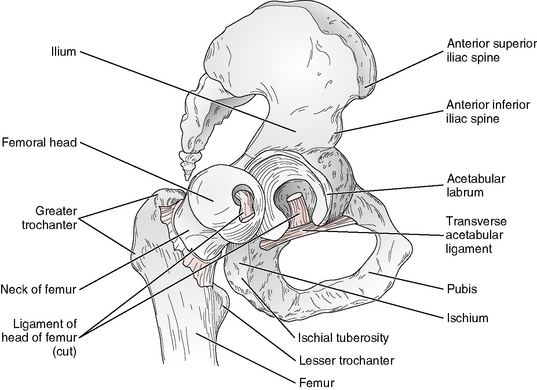
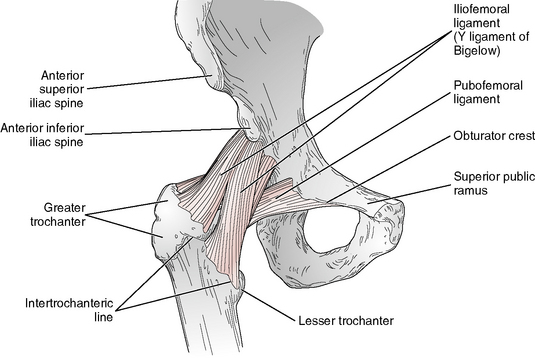
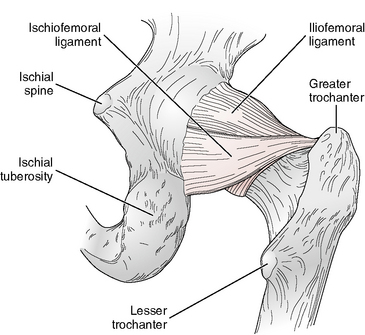
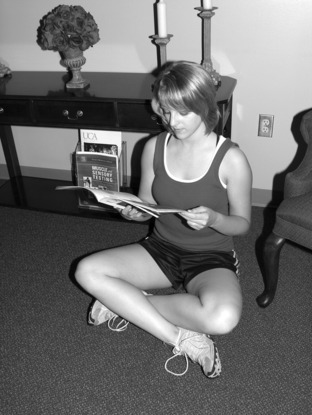
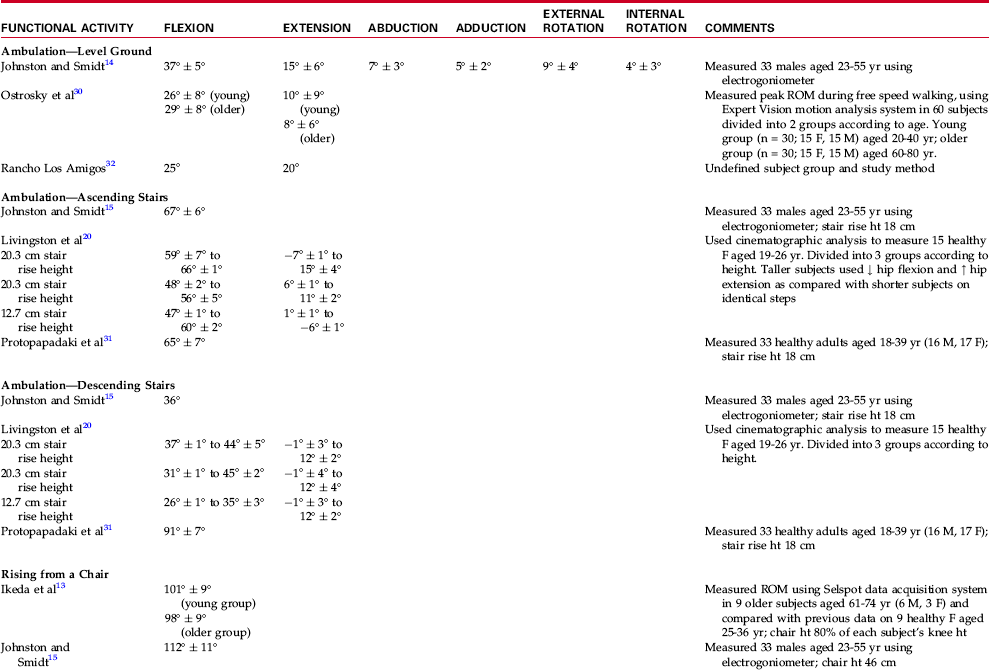
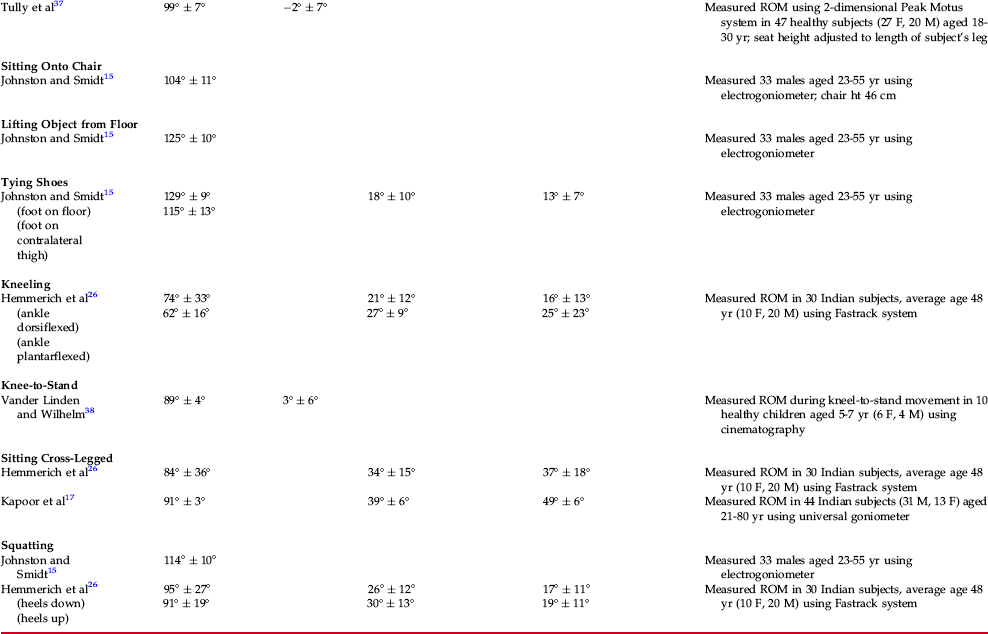
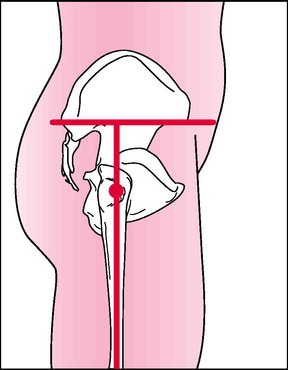
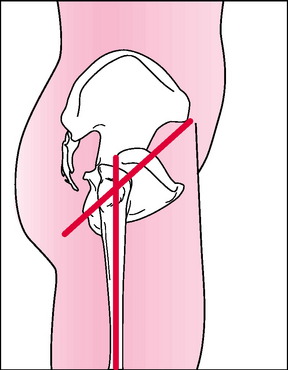
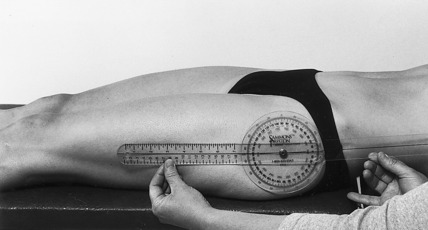
Chapter 11 The hip is a ball-and-socket joint that consists of an articulation between the convex head of the femur and the concave acetabulum of the pelvis, or hip bone (Fig. 11-1). All three bones that make up the pelvis (ilium, ischium, and pubis) contribute to the acetabulum, which provides a deep, cup-shaped receptacle for the spherically shaped femoral head. A fibrocartilaginous rim, the acetabular labrum, attaches to the margin of the acetabulum, further increasing its depth.4,25 Thus the hip, unlike the glenohumeral joint, has a great deal of inherent bony stability and is less dependent on muscular and ligamentous structures for support. The articular capsule of the hip joint is strong and is crossed by three ligaments that provide additional reinforcement. The iliofemoral ligament is shaped like an inverted Y and reinforces the anterior joint capsule (Fig. 11-2). The stem of the iliofemoral ligament is attached to the anterior inferior spine of the ilium, and its two branches are attached along the whole length of the intertrochanteric line of the femur.4,25 The pubofemoral ligament lies along the medial and inferior part of the joint capsule, running from the superior ramis of the pubis and the pubic portion of the acetabular rim to the neck of the femur (see Fig. 11-2). Reinforcing the posterior aspect of the joint capsule is the ischiofemoral ligament (Fig. 11-3). This ligament arises from the ischial portion of the acetabulum and spirals upward across the posterior aspect of the femoral neck to insert into its superior aspect, just medial to the root of the greater trochanter.9,21,25 Movement at the hip, which occurs in all three of the cardinal planes, consists of flexion, extension, abduction, adduction, medial rotation, and lateral rotation. These motions may be achieved by movement of the femur on the pelvis or by movement of the pelvis on the femur. The pelvic movements of anterior and posterior tilting produce flexion and extension of the hip, respectively. Tilting of the pelvis laterally produces hip adduction on the high side and hip abduction on the lower side of the pelvis. Rotation of the pelvis in the transverse plane results in lateral rotation of the hip ipsilateral to the more anteriorly displaced pelvis and medial rotation of the contralateral hip. An additional motion, circumduction, has been described as occurring at the hip joint. This motion is a sequence of flexion, abduction, extension, and adduction and is not normally measured with a goniometer.4,19,28 During motions of the hip, the convex femoral head moves within the concave acetabulum. A pure spin of the femoral head within the acetabulum occurs during flexion and extension of the hip.28 Other motions of the hip produce a combined roll and glide of the femoral head in the opposite direction of the distal femur. Most of the motions at the hip are limited by the ligaments (iliofemoral, ischiofemoral, and