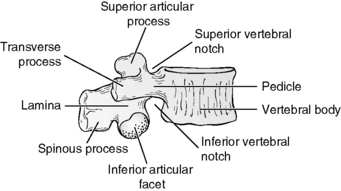
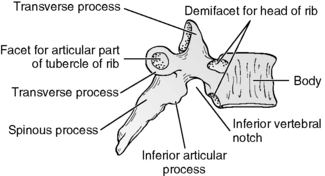
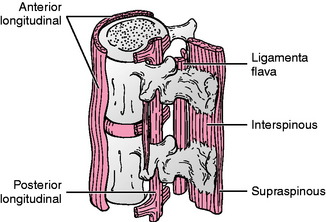
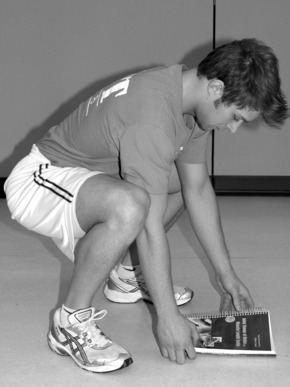
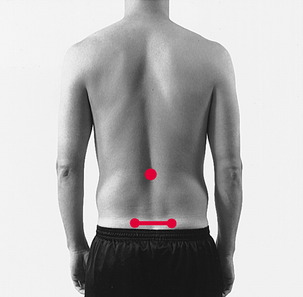
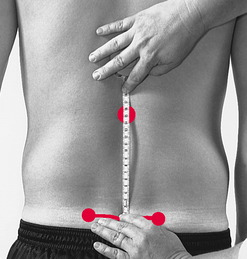
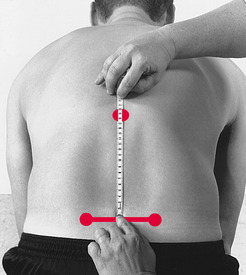
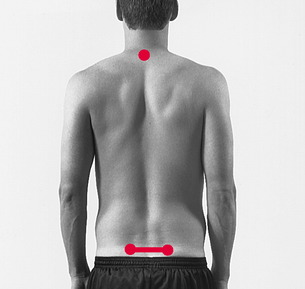
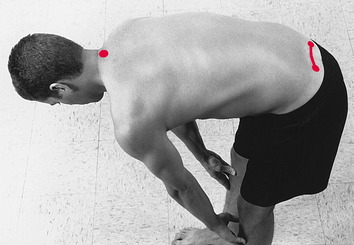
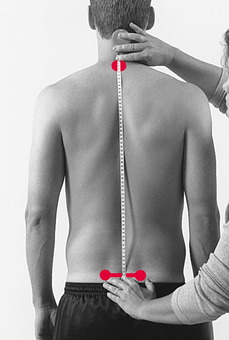
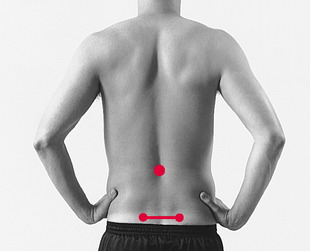
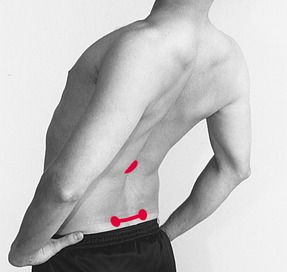
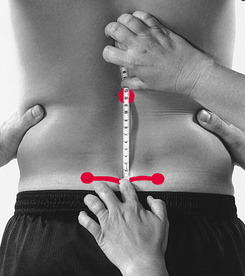
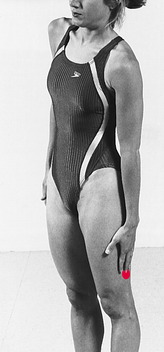
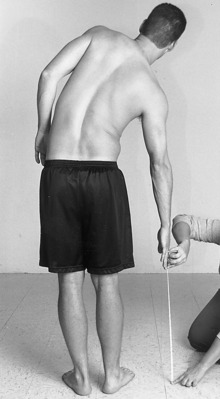
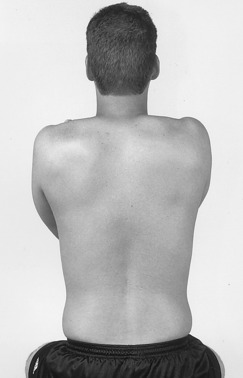
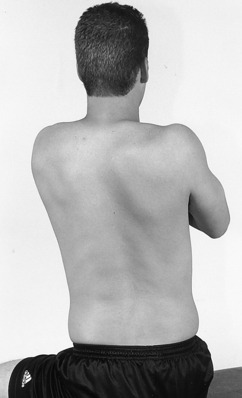
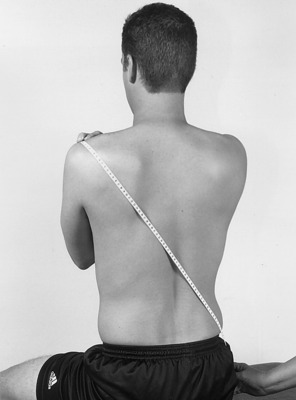
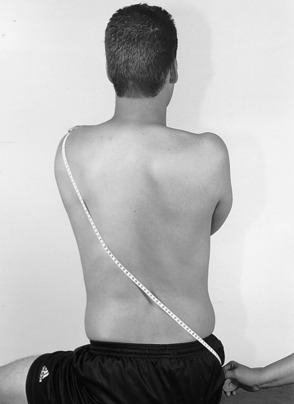
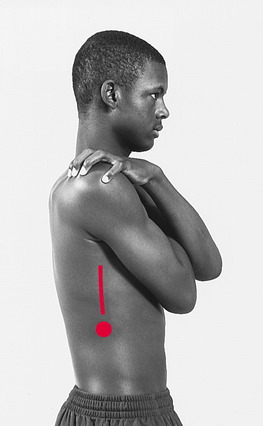
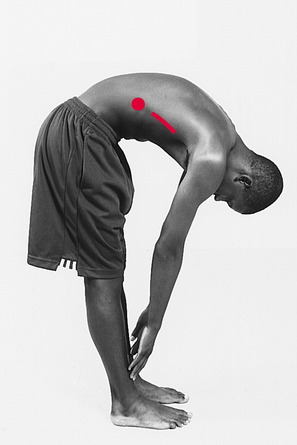
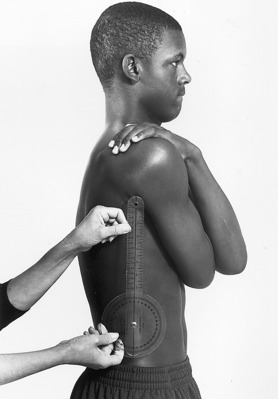
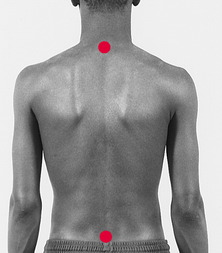
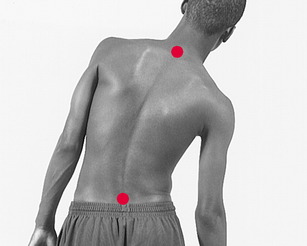
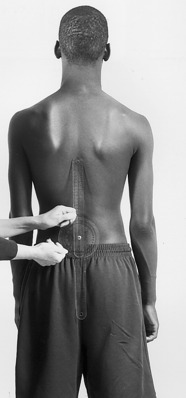
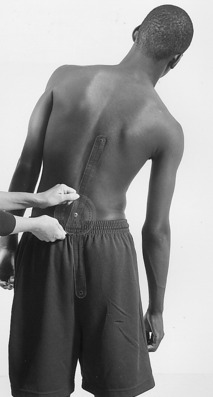
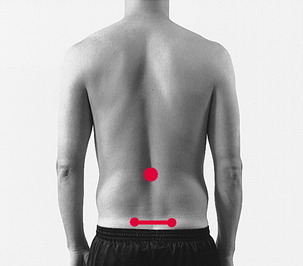
Chapter 8 The following discussion of the thoracic and lumbar spine is a synopsis of information presented in several contemporary sources.4,7,11 Although the cervical spine is built for maximum mobility, the thoracic spine and lumbar spine are built for weight bearing and stability. Twelve vertebrae (composed of the superior and inferior vertebral facets, the vertebral bodies, and the discs that are interposed between the vertebral bodies) make up the thoracic spine, and five make up the lumbar spine. A typical lumbar vertebra is pictured in Figure 8-1, and a typical thoracic vertebra is pictured in Figure 8-2. The major differences between the two are the long spinous process of the thoracic spine, which is directed downward rather than posterior, and the fact that the thoracic spine articulates with the ribs. A general overview of the connective tissue of the thoracic and lumbar spine includes the intervertebral disc, which connects the vertebral bodies to form intervertebral cartilaginous joints, and the following supporting ligaments: anterior longitudinal, posterior longitudinal, ligamentum flavum, intraspinous and supraspinous (Fig. 8-3). Six main ligaments, which provide stability and limit motion, are associated with the intervertebral joints. The anterior longitudinal ligament prevents excessive spinal extension, and the posterior longitudinal, ligamentum flavum, interspinous, and supraspinous ligaments limit flexion of the spine. In addition, the spinous processes of the thoracic spine limit extension. The intertransverse ligaments limit lateral flexion. Rotation of the spine is limited by facet orientation. Information on normal ROM for the thoracic and lumbar spine may be found in Appendix B. The amount of lumbar movement required for four functional activities was examined by Hsieh and Pringle5: stand-to-sit, sit-to-stand, picking up a small object from the floor, and putting on socks (Figs. 8-4 through 8-7). The authors examined 48 healthy subjects (mean age, 26.5 ± 4.6 years); instructions were provided to each subject to standardize how each activity was performed. The authors reported that sit-to-stand and stand-to-sit activities required 56% to 66% lumbar flexion. Putting on socks required 90% lumbar flexion. Picking up a small object from the floor required almost full lumbar flexion (95%). Therefore, putting on socks and picking up a small object from the floor required almost twice as much lumbar ROM as was required for sit/stand activities. The authors suggested that subjects with less than 79% flexion of the lumbar spine will show compensations during sit/stand activities and will be unable to pick up objects from the floor or put on their socks. The least expensive instrument for measuring spinal movement, and perhaps the easiest to use, is a tape measure. Additionally, a tape measure probably has been used in the clinic for measuring ROM of the spine longer than any other measurement technique.8 SCHOBER METHOD: One of the most common tape measure procedures used to measure lumbar flexion relates to a technique originated by Schober and subsequently modified for measurement of spinal flexion. According to Macrae and Wright,8 in 1937 Schober described the original two-mark method for measuring spinal flexion, in which one mark is made at the lumbosacral junction, and a second mark is made 10 cm above the first mark, while the subject stands with the spine in a neutral position. After the standing subject bends forward as far as possible, the increase in distance between the first and second marks provides an estimate of the amount of flexion that is present in the spine. Because the tape measure technique relies on stretching or distraction of the skin overlying the spine, this technique (and modifications of the technique) is sometimes referred to as the skin distraction method. Macrae and Wright8 modified the original Schober method by introducing a third mark, a measurement mark placed 5 cm below the lumbosacral junction. This modification uses a mark at the lumbosacral junction and other marks 5 cm inferior and 10 cm superior to the lumbosacral junction. The rationale offered by