CHAPTER 24 Management of the Infected Shoulder Arthroplasty
Infection after shoulder arthroplasty is a rare but devastating complication. The reported incidence in the literature for unconstrained primary shoulder arthroplasty ranges from 0% to 4%.1,2 In the literature, limited information is available on the treatment of the infected shoulder prosthesis. Therefore, the rationale behind the evaluation as well as treatment of the infected shoulder prosthesis is derived in large part from the hip and knee arthroplasty literature. This chapter reviews the evaluation of a patient with an infected shoulder arthroplasty, outlines management options, and discusses expected outcomes with specific treatments.
PATIENT EVALUATION
Classification
An accurate history is critical to determining the time course of infection as well as assisting in classification. Gustilo and colleagues proposed a classification system based on the interval of time between the arthroplasty procedure and the onset of infection.3 In addition to defining the time course of the infection, this simple classification can be used to guide treatment options. There are four types:
Physical Examination
The physical examination starts with careful inspection of both upper extremities. One looks for signs of muscle atrophy as well as the status of prior incisions. Erythema may be present as well as a sinus tract. One should be concerned if the wound has a reddish, cellulitic appearance after shoulder arthroplasty. In many of these patients, the symptoms are misinterpreted to result from a superficial infection when a deep prosthetic infection may be present. One should also look for swelling and palpate the shoulder to determine if tenderness is present. Atrophy, associated with long-standing rotator cuff disease or potential nerve injury, should be noted. One must pay close attention to the integrity of the deltoid, particularly among patients who have undergone prior surgery. Cervical range of motion is assessed as well as midline and paraspinal tenderness. Spurling’s test is performed to evaluate for possible cervical radiculopathy. A bilateral examination is performed and includes the shoulder, elbow, and wrist. Upper extremity reflexes, strength, and sensation are also recorded.
Diagnostic Studies
Blood work typically includes a C-reactive protein, erythrocyte sedimentation rate, and complete blood cell count. In the early postoperative setting, however, these values may be nonspecific. In addition, there is little information on the relative time frame for these values to return to normal specifically after shoulder arthroplasty. Therefore, the best information available in regard to understanding these values in the postoperative period resides in the hip and knee arthroplasty literature. The C-reactive protein typically peaks around the second postoperative day after joint arthroplasty.4 However, it may remain elevated in cases of diffuse inflammatory arthritis.5
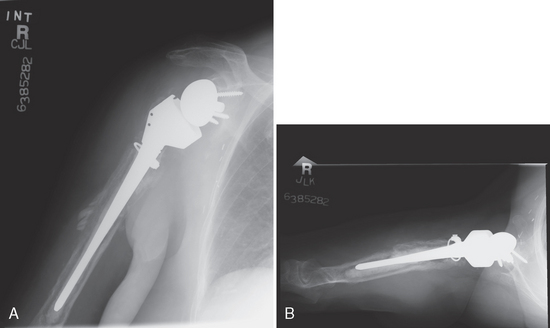
It is helpful to review serial postoperative radiographs. Fluoroscopically positioned radiographs are very useful in looking for periprosthetic lucency, osteolysis, and frank component loosening. In addition, periosteal new bone formation can occur in the setting of infection (Fig. 24-1).6 One may also consider an indium leukocyte bone scan. This test may be more accurate than a bone scan alone to detect infection. However, patients with an underlying inflammatory disease may be more likely to have a false-positive result. In addition, there are no data on the sensitivity and specificity of indium scans after shoulder arthroplasty.
Aspiration of the joint is an important component of the work-up process to evaluate for potential infection. At our institution, the patient undergoes fluoroscopically guided aspiration of the shoulder to ensure that fluid is obtained from the correct location. In addition, the aspiration can be performed from a posterior approach if anterior cellulitis is present. A critical component of obtaining an accurate aspiration involves making sure that the patient has been off of antibiotics for several weeks before this test. In addition, one needs to be sure that the cultures are held for an appropriate amount of time. Propionibacterium acnes is one of the most common organisms responsible for infection in the shoulder. It has been found to be one of the primary agents responsible for infection after rotator cuff surgery,7 instability surgery,8 operative treatment of proximal humerus fractures,9 and shoulder arthroplasty.1 It is critical for the cultures to be kept for a minimum of 7 days. If there is enough aspirate for a white blood cell count and differential, this may be quite helpful in making the diagnosis. A negative aspiration suggests that an infection is not present. However, in our experience, patients with negative aspirations may have positive cultures taken at the time of revision surgery. Therefore, patients are counseled that they might still have a low-grade infection despite a negative aspiration.
New molecular techniques are being investigated to assist in making the diagnosis of an infection in the setting of a joint arthroplasty.10 One of these techniques involves polymerase chain reaction to evaluate for organisms. These techniques can employ ultrasound to dislodge any organisms from the implants. This is a promising technique that might play a larger role in the future.
Diagnosis
Diagnosis of infection can be challenging, particularly among patients undergoing revision shoulder arthroplasty. Many of these patients do not present with overt signs of infection such as erythema or sinus tracts. Topolski and colleagues11 have reported on the value of preoperative studies and intraoperative histology among patients who underwent revision shoulder arthroplasty and had positive intraoperative cultures. The authors reviewed the results of 75 shoulders that had no overt signs of infection and that underwent revision shoulder arthroplasty. In regard to preoperative studies, the white blood cell count was negative in 67 of 72 (93%), 64 of 70 (91%) polymorphonuclear percentage distributions were negative, and 36 of 42 (86%) erythrocyte sedimentation rates were negative. Among 16 patients in whom C-reactive protein was measured, the test was negative in 12 (75%). The intraoperative histology was negative in 67 of 73 patients (92%). The most common organism was P. acnes in 45 of 75 cases. The mean time for the first growth was 5.1 days. The authors concluded that there are no good intraoperative or preoperative studies to detect who will have a positive intraoperative culture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree