is likely to be a long procedure. All precautions are taken to ensure that all pressure points are well padded prior to the commencement of surgery. Sequential calf/foot compression devices should be employed to enhance venous flow in the nonoperated limb. Preoperative antibiotics should be used to minimize the risk of infection. Vancomycin and a third-generation cephalosporin should provide adequate cover against Gram-positive cocci, Gram-negative organisms, and anaerobes.
Venous access should include central lines, and arterial access is very useful to maintain continuous blood pressure monitoring.
Although most centers would induce general anesthesia, some centers may elect to provide regional anesthesia alone or in combination with general anesthesia. The value of including regional anesthesia is the opportunity to continue limb analgesia postoperatively with the use of an epidural catheter. The disadvantage of regional anesthesia is the potential for disguising a nerve plasy or compartment syndrome.
Anatomic Considerations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree