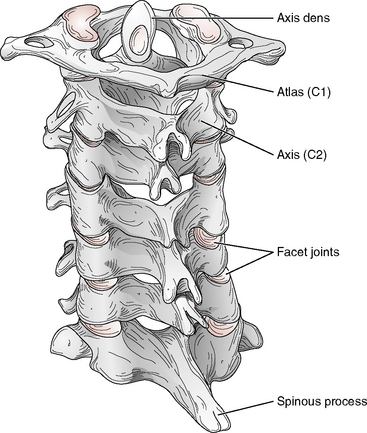
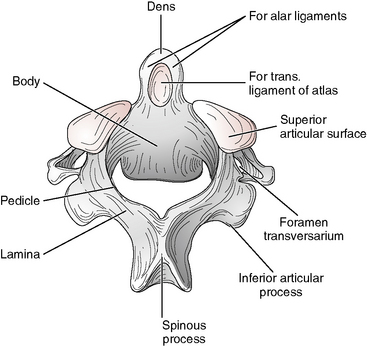
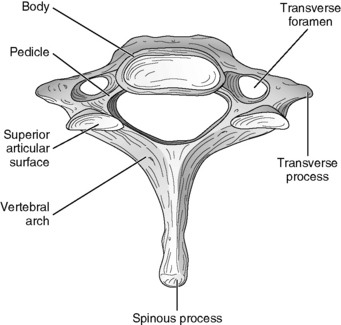
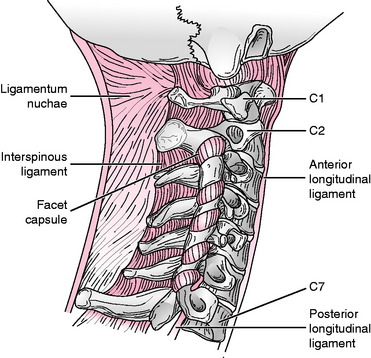
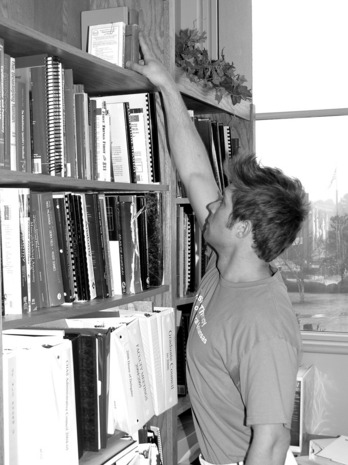
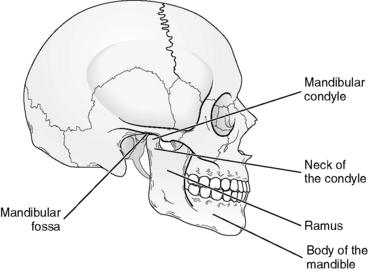
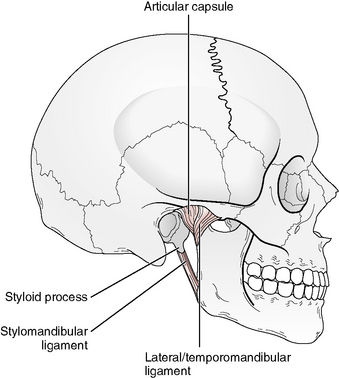
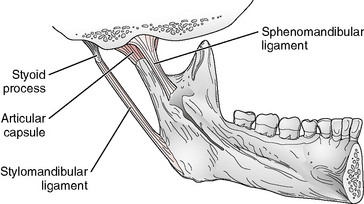
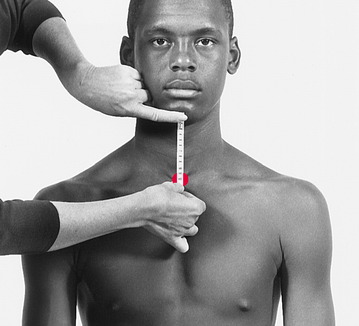
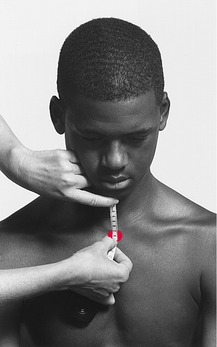
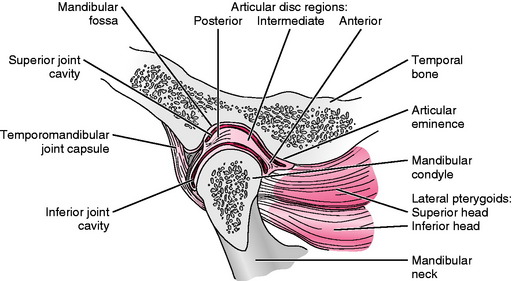
Chapter 9 The following discussion of the cervical spine is a synopsis of information presented in several contemporary sources.7,8,11,13 The cervical region of the spine is made up of two anatomically and functionally distinct regions: the suboccipital region and the lower cervical region. The bones of the suboccipital region include the occipital bone and the first and second cervical vertebrae (C1-C2); the third through the seventh cervical vertebrae (C3-C7) make up the lower cervical region (Fig. 9-1). The atlas (C1) has no body or spinous process and is shaped like a ring (Fig. 9-2). Articulation between the two superior facets of the atlas and the two condyles on the occiput of the skull forms the atlanto-occipital joint. Movement between the atlas and the occiput (atlanto-occipital joint) is primarily a nodding motion in the sagittal plane about a medial-lateral axis. The axis (C2) has a vertical projection called the dens (also known as the odontoid process) that arises from the superior surface of the body. The dens of the axis fits into a ring formed by the anterior arches of the atlas and the transverse (cruciform) ligament so that the atlas pivots around the dens of the axis. Fifty percent of rotation in the cervical spine occurs at the atlantoaxial joint. The C3-C7 vertebrae have common structural features that are considered typical for the spine. These features are presented in Figure 9-3. A general overview of the connective tissue of the cervical spine includes the intervertebral discs, which connect the vertebral bodies starting with C2-C3 and below that form intervertebral cartilaginous joints. The supporting ligaments include: anterior longitudinal, posterior longitudinal, ligamentum flavum, interspinous, ligamentum nuchae, and the joint capsules of the facet joints (Fig. 9-4). The facet joints are located laterally on each side of the spine and are formed by the articulation of the facet surfaces of the two vertebrae. These facet joints occur in pairs in the cervical spine, with the inferior facet of the superior cervical vertebrae (oriented inferiorly and anteriorly) articulating with the superior facet surface of the inferior vertebrae (oriented superiorly and posteriorly) (see Fig. 9-1). Limitation of motion in the first two cervical vertebrae is due to a ligamentous support system specific to this area of the spine. This support structure at the atlanto-occipital and atlantoaxial joints includes the tectorial membrane and