pubofemoral) and muscles that surround the joint, as well as by the hip joint capsule. The primary exception to this rule is hip flexion, which frequently is limited by approximation of the soft tissue between the anterior thigh and the abdomen when the knee is flexed. Hip flexion and extension range of motion are dependent on the position of the knee during movement. Full hip flexion is obtained only with the knee flexed. If the hip is flexed with the knee extended, tension in the hamstring muscles limits the motion. Likewise, full hip extension requires that the knee is extended, and in this position, motion is limited by tension in the iliofemoral ligament.4,9 Extending the hip with the knee fully flexed typically decreases the available hip extension range of motion subsequent to tension in the rectus femoris muscle. Adduction of the hip is limited by contact with the contralateral limb and by tension in the lateral portions of the iliofemoral ligament and the hip abductor muscles.5 Hip abduction is limited by tension in the pubofemoral ligament. Medial rotation of the hip is limited by tension in the ischiofemoral ligament, the posterior aspect of the articular capsule, and the lateral rotator muscles.21 Lateral rotation is limited by the medial and lateral fibers of the iliofemoral ligament, as well as by tension in the tensor fasciae latae and the iliotibial band.4,28 Information on normal ranges of motion for all motions of the hip is found in Appendix B. Normal end-feels for hip extension, abduction, adduction, medial rotation, and lateral rotation are firm, as a result of capsular and ligamentous limitations of motion. The normal end-feel for hip flexion with the knee flexed is soft (soft tissue approximation), whereas the normal end-feel for hip flexion with the knee extended is firm, owing to muscular tension in the hamstring group.4,19 The experts have expressed slight disagreement when describing the capsular pattern in the hip. Cyriax6 states that flexion, abduction, and medial rotation are all “grossly” limited; extension is less limited than flexion, abduction, and medial rotation; and lateral rotation has no limitation. Although Kaltenborn16 agrees that lateral rotation is the least limited, he states that medial rotation is most limited, followed by limitations in extension, then abduction and flexion. Several studies investigating motion of the hip joint during functional activities are described in the literature. Research has involved the examination of a variety of functional activities, including walking on level surfaces,15,29,30,32,36 ascending and descending stairs,16,20,31 sitting onto and rising from a chair (Fig. 11-4),13,16,37 lifting an object from the floor, tying a shoe (Fig. 11-5),16 and transitioning from a kneeling to a standing position.38 A few authors also have examined hip motion in so-called high range of motion activities such as kneeling, squatting, and sitting cross-legged (Fig. 11-6).12,16,17,26 A summary of hip range of motion as it relates to various functional activities is located in Table 11-1. Most of the studies from which data were derived were performed in healthy adults, although some investigations included elderly and pediatric subjects. Essentials of the study populations and instrumentation used are included