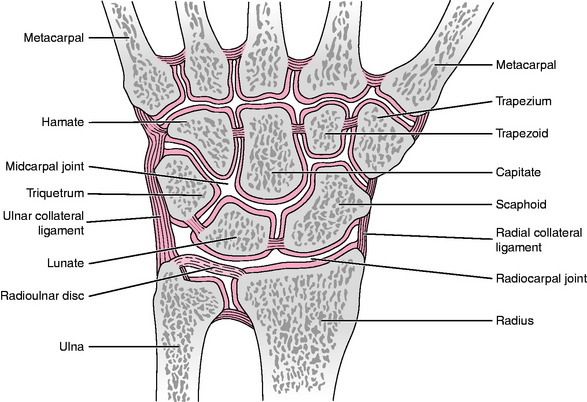
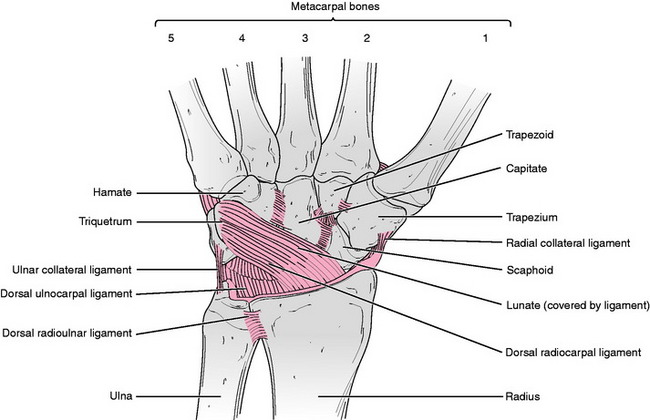
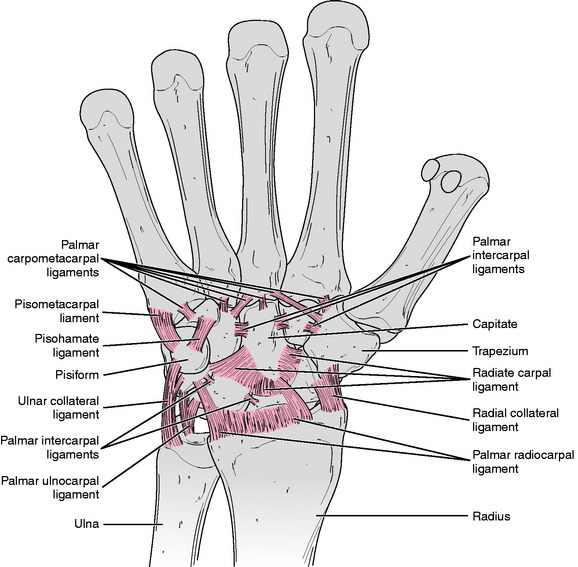
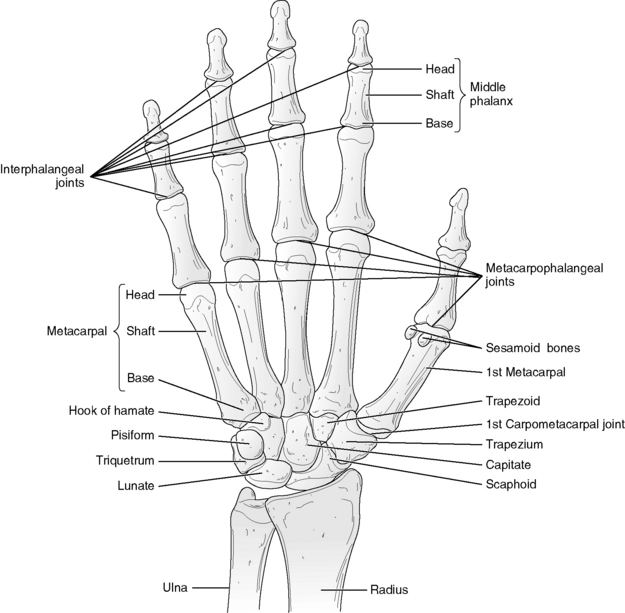
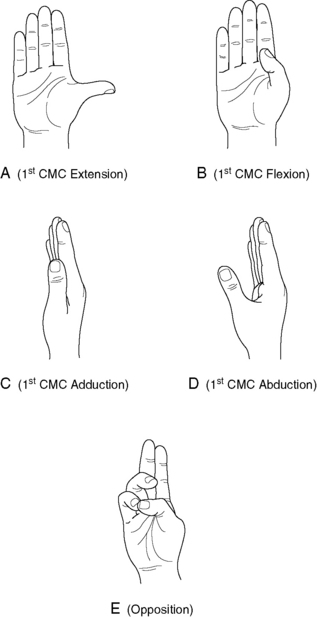
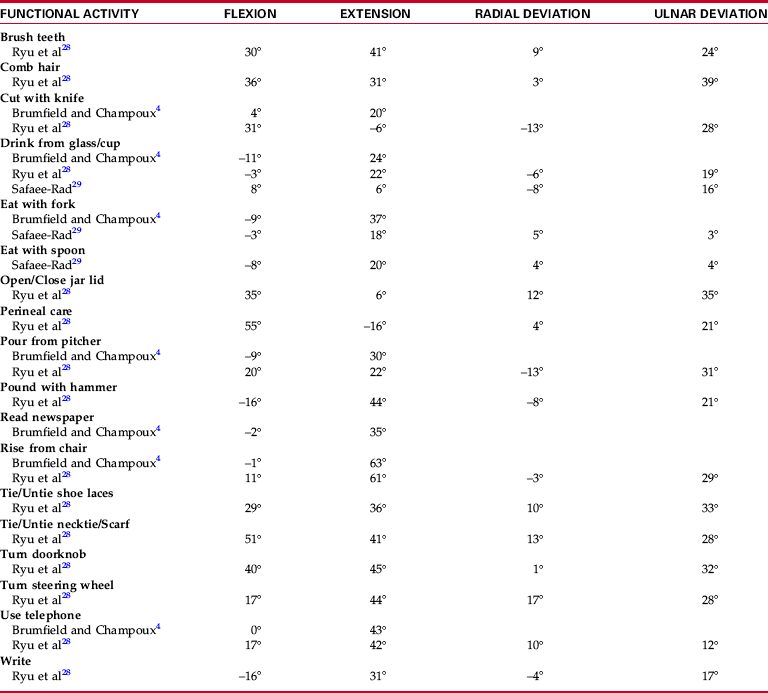
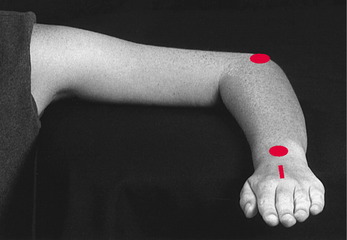
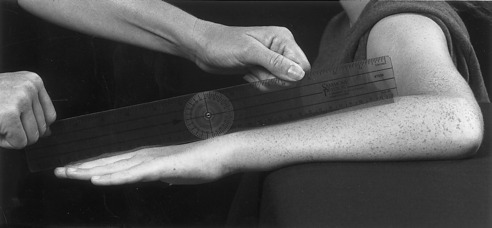
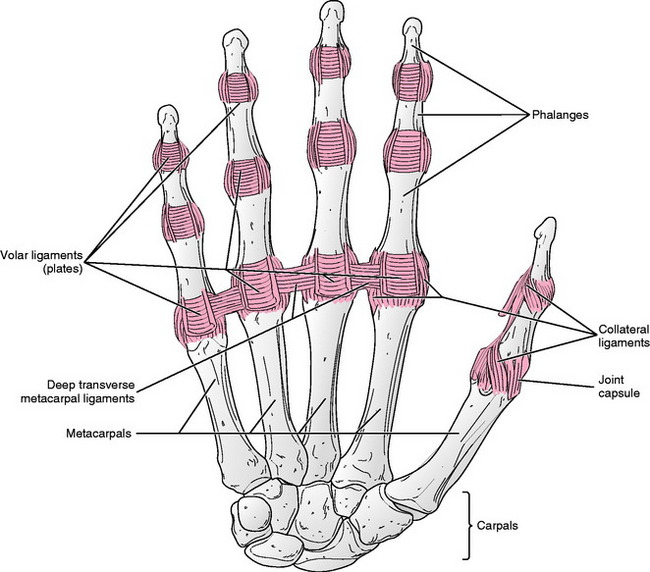
Chapter 5 Although Gray’s Anatomy designates the radiocarpal joint as “the wrist joint proper,”5 other authors describe a wrist joint complex that includes the more distal midcarpal joint and the radiocarpal joint.18,25 The proximal articular surface of the radiocarpal joint is concave and is composed of the distal end of the radius and the triangular fibrocartilage of the radioulnar disk (Fig. 5-1). Distally, three of the carpal bones in the proximal row, specifically, the scaphoid, lunate, and triquetrum, form the convex-shaped distal articular surface of the radiocarpal joint. The articulation between the proximal and distal rows of carpal bones makes up the midcarpal joint (see Fig. 5-1). Some sources have described the midcarpal joint as having medial and lateral joint compartments.25,36 The medial compartment consists of the articulation of a concave proximal surface formed by the scaphoid, lunate, and triquetrum and a convex distal surface formed by the hamate and head of the capitate. Joint surfaces of the lateral compartment are fairly planar and consist of the articulation of the trapezium and trapezoid proximally with the scaphoid bone in the distal carpal row. Several ligaments reinforce the wrist joint complex and guide the motions that occur at the radiocarpal and midcarpal joints. A number of intrinsic ligaments interconnect the carpal bones, binding them together and providing stability to the wrist.2 Limitation of wrist motion occurs primarily via ligaments that arise external to the carpal bones. These so-called extrinsic ligaments of the wrist include the posteriorly located dorsal radiocarpal ligaments (Fig. 5-2), the anteriorly positioned palmar ulnocarpal and palmar radiocarpal ligaments (Fig. 5-3), and the radial and ulnar collateral ligaments, located on the radial and ulnar aspects of the wrist, respectively (see Figs. 5-2 and 5-3).2,21,22,35 Movement at both the radiocarpal and midcarpal joints is necessary to achieve the full range of motion (ROM) of the wrist, which has been classified as a condyloid joint with 2 degrees of freedom.3 Motions present at the wrist include flexion, extension, abduction (radial deviation), and adduction (ulnar deviation). These movements occur around an axis that passes through the head of the capitate.37 The amounts of flexion and ulnar deviation exceed the amounts of extension and radial deviation available at the wrist.9,28,30 Motions of the bony surfaces making up the radiocarpal and midcarpal joints during motions of the wrist are fairly complex. Models have been proposed that, although not complete, account for much of the motion that occurs.14,27,30 During flexion of the wrist, convex distal joint surfaces at the radiocarpal and midcarpal joints roll in a volar direction and slide dorsally on concave proximal joint surfaces. During extension, motion of the bony surfaces of these joints occurs in the opposite