An understanding of the three-dimensional components of spinal deformity in children with cerebral palsy is necessary to recommend treatments that will positively affect these patients’ quality of life. Management of these deformities can be challenging and orthopedic surgeons should be familiar with the different treatments available for this patient population. This article discusses the incidence, causes, natural history, and treatment of patients with scoliosis.
An understanding of the three-dimensional components of spinal deformity in children with cerebral palsy (CP) is necessary to recommend treatments that will positively affect these patients’ quality of life. Management of these deformities can be challenging and orthopedic surgeons should be familiar with the different treatments available for this patient population.
Incidence
The incidence of scoliosis in CP varies greatly, from 6% to almost 100%; but the generally accepted incidence in the overall CP population is 20% to 25%. The rate varies depending on the particular study, the type of CP, the severity of neurologic involvement, and ambulatory status. The incidence is highest in patients with spastic CP (about 70%) and lowest in those with athetoid type (from 6%–50%). Madigan and Wallace, in their survey of institutionalized CP patients published in 1981, found that 64% of the 272 patients studied had scoliosis greater than 10 degrees on screening radiographs and that the incidence of scoliosis was related to severity of neurologic involvement. In support of this conclusion, they pointed to the inverse relationship of ambulatory status and scoliosis (44% of independent ambulators, 54% of dependent ambulators, 61% of independent sitters, and 75% of dependent sitters or bedridden residents). Patients with subluxated or dislocated hips (an indicator of disease severity) were also found to have a 75% to 77% incidence of scoliosis. Interestingly, there was no difference between patients with unilateral or bilaterally dislocated hips, underscoring the importance of severity of involvement rather than the balance of the pelvis. Kalen and colleagues found that none of their patients with curves greater than 45 degrees were ambulators, whereas 34% of those with curves less than 45 degrees were. The incidence of scoliosis is directly related to their gross motor function classification system (GMFCS) level.
Cause
The cause of scoliosis in CP is not entirely clear, but is thought to be due to some combination of muscle weakness, truncal imbalance, and asymmetric tone in paraspinous and intercostal muscles. Whether the development of scoliosis is due to the primary cerebral insult or due to its secondary consequences is also unclear. In addition, there is some data to suggest that certain spasticity treatments, namely selective dorsal rhizotomy (SDR) and intrathecal baclofen, may result in progressive scoliosis. SDR is done with the intention of decreasing the spasticity. It has been implicated by some investigators in increasing spinal deformities with the incidence of scoliosis ranging from 16% to 57%. Other investigators, however, have demonstrated no significant spinal deformity following SDR. Spiegel and colleagues reported scoliosis in only 17% of their ambulatory CP patients. Recently, Langerak and colleagues evaluated the long-term follow-up of their patients who underwent SDR 17 to 26 years prior and compared this to the short-term results of those same patients. They found 57% of patients at long-term follow-up had scoliosis while none of the patients at short-term follow-up demonstrated scoliosis. The majority of curves were less than 30 degrees. Whereas this was statistically significant, it was not felt to be clinically important. The relationship between SDR and long-term, clinically significant spinal deformity is still unclear, but it is generally felt to be safe when done with great attention to maintaining the integrity of the laminae. The ideal candidates for a SDR are patients with pure spasticity and good trunk control (usually GMFCS I and II). These patients rarely develop scoliosis. SDR should probably not be performed in the GMFCS IV and V patients as they often have a mixed type CP with dystonia predominating.
In the case of intrathecal baclofen, there have been a few retrospective reviews and case reports suggesting more rapid progression of a scoliotic curve following baclofen pump insertion, with the most recent of these studies reporting a sixfold increase. In contrast, Shilt and colleagues compared 50 patients with CP who had intrathecal baclofen pump insertion with matched controls and found no difference. Once again, the patients who receive a baclofen pump are usually the more severely involved patients and, therefore, their natural history is to have progressive scoliosis. As in the case of SDR, a causal relationship between intrathecal baclofen and progressive scoliosis has not been clearly established and further long-term, randomized, prospective study is needed.