in the table. Caution should be used in extrapolating these data to the general population because the sample sizes for all studies were small. For more in-depth information on each study, the reader is referred to the reference list at the end of this chapter. A variety of techniques have been employed to measure hip flexion. Measurements have been taken with the patient in the supine position with the contralateral hip flexed or extended (Figs. 11-7 and 11-8)1,10 and with the patient in a side-lying position, using the Mundale27 (Fig. 11-9) or the pelvifemoral angle technique22 (Fig. 11-10). These techniques vary in terms of patient positioning, specific landmarks used for goniometric alignment, and the degree to which each method controls for pelvic motion. Values for the normal maximum amount of hip flexion that are provided in the literature vary widely (see www.wbsaunders.com/SIMON/Reese/joint/). Such discrepancies in standards for the normal hip appear to be caused by the technique used and the degree to which each of the different techniques controls for pelvic motion. Of the techniques provided in the preceding list, the one recommended by the American Academy of Orthopaedic Surgeons (AAOS) and the American Medical Association (AMA) places the least emphasis on controlling pelvic motion.1,10 Motions of the pelvis on the lumbar spine during measurement of hip flexion or extension can artificially inflate the range of motion measurement obtained. To control for this phenomenon, one should use landmarks on the pelvis to eliminate the possibility of including lumbar spine motion in the measurement, or one should manually ensure that the pelvis remains in a neutral position at the beginning and end of the range of motion measurement. The neutral position of the pelvis has been described as the position in which a line drawn through the anterior superior iliac spines (ASIS) and the symphysis pubis is vertical and lies in the frontal plane.18,35 With the pelvis in this position, a line connecting the anterior and posterior superior iliac spines of the pelvis is horizontal and lies in the transverse plane.19 According to the Mundale technique,27 the line through the iliac spines is used as the pelvic reference for hip flexion and extension goniometry, and the stationary arm of the goniometer is positioned perpendicular to this line (see Fig. 11-9). Using the pelvis for alignment of the stationary arm of the goniometer eliminates the possibility of including motion of the lumbar spine in goniometric measurements of hip flexion and extension. A second technique, which uses landmarks on the pelvis for alignment of the stationary arm of the goniometer, is the pelvifemoral angle technique.23 When using this technique, the examiner aligns the stationary arm of the goniometer parallel to a line that extends from the ASIS through the ischial tuberosity of the pelvis (see Fig. 11-10). When the Mundale or the pelvifemoral angle technique is used, the moving arm of the goniometer is aligned along the midline of the femur toward the lateral femoral epicondyle, while the axis is placed on the greater trochanter.23,27 With either technique, the patient is placed in a side-lying position to allow the examiner access to the indicated bony landmarks. Other techniques recommended