direction. Ulnar deviation is produced by ulnar roll and simultaneous radial slide of the convex distal joint surfaces of the radiocarpal and midcarpal joints on the concave proximal surfaces of these joints. Movement of the joint surfaces occurs in the opposite direction during radial deviation, with most of this motion being produced by the midcarpal joint.25 With the fingers free to move, limitation of wrist flexion and extension ROM is produced by passive tension in the dorsal and palmar radiocarpal ligaments, respectively.31 In addition, the palmar ulnocarpal ligament restricts wrist extension. Limitation of ulnar deviation occurs as the result of tension in the radial collateral ligament. Radial deviation of the wrist is terminated by bony impingement of the trapezium upon the radial styloid process.5,13,25,34 Information regarding normal ranges of motion for all movements of the wrist is found in Appendix B. The end-feel for passive flexion and extension of the wrist is firm because of ligamentous limitations of motion when the fingers are mobile. However, if the fingers are not free to move and are flexed, their position will limit wrist flexion secondary to passive tension in the extrinsic finger extensors. Conversely, extension of the fingers will limit wrist extension owing to passive tension in the extrinsic finger flexors. Wrist adduction is also limited by ligamentous structures and thus possesses a firm end-feel. Wrist abduction is limited by bony contact between the radial styloid process and the trapezium, producing a bony end-feel at the limit of motion.5,13,34 Unlike the carpometacarpal (CMC) joints of the fingers, the CMC joint of the thumb (first CMC joint) has a high degree of mobility. This joint is classified as a saddle joint and is formed by the articulation between the trapezium and the base of the first metacarpal bone (Fig. 5-4). The saddle classification of the joint defines the structure of the joint surfaces, each of which is concave in one direction and convex in the other.38 According to Neumann,25 ligamentous reinforcement of the first CMC joint occurs via five ligaments: the anterior and posterior oblique, located respectively on the anterior and posterior aspects of the joint; the ulnar and radial collateral, located respectively on the ulnar and radial sides of the joint; and the first intermetacarpal ligament, which connects the bases of the first and second metacarpal bones. Motions occurring at the first CMC joint include flexion, extension, abduction, adduction, rotation, and opposition (Fig. 5-5, A through E). From the anatomical position, CMC flexion and extension occur in a plane parallel to the palm of the hand (frontal plane) (see Fig. 5-5, A and B), whereas abduction and adduction occur in a plane positioned perpendicular to the palm (sagittal plane) (see Fig. 5-5, C and D).5,25 Rotation occurs as a result of rotation of the metacarpal around its longitudinal axis during flexion and extension of the first CMC joint and normally is not measured clinically. Opposition is a combination of flexion, medial rotation, and abduction of the first CMC joint (see Fig. 5-5, E).5,25 During flexion and extension at the first CMC joint, the concave arch of the first metacarpal moves on the convex arch of the