Cause
The cause of scoliosis in CP is not entirely clear, but is thought to be due to some combination of muscle weakness, truncal imbalance, and asymmetric tone in paraspinous and intercostal muscles. Whether the development of scoliosis is due to the primary cerebral insult or due to its secondary consequences is also unclear. In addition, there is some data to suggest that certain spasticity treatments, namely selective dorsal rhizotomy (SDR) and intrathecal baclofen, may result in progressive scoliosis. SDR is done with the intention of decreasing the spasticity. It has been implicated by some investigators in increasing spinal deformities with the incidence of scoliosis ranging from 16% to 57%. Other investigators, however, have demonstrated no significant spinal deformity following SDR. Spiegel and colleagues reported scoliosis in only 17% of their ambulatory CP patients. Recently, Langerak and colleagues evaluated the long-term follow-up of their patients who underwent SDR 17 to 26 years prior and compared this to the short-term results of those same patients. They found 57% of patients at long-term follow-up had scoliosis while none of the patients at short-term follow-up demonstrated scoliosis. The majority of curves were less than 30 degrees. Whereas this was statistically significant, it was not felt to be clinically important. The relationship between SDR and long-term, clinically significant spinal deformity is still unclear, but it is generally felt to be safe when done with great attention to maintaining the integrity of the laminae. The ideal candidates for a SDR are patients with pure spasticity and good trunk control (usually GMFCS I and II). These patients rarely develop scoliosis. SDR should probably not be performed in the GMFCS IV and V patients as they often have a mixed type CP with dystonia predominating.
In the case of intrathecal baclofen, there have been a few retrospective reviews and case reports suggesting more rapid progression of a scoliotic curve following baclofen pump insertion, with the most recent of these studies reporting a sixfold increase. In contrast, Shilt and colleagues compared 50 patients with CP who had intrathecal baclofen pump insertion with matched controls and found no difference. Once again, the patients who receive a baclofen pump are usually the more severely involved patients and, therefore, their natural history is to have progressive scoliosis. As in the case of SDR, a causal relationship between intrathecal baclofen and progressive scoliosis has not been clearly established and further long-term, randomized, prospective study is needed.
Differences with Adolescent Idiopathic Scoliosis
There are several key differences between patients with CP and scoliosis and those with adolescent idiopathic scoliosis (AIS). The curves in patients with CP, especially those more profoundly affected, tend to occur at an earlier age than in AIS. They, therefore, have a propensity to develop into larger, and stiffer, curves. As in AIS, larger curves are likely to progress after maturity. Thometz and Simon found that curves greater than 50 degrees at skeletal maturity in patients with severe CP progressed at a rate of 1.4 degrees per year. Unlike AIS, severity of neural involvement, ambulatory status, and curve location also impact the rate of curve progression following skeletal maturity. In addition, skeletal maturity may be delayed in patients with CP; some maintain open growth plates early in the third decade. The shape of the curve in CP may be different than that in AIS. In more severely affected patients with CP, long C-shaped curves and left-sided curves are not uncommon. Madigan and Wallace found an equal distribution between single “C” curves and multiple or “S” curves in their institutionalized patients with scoliosis, although 67% of their bed-ridden group had “C” curves versus only 22% of the independent sitters. In that same study, 14 of the 42 thoracic “C” curves were convex to the left and 12 of the 28 double major curves had a thoracic component convex to the left. The CP curves also typically have greater deformity in the sagittal plane, either being kyphotic or lordotic. Finally, the associated pelvic obliquity seen in the CP patient separates their curve type from the typical AIS patient. As discussed later, these distinctions result in different approaches for the management of CP scoliosis and AIS. For example, bracing is less effective in halting curve progression in CP patients and is less tolerated due to patient comorbidities and movement disorders. The planning and execution of spinal fusion is more difficult as these patients often require longer fusions to the pelvis. More important, many CP patients are more medically fragile than a typical idiopathic patient and often require multidisciplinary management.