the atlantoaxial (anterior and posterior), alar, and transverse ligaments. From C2 to C7, the anterior longitudinal ligament and the contact of the spinous processes limit excessive extension. Flexion is limited by the same ligaments that limit flexion in the lumbar spine (the posterior longitudinal, ligamentum flavum, and interspinous ligaments), with the addition of the ligamentum nuchae in the cervical spine. Running along the tips of the spinous processes of the cervical spine, the ligamentum nuchae is actually a continuation of the supraspinous ligament. Lateral flexion is limited by the bony configuration of the saddle-shaped surface of the vertebral body, and rotation is limited by the fibers of the annulus fibrosus of the disc. Appendix B provides information regarding normal ROM of the cervical spine. The cervical spine is more mobile than the thoracic and the lumbar spine and is designed to meet the requirements of positioning of the head in space and moving to alter the visual field.11 Limitations in cervical ROM may restrict the ability of a person to perform those tasks that require full ROM or may cause the person to adapt by using trunk movement. Bennett et al5 reported on the amount of cervical ROM required for 13 daily functional tasks in 28 subjects (aged 21 to 26 years). Activities that required the greatest amount of cervical ROM were reported to be looking over the shoulder when driving a car in reverse (rotation) (Fig. 9-5), placing an object on a high shelf (Fig. 9-6), drinking from a glass (Fig. 9-7), putting on socks (Fig. 9-8), and washing hair in the shower. Cutting with a knife, holding a telephone to the ear, reading a newspaper, rising from a chair, opening a door, pouring from a pitcher, writing at a table, and working on a computer did not result in much cervical ROM. In Chapter 8, which describes measurement of the thoracic and lumbar spine, it is noted that the American Medical Association (AMA) has accepted the inclinometer as “a feasible and potentially accurate method of measuring spine mobility.”2 This statement was directed not only at examination of the thoracic and lumbar spine but also at measurement of the cervical spine. Specifically included in the Guides to the Evaluation of Permanent Impairment2 is the use of single and double inclinometers that are held in place manually. Attachment of Inclinometer to the Head: The process of attaching an inclinometer to the head to measure cervical ROM has undergone a sort of evolution, beginning with the inclinometer attached to the ears and worn as headphones in the early 1960s and progressing, with increasing sophistication, to use of the cervical range of motion (CROM) device (Performance Attainment Associates, Roseville, MN) in the late 1990s. This evolution included the “bubble goniometer,”4 the attachment of the inclinometer to the head with elastic straps,3 a “cloth helmet,”1 the use of rigid headgear