trapezium. Thus, according to the rules governing concave on convex movement, the first metacarpal rolls and slides in an ulnar direction during flexion and in a radial direction during extension at the first CMC joint. Conversely, because abduction and adduction at the first CMC joint involve movement of the convex arch of the first metacarpal on the concave arch of the trapezium, the first metacarpal rolls volarly and slides dorsally during abduction and moves in the reverse direction during adduction.11,25 Motions of the first CMC joint are limited by a variety of structures, including soft tissues, ligaments, muscles, and joint capsule. CMC joint flexion may be limited by contact between the thenar muscle mass and the soft tissue of the palm. When the muscle mass of the thenar eminence is not well developed, limitation of CMC joint flexion is caused by tension in the extensor pollicis brevis and abductor pollicis brevis muscles, as well as by tension in the radial collateral ligament and the dorsal aspect of the CMC joint capsule. Extension of the first CMC joint is limited primarily by tension in the muscles (adductor pollicis, flexor pollicis brevis, first dorsal interosseous, opponens pollicis) and by tension in the anterior oblique ligament. The limits of CMC abduction occur as the result of tension in the adductor pollicis and first dorsal interosseous muscles and all ligaments surrounding the first CMC joint, and because of stretch of the skin and connective tissue of the web space. Both opposition and adduction of the first CMC joint are limited by soft tissue approximation, the former between the pad of the thumb and the base of the fifth digit, and the latter between the side of the thumb and the tissue overlying the second metacarpal.13,25,38 Information regarding normal range of motion for all movements of the first CMC joint is found in Appendix B. The metacarpophalangeal (MCP) joints of digits 1 through 5 are classified as condyloid joints and are formed by the articulation of the convex head of the metacarpal with the concave base of the proximal phalanx of the corresponding digit (see Fig. 5-4). Each MCP joint is reinforced along its sides by a pair of collateral ligaments and along its volar surface by a volar plate. The volar plates are fibrocartilaginous discs that reinforce the joint, resist hyperextension, and provide an expanded articular surface for the metacarpal heads.25 The volar plates of the second through fifth MCP joints are interconnected via the deep transverse metacarpal ligaments23 (Fig. 5-6). Fig. 5-6 Ligamentous reinforcement of the metacarpophalangeal and interphalangeal joints—palmar view. Nine interphalangeal (IP) joints are present in the digits of the hand. Each finger possesses two IP joints: a proximal interphalangeal joint (PIP), which consists of the articulation of the convex head of the proximal phalanx with the concave base of the middle phalanx, and a distal interphalangeal joint (DIP), which consists of the articulation of the convex head of the middle phalanx with the concave base of the distal phalanx (see Fig. 5-4). The thumb possesses only a single IP joint, formed by the articulation of the convex head of the proximal phalanx with the concave base of the distal phalanx. Similar to the