Natural history
There have been several studies on the natural history of untreated scoliosis in patients with CP, looking at factors related to progression and at the impact untreated scoliosis may have on the patients’ overall function and health. Factors implicated in progression include type of involvement (quadriplegia), poor functional status (nonambulatory), and curve location (thoracolumbar). Thometz and Simon found that progression was most rapid for thoracolumbar curves, followed by lumbar curves, with thoracic curves having the slowest rate. Saito and colleagues evaluated 37 institutionalized patients with severe spastic CP who were followed for an average of 17.3 years, from childhood to adulthood, and identified the following risk factors for progression: a spinal curve greater than 40 degrees before age 15 years, total body involvement, being bedridden, and a thoracolumbar curve. Untreated severe scoliosis is generally thought to have detrimental effects on patients’ overall health and function specifically the cardiopulmonary system and sitting balance. Majd and colleagues, in their survey of institutionalized adults with CP, found that those patients who experienced a decline in function had the greatest Cobb angle and rate of progression (80 vs 56 degrees and 4.4 vs 3.0 degrees per year respectively). Saito and colleagues found that 20 of their 37 patients required increased amounts of nursing time to complete various activities of daily living. The average Cobb angle for those 20 patients was 73 degrees versus 34 degrees in those patients who did not require increased assistance. Conversely, Kalen and colleagues did not demonstrate any difference in the incidence of decubiti, highest functional level achieved, functional loss, oxygen saturation, or pulse in CP patients with untreated scoliosis greater than 45 degrees as compared with those with mild or no curves. Finally, the importance of sitting balance in significantly affected patients cannot be underestimated. As curve severity increases beyond wheelchair modification capabilities, a patient may need to rely on his or her upper extremities to help maintain an upright position, thereby becoming a “functional quadriplegic.”
Treatment
Nonsurgical
The role of nonsurgical treatment in CP patients with scoliosis is very different than in the AIS population. Nonoperative treatment options still consist of observation and bracing, but also include seating modifications and medical management. The goals of any intervention are to maintain comfortable upright sitting and to allow the functional use of the upper extremities, thereby maximizing a patient’s ability to interact with his or her environment. Observation is indicated for small curves that do not cause any functional deficit. Bracing is used in CP patients but, unlike in AIS, it is not used with the intention of stopping curve progression. There is some evidence that brace use may slow curve progression in CP patients. Unfortunately, this is inconclusive with other investigators demonstrating no clinically significant effect of bracing on curve progression. This may be caused by the great differences in achievement of skeletal maturity in CP. In general, soft braces are tolerated in spastic patients better than rigid orthoses, both in maintaining skin integrity and minimizing respiratory compromise. Bracing should remain an option for physicians treating scoliosis in CP patients, but for different intended purposes than in AIS. They can assist in sitting balance, as well as potentially slow curve progression—especially in young patients or in hypotonic ambulatory patients with short thoracolumbar curves less than 40 degrees.
Another option for patients that are wheelchair-dependent and cannot tolerate a brace is to provide seating modifications. This usually involves adapting a patient’s wheelchair with various supports. It does not alter the natural history of the scoliosis. There are a variety of seating modifications that can be used—from custom-molded seatbacks for patients with severe spinal deformity to 2- and 3-point body support systems. The 3-point force configuration has been shown to achieve the best static correction of the scoliotic spine based on external measurements, but modifications should be individually determined and tailored. Numerous alternative modalities have also been investigated, including physical therapy, electrical stimulation, and botulinum toxin A. Physical therapy and electrical stimulation have not been shown to be effective. Although botulinum toxin A is increasingly being used to treat limb spasticity in CP patients, there is scant evidence for its use in treating scoliosis. Nuzzo and colleagues retrospectively reviewed patients with paralytic scoliosis who had a delay in surgical intervention that were treated with botulinum toxin as a supplement to other treatment modalities. No patient had any worsening of their scoliosis and some had a reduction in their Cobb angle.
Surgical
The definitive treatment for progressive, debilitating scoliosis in patients with CP is surgical intervention, with the goals being to halt progression, level the pelvis, and achieve good frontal and sagittal balance. There is no strict guideline for when surgery is absolutely indicated. Most investigators consider fusion for curves that progress beyond 50 degrees or for those that lead to a deterioration in functional sitting. However, each patient, their families and caretakers, their deformity, and their specific comorbidities must be taken into consideration before embarking on treatment. The physician who treats neuromuscular scoliosis must be prepared to address the inherent complications routinely encountered in this patient population. Thorough preoperative evaluation, coherent multidisciplinary management, careful preoperative surgical planning, and safe intraoperative execution are all required for a successful outcome.
