Medial Collateral Ligament Reconstruction
Christopher D. Harner
Anthony M. Buoncristiani
Fotios P. Tjoumakaris
INDICATIONS/CONTRAINDICATIONS
Of the four major ligaments in the knee, the medial collateral ligament (MCL) has the greatest chance to heal after injury. This is in large part due to its anatomic and biologic properties. Because the MCL heals, there are few cases in which surgical intervention is required. In fact, it has been shown that surgery may even be detrimental in certain situations, since the risk of postoperative stiffness is significant.
Clinical classification of MCL injuries can be organized by timing, severity, and associated injuries. All these factors must be taken into account when formulating a treatment plan. Timing, although somewhat artificial, can be divided into acute (< 3 weeks), subacute, and chronic (>4 to 6 weeks). This is based on the natural progression of the healing process, with the majority of MCL injuries healing to some extent within 3 to 4 weeks. Severity of the MCL injury is assessed by valgus stress testing at 0 and 30 degrees of knee flexion on physical examination. It is classified as per the guidelines established by the American Medical Association and discussed further later.
Finally, it is important to determine what other injuries are associated with an MCL tear. There are essentially three main scenarios: (a) no associated injuries (i.e., isolated); (b) associated with either anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL) disruption alone; and (c) multiliagementous injury. The anatomic location of the injury (i.e., femoral insertion, tibial insertion, or midsubstance tear) may be helpful in predicting the potential for healing. Femoral avulsions seem to heal better than tibial avulsions, although the risk of loss of motion is greater. The overall alignment of the limb also is an important factor, as an underlying genu varum alignment will protect the ligament more than genu valgum. Of course, patient activity level and expectations may also play a role in treatment.
Acute Cases
Isolated MCL Injuries
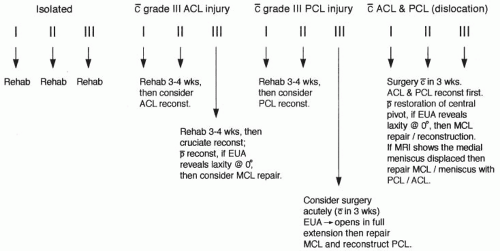
Isolated grade I and II MCL injuries are treated nonoperatively (Fig. 22-1). A guided program of early, protected (i.e., braced) motion, weight-bearing, and controlled exercises is instituted. The ACL acts as a secondary restraint to resist valgus load, and it is important to confirm its integrity before embarking on a course of nonoperative treatment.
Grade III, or “complete,” tears may also be treated nonoperatively, but only after careful exclusion of any associated injuries that may necessitate surgical intervention. These would include cruciate ligament injury, meniscal tear requiring repair, and entrapment of the MCL (Figs. 22-2 and 22-3).
With ACL Disruption
The indications for ACL reconstruction remain the same despite the presence of an MCL injury. In cases of grade I or II MCL tears, if the ACL is to be reconstructed, it is delayed 4 to 6 weeks, giving the MCL a chance to heal and allowing the knee to recover from the initial
trauma. Grade III MCL tears with ACL disruption pose more of a controversial scenario. There have been studies supporting acute surgery on both the MCL and the ACL as well as those supporting delayed reconstruction of the ACL along with nonoperative management of the MCL injury.
trauma. Grade III MCL tears with ACL disruption pose more of a controversial scenario. There have been studies supporting acute surgery on both the MCL and the ACL as well as those supporting delayed reconstruction of the ACL along with nonoperative management of the MCL injury.
It has been our experience that most grade III MCL injuries heal if protected. The major risk with early surgery is the development of arthrofibrosis. However, in a certain subset of patients with this
combination of injury (grade III MCL/ACL), the MCL does not heal and there is residual valgus and rotatory laxity that is very difficult to correct later. We try to detect this group initially by physical examination and magnetic resonance imaging (MRI). If the patient has gross opening in full extension, he or she is considered a candidate for MCL repair. The MRI can be helpful in this setting, as it will reveal if the injury is an avulsion off of the tibia or the femur. We believe that the tibial avulsion is more problematic, as the synovial fluid has access to the ligament/bone interface, which may prevent healing. In this scenario, we do a surgical repair of the MCL through a limited approach to the tibial insertion combined with an ACL reconstruction. We prefer allograft tissue for the ACL to minimize iatrogenic trauma. Furthermore, if significant laxity is noted with an anterior drawer (>10 mm), we elect to repair the posterior oblique ligament (POL) at the site of injury to decrease anteromedial rotatory instability that may complicate the ACL reconstruction in this scenario. We also repair meniscal pathology at the same time. When we do elect to repair an MCL/ACL injury, we delay the surgery at least 10 to 14 days and brace the knee in the interim. This allows for the acute effects of the trauma to subside.
combination of injury (grade III MCL/ACL), the MCL does not heal and there is residual valgus and rotatory laxity that is very difficult to correct later. We try to detect this group initially by physical examination and magnetic resonance imaging (MRI). If the patient has gross opening in full extension, he or she is considered a candidate for MCL repair. The MRI can be helpful in this setting, as it will reveal if the injury is an avulsion off of the tibia or the femur. We believe that the tibial avulsion is more problematic, as the synovial fluid has access to the ligament/bone interface, which may prevent healing. In this scenario, we do a surgical repair of the MCL through a limited approach to the tibial insertion combined with an ACL reconstruction. We prefer allograft tissue for the ACL to minimize iatrogenic trauma. Furthermore, if significant laxity is noted with an anterior drawer (>10 mm), we elect to repair the posterior oblique ligament (POL) at the site of injury to decrease anteromedial rotatory instability that may complicate the ACL reconstruction in this scenario. We also repair meniscal pathology at the same time. When we do elect to repair an MCL/ACL injury, we delay the surgery at least 10 to 14 days and brace the knee in the interim. This allows for the acute effects of the trauma to subside.
With PCL Disruption
Although a rare injury, this pattern can result in a very unstable knee. Because both the PCL and the MCL attach to the medial femoral condyle, complete disruption of both results in gross laxity of the medial side of the knee. In the setting of grade III injury to both of these structures, we recommend surgical treatment.
With ACL and PCL Disruption
In the setting of an ACL/PCL/MCL injury, we almost always repair or reconstruct all three injured ligaments. Delaying the intervention more than 3 weeks in this case often results in significant residual MCL laxity that is very difficult to correct. The only exception is if the MCL injury is only partial (i.e., grades I or II), in which case we postpone the surgery until final healing of the MCL occurs.
Chronic Cases
Chronic instability results following a grade III MCL injury that does not heal. There is usually more than single-plane (i.e., valgus) instability present with rotational and translational (i.e., cruciate ligaments) components. The overall alignment of the limb plays a critical part in the treatment. Knees with underlying genu valgum are more likely to have residual instability. In this setting both soft-tissue reconstruction and bony alignment may have to be addressed. The usual indication for reconstruction in chronic cases is persistent instability that affects activities of daily living.
PREOPERATIVE PLANNING
History
The MCL can be injured with valgus contact to the knee or through a twisting, noncontact mechanism. In the acute setting, depending on the severity and associated injuries, the patient will present with varying degrees of swelling, pain, and loss of motion. In combined ligament injuries, the patient is very uncomfortable and has significant loss of motion. The patient often presents with a large effusion and more pain than would be expected with an isolated ACL tear. If a combined ligament injury is suspected, the neurovasculature must be assessed, as a knee dislocation may have occurred. In the chronic setting, patients will present with instability, which usually affects activities of daily living and results in an inability to participate in athletic activities.
Examination
The goal of the examiner is to determine the degree of injury to the MCL as well as the presence of any associated injuries. In this regard, the examination of the MCL must be done in the setting of a comprehensive knee examination that includes assessment of the neurovascular status of the extremity. In the acute setting, the patient will have obvious discomfort, making the examination limited. The key to an informative examination is getting the patient to relax as much as possible. A pillow under the affected knee and gentle examination go a long way toward not only allowing the patient to guard less but also gaining his or her confidence.
The knee may or may not be grossly swollen, and the absence of a large effusion should not lead the examiner to a false sense of security. Tenderness to palpation over the MCL should be elicited.
Midsubstance tears may be associated with joint-line tenderness, creating potential difficulty in distinguishing meniscal from collateral injury. Concomitant injury to both structures, however, is possible.