MCP joints, each IP joint is reinforced by a pair of collateral ligaments attached along the sides of the joint and by a volar plate on the volar surface (see Fig. 5-6). The functions of these structures of the IP joints are analogous to their functions at the MCP joints.17,23,25 Motions available at the MCP joints of digits two through five consist of flexion, extension, abduction, and adduction; motion at the MCP joint of the thumb is essentially limited to the motions of flexion and extension.32 The amount of MCP flexion displays a general increase from the first to the fifth digits, and MCP extension is greatest in the second and fifth digits.19,33 The range of MCP joint abduction is most pronounced in the second and fifth digits, with less motion available in the third and fourth digits and little to no motion available in the first MCP joint (in the thumb). Owing to tightness of the collateral ligaments when the MCP joints are flexed, MCP abduction is least restricted when the MCP joints are extended and is severely limited to absent when the joints are flexed. Each of the IP joints of the hand is classified as a hinge joint and is thus able to perform the motions of flexion and extension.5,13 There appears to be no significant difference in the amount of flexion and extension available at the PIP and DIP joints as one progresses across the hand.19,33 During movements at the MCP and IP joints, the concave distal joint surface (base of the phalanx) rolls and slides on the convex proximal joint surface in the same direction as the external motion. For example, during MCP extension, the base of the proximal phalanx rolls and slides dorsally, and during flexion, the roll and slide occurs in a volar direction.25 Flexion of the MCP joints increases in range as one moves from the first digit (the thumb) toward the fifth digit, and it is restricted by a variety of structures, including tension in the collateral ligaments and posterior joint capsule and bony contact between the anterior aspects of the metacarpal head and the base of the proximal phalanx. Limitation of MCP joint extension is produced by tension in the anterior joint capsule and volar plate. MCP joint abduction is limited by tension in the collateral ligaments and the skin of the interdigital web spaces. Adduction at these joints is restricted primarily by soft tissue contact with the adjacent digit.13,18,25 Limitation of IP joint flexion depends on the joint being moved. Flexion at the PIP joint usually is limited by contact with the soft tissue covering the anterior aspects of the proximal and middle phalanges of digits 2 through 5. Flexion at the IP (thumb) and DIP (fingers) joints (and occasionally flexion at the PIP joints of the fingers) is limited by tension in the posterior joint capsule and collateral ligaments. Extension of all IP joints is limited by tension in the anterior joint capsule and volar plate of the joint being moved.13,18,25 Information regarding normal ranges of motion for all movements of the MCP and IP joints of the hand is found in Appendix B. The capsular pattern is the same for the MCP joints and the IP (PIP and DIP) joints. In each of these joints, the capsule should be suspected if flexion is more limited than extension.6,13 Several authors have