Preoperative evaluation
A comprehensive preoperative evaluation, including history, physical, laboratory, and radiographic studies, is imperative and a multidisciplinary approach is helpful ( Table 1 ).
| Musculoskeletal | Neurologic | Pulmonary | Gastrointestinal or Nutritional | Hematologic | |
|---|---|---|---|---|---|
| History |
|
|
|
|
|
| Physical Examination |
|
|
|
| — |
| Laboratory Tests | — | — | — |
|
|
| Radiographs |
| — |
| — | — |
| Preoperative intervention |
|
|
|
|
|
| Perioperative considerations |
|
|
| — |
|
Musculoskeletal
The history should focus on ambulatory ability and GMFCS level, as well as the details of the patient’s sitting or standing posture, upper extremity function, and any parent or caregiver concerns. In the physical examination, the clinician should note the patient’s overall balance and ability to interact with his or her environment, as well as the level of voluntary muscle control. Depending on functional level, the curvature of the spine should be evaluated in the coronal and sagittal plane when standing, sitting, or supine. A push-pull examination can give some sense of the overall flexibility of the curve. A detailed lower extremity examination should note any hip flexion contractures, which may lead to lumbar hyperlordosis and may make intraoperative prone positioning more difficult. Any significant hamstring tightness should also be noted as it can severely limit hip flexion, leading to “sacral sitting” and decreased lumbar lordosis or increased thoracic kyphosis. Finally, any hip adduction contracture or windswept deformity should also be noted because these are thought to be infrapelvic causes of pelvic obliquity. It is not entirely clear whether the scoliosis or hip asymmetry develops first, or if prevention of hip subluxation or dislocation decreases the frequency or severity of scoliosis, but it is likely that hip asymmetry, pelvic obliquity, and scoliosis are interrelated and may exacerbate each other. In some cases, correction of the spinal deformity may worsen the hip positioning, necessitating further surgical intervention in the hip. Caregivers should be counseled on this before the spinal surgery. Finally, overall skin integrity should be evaluated and any areas of skin maceration or decubiti noted and appropriately treated.
Neurology
Patients with CP may have a concomitant seizure disorder, and it is important to note the presence or absence of any seizure activity, medications used to control the condition, and whether the seizures are well controlled. Certain antiseizure medications have side effects that should factor into perioperative evaluation. Phenytoin, phenobarbital, and valproic acid have all been shown to alter vitamin D metabolism and intestinal calcium absorption. Patients taking any one of these medications will typically have lower bone mineral density, which may impact implant fixation. In addition, valproic acid has been implicated in prolonged bleeding times, excessive blood loss, and increased need for blood products in those patients taking the medication and undergoing spine surgery. Chambers and colleagues found a threefold increased risk of losing greater than 30 mL/kg of blood in patients taking valproic acid who had a single abnormal clotting test. Based on the concern for increased blood loss perioperatively, consideration should be given to replacing valproic acid with another antiepileptic medication, preferably at least 1 month before surgery. Finally, it should be noted whether the patient has had an intrathecal baclofen pump placed. In most cases, the pump must be turned off if intra-operative neuromonitoring is to be used. Proper supplies to repair the tubing should be available if an inadvertent break occurs during the course of the surgery. In some cases, an elective ligation can be done to minimize the risk of pulling it out of the thecal sac with a repair done before incision closure.
Pulmonary
Patients with CP are already prone to poor pulmonary function due to many causes such as abnormal oropharyngeal tone and anatomic abnormalities. This diminished respiratory status may be further exacerbated by a large scoliotic curve. Formal pulmonary function tests are difficult and unreliable in significantly affected patients. Indirect signs of vital capacity include crying, laughing, and vocalizations. Impaired vital capacity and forced expiratory volume in the first second increases the risk for prolonged mechanical ventilation. The frequency of pneumonia over the preceding year is one of the predictors of postoperative pulmonary complications, and frequent coughing, choking, and sputtering during feedings may be a sign of aspiration risk. Patients at increased risk for aspiration may benefit from a gastrostomy tube (G-tube) and possible Nissen fundoplication before spine surgery.
Gastrointestinal or nutritional
Gastroesophageal reflux (GERD) and malnutrition play important roles in the perioperative evaluation. Many CP patients have significant GERD, which places them at increased risk of aspiration, reactive airway disease, and diminished nutritional status. Borkhuu and colleagues recently demonstrated that preoperative GERD with feeding difficulties resulted in a 52% increased chance in developing postoperative pancreatitis, resulting in a longer hospital stay. Malnourishment has been shown to increase the risk of postoperative complications in this patient population; weight for chronologic age below the fifth percentile is associated with an increased postoperative complication score. In addition, it has been shown that CP patients with a preoperative serum albumin less than 35 g/L and total blood lymphocyte count less than 1.5 g/L have an increased infection rate, longer length of intubation, and longer hospital stay. Preoperative labs should include measures of nutrition (albumin, prealbumin, total blood lymphocyte count) and, if low, procedures to optimize feeding orally or via G-tube should be taken to improve nutritional status before surgery.