with three scales calibrated in degrees mounted on a skull cap,9 the use of an inclinometer mounted on a wood block and placed on the head,15 the “rangiometer,”17 and finally, the CROM device.16 Although not included in the Guides to the Evaluation of Permanent Impairment,2 the CROM device has been widely adopted by clinicians. The temporomandibular joint (TMJ) is unique in that the mandible has two articulations with the temporal bone, forming two separate but solidly connected joints (see Fig. 9-9). The two joints must be considered together in any examination. In addition, each TMJ has a disc that completely divides each joint into two cavities (Fig. 9-10). Movement that occurs in the upper cavity (the joint formed by the temporal bone and the superior surface of the disc) is a gliding or translatory motion, and movement that occurs in the lower cavity (the joint formed by the mandibular condyle and the inferior surface of the disc) is a rotatory or hinge movement. Fig. 9-10 View of TMJ indicating relationship disc separating the temporal bone and the mandibular condyle. The primary ligament reinforcing the TMJ is the lateral temoporomandibular ligament, which serves to provide stability to the lateral capsule (Fig. 9-11). Medial to the joint capsule, the stylomandibular and sphenomandibular ligaments are accessory ligaments to the capsule (Fig. 9-12). Movement of the mandible involves bilateral action of the TMJ. Abnormal function of one joint interferes with the function of the other. Movement of the TMJ occurs by a process that combines rotation of the mandible, in which the mandibular condyles roll onto the inferior surface of the disc, and translation of the combination of the mandibular condyle and the disc, which move onto the mandibular fossa of the temporal bone. For a detailed description of the condyle-disc-complex translation, the reader is referred to Levangie and Norkin.11 Stentpetery14 defined functional mandibular depression (opening) as the minimal amount of movement needed in the TMJ to eat and speak without problems. This author defined functional mandibular depression as 25 to 30 mm. Kraus10 described functional mandibular depression as the “patient’s ability to actively open his or her mouth to 40 mm.” Magee12 suggested that “only 25 to 35 mm of opening is needed for everyday activity.” Friedman and Weisberg6 suggested that the amount of functional opening varies according to the individual’s size, and that on average, an individual should be able to place two to two-and-a-half knuckles between the upper and lower incisors.
MEASUREMENT of RANGE of MOTION of the CERVICAL SPINE and TEMPOROMANDIBULAR JOINT
CERVICAL SPINE
LIMITATIONS OF MOTION: CERVICAL SPINE
FUNCTIONAL RANGE OF MOTION: CERVICAL SPINE
TECHNIQUES OF MEASUREMENT: CERVICAL SPINE
Inclinometer
TEMPOROMANDIBULAR JOINT
FUNCTIONAL RANGE OF MOTION: TEMPOROMANDIBULAR JOINT
Get Clinical Tree app for offline access