investigated the motion that occurs at the wrist during functional activities in healthy adults. In 1984, Brumfield and Champoux4 used a uniaxial electrogoniometer to measure wrist flexion and extension in 19 healthy adults during seven hand placement motions and seven functional activities. Participants in the study consisted of 12 men and 7 women aged 25 to 60 years. On the basis of gathered data, the authors concluded that a range of 10 degrees of wrist flexion to 35 degrees of wrist extension was sufficient to perform the functional activities included in the study. A year later, Palmer and colleagues26 used a triaxial goniometer to measure wrist flexion, extension, radial deviation, ulnar deviation, and rotation during 52 different tasks. Tasks included in the study were categorized according to activity, including personal hygiene, culinary, other activities of daily living (ADLs), carpentry, housekeeping, secretarial, mechanical, and surgical. Ten healthy subjects of unstated age were used to gather data for the tasks involved in personal hygiene, culinary, and other ADLs, and subgroups of five subjects were used for the other categories. Although specific ROM data were not provided by the authors, summary data for each category indicated that the ROM used to complete personal hygiene, culinary, and other ADL tasks consisted of 33 degrees of wrist flexion to 59 degrees of wrist extension, and 23 degrees of radial deviation to 22 degrees of ulnar deviation. Other groups of investigators, including Safaee-Rad et al29 and Ryu et al,28 have examined wrist motion during functional activities. The functions studied by Safaee-Rad and colleagues were limited to feeding activities in a group of 10 healthy adult men aged 20 to 29 years, which were analyzed using a three-dimensional (3D) motion analysis system. Ryu and colleagues28 used a biaxial wrist electrogoniometer to measure motion in 40 subjects (20 men and 20 women of unstated age) during seven hand placement and 24 functional activities. Table 5-1 contains a summary of selected data from the studies by Brumfield and Champoux,4 Safaee-Rad et al,29 and Ryu et al.28 Data from the study by Ryu et al were translated from graphic data provided in the published report. Fewer studies have investigated motion of the joints of the hand during functional activities. Hume and colleagues10 used both standard and electrogoniometric methods to measure motion of the MCP and IP joints of the fingers and thumb during 11 functional activities in 35 adult males aged 26 to 28 years. On the basis of data collected in this study, the authors concluded that only a small percentage of the total ROM of the fingers was required for functional activities. They reported average flexion postures at each of the joints for all functional activities combined, as follows: MCP joint—61 degrees, PIP joint—60 degrees, DIP joint—39 degrees, MCP joint of thumb—21 degrees, and IP joint of thumb—18 degrees. Some of the data reported by Hume et al were supported in a later study by Lee and Rim,16 who investigated the finger (but not thumb) joint angles and forces used by four different individuals when grasping five cylinders of different sizes. In their results, Lee and Rim reported that flexion angles at the MCP joints and the PIP joints increased as the size of the cylinder being grasped decreased. However, regardless of cylinder size, the position of the DIP joint remained consistently at around 40 degrees of flexion (almost identical to the average 39 degrees of flexion reported for this joint by Hume et al10). Figures 5-7 through 5-9 illustrate motions of the wrist and hand used to perform selected functional activities. Recommended techniques for measuring flexion and extension of the wrist involve positioning the goniometer along the radial, ulnar, and dorsal/volar surfaces of the wrist.1,7,24 In a multicenter study of wrist flexion and extension goniometry, LaStayo and Wheeler15 compared the reliability of all three positioning techniques and found that the dorsal-volar technique was consistently more reliable than the other two (see Chapter 7 for a full description of this study). Therefore, in this text, the dorsal-volar positioning technique is presented as the technique of choice, with radial positioning used as an alternative technique for measuring wrist flexion and extension. Wrist abduction and adduction are measured using the standard technique of positioning the goniometer over the dorsal surface of the joint.7 When motion in one plane of movement at the wrist is measured, a neutral position of the wrist with reference to the other plane should be maintained. For example, when wrist flexion-extension is measured, the subject’s wrist should not be deviated in a radial or ulnar direction. Conversely, when radial and ulnar deviation is measured, a neutral wrist position in terms of flexion and extension should be maintained. In a study of 54 subjects, Marshal et al20 found that wrist position in one plane could significantly affect wrist ROM in the perpendicular plane. A variety of methods of measuring motion of the first CMC joint have been presented in the literature.1,7 Reported norms for ROM of this joint vary widely (see Appendix B), presumably because of differences in measurement techniques. Much of the variation in technique appears to be due, at least in part, to inconsistent terminology regarding motion of this joint. Most of the techniques used in this text are based on motions of the CMC joint as defined in Gray’s Anatomy.5 Measurement of first CMC joint opposition involves the measurement of motions occurring at the first and fifth CMC joints, as well as motion occurring in at least one other joint of the first or fifth digit. To avoid measuring motion in any joint other than the first CMC joint, the technique described in this text for measuring first CMC opposition is one that was modified from two different techniques recommended by the American Academy of Orthopaedic Surgeons (AAOS)7 and the American Medical Association (AMA).1 The AAOS technique examines opposition by measuring the linear distance from the tip of the thumb to the base of the fifth metacarpal, stating that “opposition is usually considered complete when the tip of the thumb touches the base of the fifth finger.”7 Although the base (palmar digital crease) of the fifth digit provides a reproducible landmark against which first CMC joint opposition can be measured, included in this motion is measurement of MCP and IP flexion of the thumb, which the AAOS considers