Hematologic
Patients with neuromuscular scoliosis are at risk for significant perioperative blood loss with some cases exceeding 200% of a patient’s blood volume. This may be due to many factors, including need for longer fusion, poor nutritional status, use of medications such as valproic acid, and a decrease in clotting factors. Attention should be paid to any history of excessive bleeding in prior surgeries. Standard labs include hemoglobin level, prothrombin time, partial thromboplastin time, platelet count, and bleeding time. A more thorough coagulation work-up should be undertaken if there is a history of excessive bleeding during previous surgeries. Preoperative recombinant human erythropoietin, which has been shown to decrease perioperative transfusion rates in idiopathic and adult patients, has not been shown to have a significant clinical benefit in neuromuscular patients.
Imaging studies
Standard radiographs include anteroposterior and lateral of the entire spine, standing or seated if possible. The anteroposterior should be evaluated for curve type, curve magnitude, spinal balance, spinal rotation, and amount and direction of pelvic obliquity. Pelvic obliquity can be measured several ways, but is most reliable when measured from the horizontal; that is, the angle subtended by a line drawn across the top of the iliac crests and the perpendicular to a line drawn from T1 and S1. The hips should be evaluated for subluxation or dislocation. The lateral is important for assessing overall sagittal balance, as well as evaluating for spondylolisthesis, because the incidence in patients with spastic diplegia has been reported as high as 21%. A variety of special films can be taken to assess the flexibility of the spinal deformity, including bending, fulcrum bending, push-pull, and traction. In general, for this patient population, voluntary side-bending radiographs cannot be reliably obtained and traction radiographs are therefore preferred.
Surgical planning and perioperative considerations
There are several considerations to address when planning surgical correction of scoliosis in CP patients. These include the extent of the fusion, what type of instrumentation to use, and whether an anterior approach is indicated.
Extent of fusion
For most CP scoliotic curves, the proximal instrumentation should end fairly high in the thoracic spine, generally around T2, to decrease the risk of proximal junctional kyphosis and pullout of proximal instrumentation. This should also prevent any development of scoliosis above the instrumented level. The caudal extent of the fusion, most notably when to include the sacrum and pelvis, is a topic still under some debate, especially in an ambulatory patient. Several investigators report success fusing only to L5 when the pelvic obliquity is less than 15 degrees and there is some potential for ambulation. Both Whitaker and colleagues and McCall and Hayes used pedicle screws at the most caudal level, and felt that this contributed to the stability of the construct. Even for nonambulatory patients, McCall and Hayes have suggested that sparing the pelvis and maintaining a mobile L5/S1 segment may better absorb trunk movements during wheelchair activities. However, most investigators recommend fusing to the pelvis for curves that have significant pelvic obliquity. Modi and colleagues evaluated postoperative changes in pelvic obliquity in 55 neuromuscular patients with scoliosis with a minimum follow-up of 2 years. Those patients with pelvic obliquity greater than 15 degrees that had fixation to the pelvis had good correction of this obliquity and maintained it at follow-up. However, those with obliquity greater than 15 degrees that did not have pelvic fixation had good initial correction, but progressively lost this correction over time. Tsirikos and colleagues found no alteration in ambulatory status in 24 ambulatory CP patients who underwent fusion to the pelvis, except in one patient who developed severe bilateral hip heterotopic ossification. In general, any patient with significant pelvic obliquity, ambulatory or not, should be fused to the pelvis.