for measuring hip flexion and extension use landmarks on the trunk or the examining table for alignment of the stationary arm of the goniometer.1,10,24 The danger in using these landmarks is the possibility that lumbar motion may be included in measurements of hip motion, thus creating unreliable goniometric measurements. However, if the pelvis is maintained in a neutral position (see the previous description), then a line through the midline of the trunk will parallel a line connecting the ASIS and the pubic symphysis, thus providing a reliable reference for the stationary arm of the goniometer. The use of such a reference is advantageous because it allows the patient to be placed in a supine (flexion) or a prone (extension) position during the measurement, thus providing greater stability of the pelvis. Additionally, the need for marking lines on, or taping, the patient is avoided. Whenever landmarks on the trunk are used for alignment of the goniometer’s stationary arm, extreme care must be taken, as indicated previously, to maintain the pelvis in a neutral position through manual monitoring of pelvic motion and patient positioning. Both the AAOS and the AMA direct that the patient’s contralateral hip should be flexed during measurements of ipsilateral hip flexion1,10; however, maintaining the contralateral thigh against the examining table is necessary to minimize pelvic motion during the measurement.18 Therefore, the technique of measuring hip flexion described in this text recommends extension of the contralateral hip during the measurement. Measurement of hip extension range of motion also can be accomplished using the Mundale and pelvifemoral angle techniques. Additionally, the AAOS describes two methods of measuring hip extension, both of which use a proximal goniometer alignment that is parallel to the tabletop and to a line through the lateral midline of the trunk.10 The patient is placed in the prone position for both AAOS techniques; the only difference in the two techniques is that the patient’s contralateral hip is extended in one technique and is flexed over the end of the examining table in the other. Some examiners also use the Thomas technique (used for measuring hip flexion contracture; see Chapter 14) to measure hip extension.2 In a comparison of four of these techniques, Bartlett et al2 reported the highest intrarater and inter-rater reliabilities for the AAOS (contralateral hip flexed) and Thomas techniques in children with myelomeningocele and spastic diplegia (see Chapter 15). Although the contralateral hip may be extended or flexed during measurements of hip extension range of motion (ROM), fewer patients may have difficulty extending the hip while lying prone than while standing and leaning over an examining table. Measurement of hip abduction and adduction is most commonly done with the patient positioned supine and the ipsilateral hip positioned in 0 degrees of extension. The hip is maintained in 0 degrees of extension throughout the measurement.1,10,24 However, hip abduction occasionally is measured with the ipsilateral hip maintained in 90 degrees of flexion throughout the measurement.10 This technique appears to be used primarily in the pediatric population and may be less reliable than measurement of hip abduction with the