part of opposition. The technique for examining opposition recommended by the AMA involves measuring the linear distance from the flexor crease of the thumb IP joint to the distal palmar crease over the third metacarpal, without allowing flexion at the MCP or IP joint of the thumb.1 Although the flexor crease of the thumb IP joint provides a more reproducible landmark than the tip of the thumb, the distal palmar crease runs obliquely across the third metacarpal, providing a variety of points along which the distal end of the ruler may be placed during measurement (Fig. 5-10). Such a variety of possible placements could lend inconsistency to the results obtained when opposition is measured according to the AMA technique. In an effort to use a technique that (1) measures only opposition occurring at the first CMC joint, and (2) uses reproducible landmarks for both proximal and distal ends of the ruler, a technique that combines the best of the AAOS7 and AMA1 techniques is described in this text. The technique described herein examines first CMC joint opposition by measuring the linear distance between the flexor crease of the IP joint of the first digit (thumb) and the palmar digital crease of the fifth digit. Motion of the MCP and IP joints of the first and fifth digits is prevented during measurement. Unfortunately, no standards for normal ROM are yet available for this technique of measuring opposition. During goniometric measurement of MCP and IP joint motion, one must remain mindful of the fact that position of the proximal joints can greatly affect the ROM of more distal joints of the hand.19 Tension in the extrinsic finger extensors, when more proximal joints such as the wrist are flexed, can restrict the amount of flexion available in distal joints, such as the MCP joints. Conversely, extension of the more proximal joints causes tension on the extrinsic finger flexors, which, in turn, restricts the amount of extension that can be obtained at more distal joints. Therefore, care should be taken to maintain the proximal joints of the wrist and hand in a neutral position during measurement of flexion and extension of the MCP and IP joints. The standard technique for measuring MCP and IP joint flexion is performed with the goniometer positioned over the dorsal surface of the joint being examined.1,7 Extension of the MCP and IP joints may be measured with the goniometer positioned over the dorsal or volar surface of the joint. However, the soft tissue over the volar surface of the MCP joints may interfere with alignment of the goniometer during measurement of MCP extension using the volar positioning technique. Lateral positioning of the goniometer is a technique that is preferred by some examiners, but it has been reported to be slightly less reliable than dorsal placement.8
MEASUREMENT of RANGE of MOTION of the WRIST and HAND
WRIST JOINT
OSTEOKINEMATICS
ARTHROKINEMATICS
LIMITATIONS OF MOTION
END-FEEL
FIRST CARPOMETACARPAL JOINT
OSTEOKINEMATICS
ARTHROKINEMATICS
LIMITATIONS OF MOTION
METACARPOPHALANGEAL AND INTERPHALANGEAL JOINTS
OSTEOKINEMATICS
ARTHROKINEMATICS
LIMITATIONS OF MOTION
CAPSULAR PATTERN
RANGE OF MOTION AND FUNCTIONAL ACTIVITY
TECHNIQUES OF MEASUREMENT
FIRST CARPOMETACARPAL JOINT
METACARPOPHALANGEAL AND INTERPHALANGEAL JOINTS