Type of instrumentation
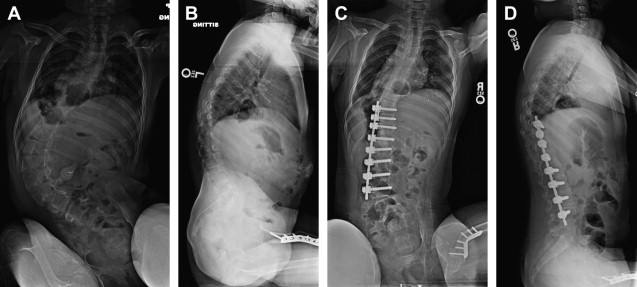
Spinal instrumentation for neuromuscular scoliosis has evolved over the years since the introduction of the Harrington rod in 1962. Due to high pseudoarthrosis rates (11%–40%), modest initial correction (30%–55%), loss of correction over time (8%–28%), and need for prolonged bed rest or casting with Harrington rod instrumentation, segmental spinal instrumentation as developed by Luque in 1976 was quickly adopted as a preferred method to treat scoliosis in neuromuscular patients. Numerous investigators demonstrated improved correction (40%–64%) with lower rates of pseudoarthrosis and decreased need for postoperative immobilization. This was followed with a modification of the Luque-segmental spinal fixation in 1982 by Allen and Ferguson to achieve pelvic fixation. This Galveston method was developed to extend the fusion to the pelvis to better correct pelvic obliquity and overall spinal balance ( Fig. 1 ). Originally requiring intraoperative contouring of two separate Luque rods, the Galveston technique was later modified by Bell and colleagues by developing the unit rod: a single, continuous stainless steel rod with a “U” bend at the rostral end and Galveston-type contouring at the caudal end. Numerous investigators have shown good correction with the unit rod. Bulman and colleagues compared unit rod fixation to Luque rod instrumentation and found improved correction with the unit rod of both scoliosis (62% vs 49%) and pelvic obliquity (79% vs 50%). In one of the largest series, Tsirikos and colleagues retrospectively evaluated 287 children treated with a unit rod; they reported an average Cobb correction rate of 68% and pelvic obliquity correction of 71%, with 96% caregiver satisfaction rate. The U-rod is similar to the unit rod, but it does not extend to the pelvis; instead, it ends in L5 pedicle screws. Extending from its development and use in idiopathic scoliosis, multihook segmental systems such as the Cotrel-Dubousset and Isola instrumentation have also been used in neuromuscular patients, alone or as part of hybrid constructs. Yazici and colleagues evaluated 31 patients and reported scoliotic and pelvic obliquity correction rates of 64% and 82% respectively using Isola instrumentation with Galveston pelvic fixation. They suggested that this construct was the most effective in deformity correction as compared with Luque-Galveston, unit rod, or Cotrel-Dubousset instrumentation.
Recently, pedicle instrumentation has been successfully used for neuromuscular scoliosis. One of the first reports of its use in neuromuscular scoliosis is by Rodgers and colleagues in patients with myelomeningocele. Since that time, there have numerous articles describing its successful use in CP patients. The safety of pedicle screw placement in neuromuscular scoliosis patients using the free-hand technique has been evaluated; Modi and colleagues evaluated 1,009 pedicle screws in 37 consecutive neuromuscular scoliosis patients by CT scan, and found that 93.3% were in the safe zone. In addition, Modi and colleagues published the three-year follow-up data of 52 CP patients who underwent posterior spinal fusion with pedicle screw construct, reporting a 63% scoliosis correction and 56% pelvic obliquity correction. There were 17 major and minor complications in 15 patients; one of these was canal impingement by a screw causing leg weakness and urinary retention, which resolved following screw removal. Watanabe and colleagues compared the radiographic outcomes of curves greater than 100 degrees, of which the majority were neuromuscular, treated at the apical level with either Luque wires, hooks, or pedicle screws. They found that the greatest Cobb correction rate, smallest loss of correction, and greatest amount of apical vertebral translation was in the pedicle screw group.
Similar to the many constructs used to instrument the spine, there are also many methods of addressing pelvic obliquity. The Galveston technique is the most popular and most tested, but iliac and sacral screws, spinopelvic transiliac fixation, and an S-contoured rod that wraps over the sacral ala have also been used. There are advantages and disadvantages to each method but, biomechanically, it appears to be important that the construct crosses a point anterior to the caudal projection of the middle column. Peelle and colleagues compared 20 neuromuscular patients treated with the Galveston method to 20 neuromuscular patients treated with iliac screws and found that there was no difference in Cobb correction, but better pelvic obliquity correction in the iliac screw group. In addition, there were four broken rods and two reoperations in the Galveston group versus one broken screw and no reoperations in the iliac screw group. Sponseller and colleagues, on the other hand, recently compared unit rods with custom bent rods that commonly used iliac screws in 157 CP patients treated for scoliosis. They found improved pelvic obliquity correction with the unit rods, but with higher transfusion requirements and infection rates. In summary, Luque segmental spinal fixation with Galveston pelvic fixation has been successfully used since the 1980s and provides predictable and inexpensive correction, but not without complications. Increased use of pedicle screws has resulted in some improvement in deformity correction. It may also even further decrease the risk of pseudoarthrosis and a loss in correction. There is some controversy, however, whether this justifies the greater financial cost associated with pedicle screws. Currently, a prospective multicenter study is being conducted to evaluate the operative treatment of scoliosis in CP patients. Since various instrument types are included, some of these controversies may be answered.