Midsubstance tears may be associated with joint-line tenderness, creating potential difficulty in distinguishing meniscal from collateral injury. Concomitant injury to both structures, however, is possible.
Valgus stress testing of the affected knee in comparison to the contralateral knee is the cornerstone of the diagnosis. This is done at both 30 degrees of flexion and full extension, if possible. Flexing the knee to 30 degrees isolates the MCL. Putting the leg over the side of the examining table helps stabilize the femur, and placing a finger on the medial joint line helps in assessing the amount of opening. The amount of medial compartment opening is graded according to the American Medical Association (AMA) guidelines. A grade I injury allows 0 to 5 mm of opening with a firm end point; a grade II injury allows 5 to 10 mm with a firm end point; a grade III injury, or a “complete” tear of the superficial and the deep portions of the ligament, allows greater than 10 mm of opening and the end point is usually soft. These numbers are all with reference to the uninvolved side. The following figures demonstrate sequentially the Lachman (Fig. 22-4), posterior drawer (Fig. 22-5), positioning the knee at 30 degrees (Fig. 22-6) and then applying a valgus load (Fig. 22-7); then positioning the knee at 0 degrees (Fig. 22-8) and applying a valgus load (Fig. 22-9).
Any opening of the medial joint line to valgus stress with the knee at 0 degrees is a much more ominous sign and is seen only with grade III injuries. It implies a large magnitude of force to the knee and mandates careful scrutiny of cruciate ligaments, the menisci, and the patella for stability. The posteromedial capsule and the vastus medialis obliquus must also be suspected of involvement.
Another provocative test to determine the degree of injury is the external rotation anterior drawer test. This maneuver assesses the amount of anterior translation of the tibia under the femur at roughly 80 degrees of knee flexion and the foot in maximal external rotation. It is not always possible to perform this test on the acutely injured knee due to patient discomfort. It is positive if the amount of translation is significantly increased compared with the contralateral knee. The sine qua non for this test to be positive is disruption of the meniscotibial ligaments, allowing the meniscus to move freely. If the meniscotibial ligaments are intact, the meniscus remains firmly seated on the tibia, providing a buttress against the posterior femoral condyle and thus resisting anterior translation of the tibia.
Imaging
A standard radiographic knee series is indicated in all cases of suspected MCL injury. This should include a 45-degree flexion weight-bearing view and lateral and sunrise views. If weight bearing is not possible, a simple anteroposterior view should be substituted. Avulsions or osteochondral fragments seen on radiograph could significantly affect the treatment plan. Any patient with increased laxity to valgus stress and open physes should have stress views to localize the source of the laxity. In chronic cases with instability, long-standing cassette radiographs of both lower extremities should be obtained to assess alignment.
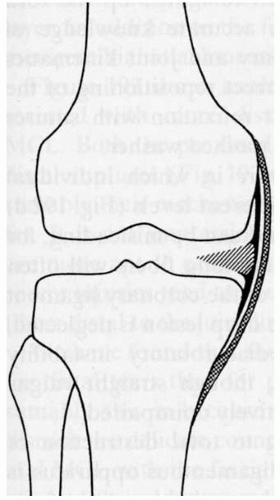
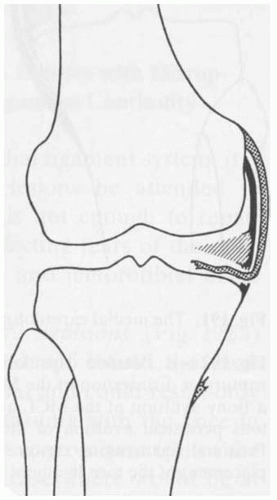
Magnetic resonance imaging offers an abundance of information that may alter the treatment plan. The presence of meniscal tears, the location of the MCL tear, and any concomitant injuries, ligamentous or otherwise, can be discovered. This study is particularly useful when the physical examination is compromised but can also reveal pivotal information, such as the presence of an entrapped MCL lesion (Figs. 22-10 and 22-11), even in apparently straightforward cases.
 FIGURE 22-9 A valgus stress is placed on the knee at full extension. The amount of medial joint space is assessed. |
 FIGURE 22-10
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|