hip extended.7 Hip abduction and adduction also may be measured with an inclinometer if the subject is placed in a side-lying position. Measurements of iliotibial (IT) band tightness, attained through this method, have been shown to have high reliability.33 Although measurement of hip abduction and adduction with the inclinometer is not demonstrated in this chapter, measurement of IT band tightness using this technique may be found in Chapter 14. Rotation of the hip is generally measured with the patient’s hip in 90 degrees of flexion (patient seated) or with the hip in the anatomical position of 0 degrees of extension (patient prone or supine). In the literature, disagreement exists over which position, if either, allows the greater amount of hip rotation. Haley11 reported a decrease in medial and lateral active hip rotation in the supine, as compared with the seated position, whereas Simoneau et al34 reported increased active hip lateral, but not medial, rotation when measured in the prone, as compared with the seated, position. Results reported by Simoneau et al were supported by Bierma-Zeinstra and colleagues,3 who reported that both medial and lateral hip rotation were greater when measured in the prone, as compared with the supine or seated, position. Ellison et al8 found no difference in the amount of medial and lateral rotation of the hip in the prone compared with the seated position, although this group measured passive, but not active, hip rotation. Additionally, the amount of motion measured at the hip may differ depending on the measurement tool used. Bierma-Zeinstra and colleagues3 found significantly higher measurements of hip external rotation range of motion when they measured movement with the goniometer as compared with measurements obtained with an inclinometer. Conversely, the inclinometer yielded significantly greater measurements of hip flexion and extension than did the goniometer. Unfortunately, most sources reporting standards for hip rotation range of motion (e.g., AAOS, AMA) do not include descriptions of the position in which rotation of the hip was measured, nor do many describe the instrument used to measure the motion. Available data for normal ranges of hip rotation are reported in Appendix B. Because there appears to be no difference in the reliability of measurements of hip rotation taken with the hip flexed or extended,34 and because information is mixed regarding whether the inclinometer or the goniometer is most reliable for measuring hip rotation ROM3 the examiner may choose either method or instrument for performing measurements of this motion. However, care should be taken, as always, to use identical techniques whenever repeated measures are taken, in that the amount of motion may vary depending on patient position and the instrument chosen.3,11,34 The techniques described in this text for measuring hip rotation include those in both seated and prone positions with the goniometer and the inclinometer.
MEASUREMENT of RANGE of MOTION of the HIP
ANATOMY
OSTEOKINEMATICS
ARTHROKINEMATICS
LIMITATIONS OF MOTION: HIP JOINT
END-FEEL
CAPSULAR PATTERN
ROM and Functional Activity
TECHNIQUES OF MEASUREMENT: HIP FLEXION/EXTENSION
TECHNIQUES OF MEASUREMENT: HIP ABDUCTION/ADDUCTION
TECHNIQUES OF MEASUREMENT: HIP MEDIAL-LATERAL ROTATION