Role of anterior approach
Traditionally, the inclusion of anterior release and fusion has been to improve flexibility in large, stiff curves and to prevent crankshaft in young patients. To improve curve flexibility and, therefore, correction, anterior release and fusion is usually considered for curves greater than 70 to 100 degrees, or those that do not bend down to 50 to 70 degrees on flexibility radiographs. Significant sagittal deformity and persistent pelvic obliquity on flexibility radiographs are also indications for anterior release. However, the use of pedicle screws with more aggressive posterior-based releases or osteotomies have challenged these indications for an anterior procedure. There have been a few studies suggesting anterior release may not be necessary even in large, stiff curves. Suk and colleagues reviewed 35 patients with curves over 70 degrees treated with posterior pedicle screw instrumentation and fusion only. Thoracic curve correction averaged 66% and lumbar curve correction averaged 59%. They concluded that severe curves of 70 to 105 degrees and greater than 25% flexibility can be successfully treated by posterior spinal fusion without anterior release. They did comment that an anterior release was performed for curves greater than 110 degrees and flexibility less than 20%. Watanabe and colleagues reviewed 68 patients, 44 neuromuscular, with curves greater than 100 degrees treated (at the apical level) with wires, hooks, or pedicle screws. The pedicle screw group had the lowest rate of an anterior procedure with the best rate of correction. The investigators concluded that curves of 100 to 159 degrees can be acceptably and safely treated by posterior-only instrumentation and fusion using pedicle screw constructs. In the only study of exclusively neuromuscular patients, Suh and colleagues reviewed 13 patients with curves greater than 100 degrees treated by posterior-only approach using pedicle screws and posterior multilevel vertebral osteotomies at the apex. The average preoperative Cobb was 118 degrees with only 20% flexibility. The average Cobb correction was 59.4% with 46.1% pelvic obliquity correction. There no neurologic or vascular injuries.
With regard to crankshaft, there is some evidence to suggest that an anterior approach is not always needed in younger patients. Smucker and Miller looked at 50 CP patients with open triradiate cartilages treated with posterior-only spinal fusion with the unit rod. Twenty-nine had a closed triradiate on their most recent films and the mean absolute curve change postoperatively was 0.6 degrees (−9 to14 degrees). They concluded that posterior spinal fusion alone is adequate to control crankshaft in this skeletally immature population. Westerlund and colleagues also found that acceptable curve correction and maintenance of correction can be achieved with posterior-only unit rod instrumentation, even in very skeletally immature patients.
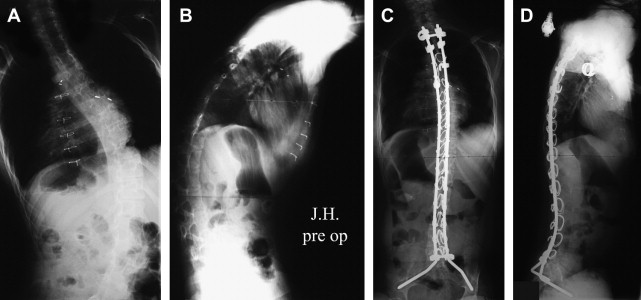
For certain neuromuscular patients (deficient posterior elements, very young patients, ambulatory, nonprogressive curve), some surgeons recommend a selective anterior-only fusion. Although this has not been widely studied in CP patients, the authors routinely perform an anterior instrumentation and fusion to control progressive scoliosis and pelvic obliquity in patients who are too young to undergo a typical T2 to pelvis fusion. This obviates the need for repeated surgeries with methods such as growing rods ( Fig. 2 ). Typically, these patients will require a posterior fusion once they are more skeletally mature.