Macrae and Wright8 for making the modification of the original Schober technique is that when using the Schober technique in their pilot work, the authors observed that skin above and below the lumbosacral spine was distracted during flexion of the lumbar spine, leading to inaccuracies in measurement. Therefore, the technique that Macrae and Wright8 referred to as the “modified” Schober technique included three marks: (1) the lumbosacral junction, (2) 5 cm inferior to the lumbosacral junction, and (3) 10 cm superior to the lumbosacral junction. Van Adrichem and van der Korst13 suggested that using the lumbosacral junction (the base mark used for the Schober technique), which had to be identified by palpation, added difficulty to this method of measurement. Given this information, Williams et al14 suggested that the “modified-modified Schober,” rather than the Schober or the modified Schober method, should be used. The modified-modified Schober uses two skin landmarks (as opposed to three skin landmarks used with the modified Schober). These two landmarks include a point bisecting a line that connects the two posterior superior iliac spines (PSIS) (base line) and a mark 15 cm superior to the base line landmark. Given the ease of palpating the PSIS and the difficulty involved in determining the lumbosacral junction, the base line for measuring lumbar flexion and thoracolumbar flexion used in this chapter is the bisection of the line that connects the two PSIS, as described by Williams et al14 (see Figs. 8-9 to 8-16). Moll and Wright10 suggested that modifications of the Schober technique might be appropriate for the examination of lumbar extension. These authors suggested measuring the change in skin marks as the marks move closer together during the extension movement. Again, for reasons previously described, the base line for measuring lumbar extension used in this chapter is the bisection of the line connecting the two PSIS, as described by Williams et al14 (see Figs. 8-29 to 8-32). FINGERTIP-TO-FLOOR METHOD: In an attempt to examine flexion of the spine quickly and reproducibly, some authors have advocated the fingertip-to-floor method.3,6 The fingertip-to-floor method differs from the Schober method and its modifications in that these measurements are not taken directly over the lumbar spine. The patient simply bends forward, and the distance between the tip of the middle finger and the floor is measured with a tape measure (Fig. 8-8). Measuring lateral flexion by placing a mark at the location on the lateral thigh that the third fingertip can touch during erect standing and after lateral flexion (see Figs. 8-49 to 8-51) was first introduced by Mellin.9 The distance between the two marks represents the range of lateral flexion to that side. Fig. 8-51 Measurement of difference between skin marks on thigh (indicated by red dots) using tape measure. Using the fingertip-to-floor method, the distance from the third fingertip to the floor is measured, first with the patient standing erect, and then after the subject laterally flexes the spine.2 The change in distance from erect standing to lateral flexion is considered the range of lateral flexion (see Fig. 8-52). The standard goniometer, consisting of two hinged rulers rotating on a protractor (described in detail in Chapter 1), is commonly used for measuring ROM of the spine. Techniques for measurement of flexion (see Figs. 8-17 to 8-20), extension (see Figs. 8-37 to 8-40), and lateral flexion (see Figs. 8-53 to 8-56) are described later in this chapter. A goniometer is not commonly used to measure rotation of the thoracolumbar spine. The American Medical Association1 (AMA) has published its Guides to the Evaluation of Permanent Impairment, in which the use of inclinometers has been stipulated as “a feasible and potentially accurate method of measuring spine mobility.” Therefore, it can be suggested that the use of the inclinometer for appropriate measurement of spinal mobility appears to have gained acceptance. Several options are available for the use of the inclinometer in measuring spinal movement. Two inclinometers can be used simultaneously to measure spinal movement (referred to as the double-inclinometer method). Or, one inclinometer can be used to measure the same spinal movement (referred to as the single-inclinometer method). In addition, the inclinometer can be held against the subject during the examination of ROM, or the inclinometer can be strapped onto and attached to the individual (Back range of motion [BROM] device). All these techniques have been accepted by the AMA1 as appropriate methods for measurement of spinal mobility. This chapter describes use of dual-inclinometer technique to measure movement of the lumbar and thoracic spine for flexion (see Figs. 8-21 to 8-24), extension (see Figs. 8-41 to 8-44), lateral flexion (see Figs. 8-57 to 8-60), and rotation (see Figs. 8-69 to 8-71).
MEASUREMENT of RANGE of MOTION of the THORACIC and LUMBAR SPINE
ANATOMY AND OSTEOKINEMATICS
LIMITATIONS OF MOTION
FUNCTIONAL RANGE OF MOTION
TECHNIQUES OF MEASUREMENT
Flexion and Extension
Lateral Flexion

Goniometer
Inclinometer
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


MEASUREMENT of RANGE of MOTION of the THORACIC and LUMBAR SPINE