Management of Soft Tissue Defects Surrounding the Knee and Tibia: The Gastrocnemius Muscle Flap
Steven Myerthall
David J. Jacofsky
Steven L. Moran
Defects surrounding the knee and patellar region are common and may result from trauma, tumor, or infection. One of the most important goals in the management of open wounds surrounding the knee is stable soft tissue coverage. Soft tissue coverage with muscle can seal the joint and bone from ongoing contamination and help to revascularize underlying structures, while preventing the development of late infection and nonunion. Options for soft tissue coverage are determined by the size of the wound, location, and surrounding zone of injury. The gastrocnemius muscle flap has historically been used to cover defects surrounding the knee, lower thigh, and patellar region. Its consistent vascular anatomy and superficial location have made it a workhorse for coverage of defects in this area.
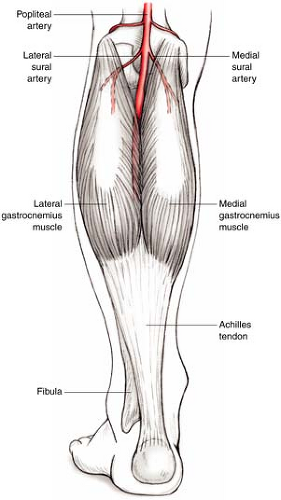
The gastrocnemius is the most superficial muscle of the posterior calf. The muscle has two heads arising from the medial and lateral condyles at the femur, and the adjacent capsule of the knee; these muscles then insert into the calcaneal tendon (Fig. 26-1). The two muscle heads, medial and lateral, unite at the level of the fibular head. Proceeding distally the muscles join with the tendon of the soleus at the mid-leg to form the Achilles tendon. The medial sural artery is the dominant vascular pedicle for the medial gastrocnemius muscle, whereas the lateral sural artery supplies the lateral head. The origin of the arteries is approximately 4 cm above the head of the fibula and both originate from the popliteal artery. Innervation to the muscles originates from the tibial nerve and lies posterior to the vascular pedicle as it enters the muscle.
Indications/Contraindications
Both the medial and lateral gastrocnemius muscles may be used independently or in conjunction with each other. The medial gastrocnemius will cover the inferior thigh, knee, and proximal tibia. The medial head of the muscle is used most frequently as a proximally based flap due to its larger size in comparison to the lateral head of the muscle. The lateral head may also be used alone or in combination with the medial head for coverage of large tibial defects or for lateral distal thigh wounds. For defects at the level of the mid-portion of the tibia, the gastrocnemius muscle may not provide adequate coverage and the soleus muscle is preferred for coverage of middle third defects. For defects involving the distal third of the tibia and ankle, free tissue transfer is usually required. The tendinous inferior margin of the gastrocnemius muscle may be used to augment the repair of an injured suprapatellar tendon.
Contraindications to the use of the gastrocnemius muscle flap include active infection and/or significant disruption of the soft tissue and/or vascular pedicle. Additional contraindications for flap use include any procedure or injury which may have traumatized or injured the sural artery, such as a previous repair of a popliteal arterial laceration or repair of popliteal aneurysm. Occasionally, severe compartment syndromes may render the muscle fibriotic and useable for transfer, but due to its superficial location and high take off of the sural artery, this is unusual. Direct trauma to the posterior calf may result in muscle destruction and should be ruled out prior to proceeding with flap elevation. Radiation to the knee following tumor extirpation may also compromise the vascular pedicle,
increasing the chance of total or partial muscle necrosis following transfer. The muscle should not be used if the soleus and contralateral gastrocnemius muscle are no longer functional, as this will create postoperative difficulty with plantar flexion. A history of a recent deep venous thrombosis within the involved extremity is a relative contraindication for the use of the flap, although we have used the flap successfully in such situations.
increasing the chance of total or partial muscle necrosis following transfer. The muscle should not be used if the soleus and contralateral gastrocnemius muscle are no longer functional, as this will create postoperative difficulty with plantar flexion. A history of a recent deep venous thrombosis within the involved extremity is a relative contraindication for the use of the flap, although we have used the flap successfully in such situations.
Distally based gastrocnemius muscle flaps have been described for coverage of middle third and lower leg defects. Vascular supply to the muscle in these cases is supplied through crossing anastomotic arterial connections between the medial and lateral gastrocnemius muscle bellies extending across the midline raphe. Use of the flap in this manner is not common, as more reliable methods of middle third and lower leg coverage are available and include the soleus muscle flap, the sural artery flap, and free flap coverage.
Preoperative Planning
The preoperative management of severe open fractures involves stabilization of the patient, tetanus prophylaxis, and broad-spectrum antibiotics. Trauma often compromises the availability of the skin and soft tissue surrounding the knee. Nonviable tissue requires aggressive debridement. Serial debridements may be needed if tissue viability is uncertain. Once the wound bed is clean, flap coverage may proceed, ideally within 72 to 96 hours following initial injury. Preoperative physical examination should focus on determining the function of the remaining muscles of the lower leg to determine if sacrifice of the gastrocnemius could result in a significant loss of plantar flexor following muscle transfer. A vascular examination should also be performed to assess for the patency of the popliteal artery. In those patients with a history of peripheral vascular disease or a history of popliteal arterial trauma, an angiogram can confirm patency of the sural artery prior to surgery.
Surgery
Patient Positioning
Operating room setup is standard for lower extremity coverage. A leg tourniquet may facilitate dissection, especially in cases of lateral gastrocnemius harvest where the perineal nerve must be identified and protected during flap elevation.
The muscle may be harvested with the patient in prone or supine position. If the patient is prone, a stockinette or mid-posterior S-shaped incision is made and significantly facilitates exposure of the muscle’s origin posteriorly over the femoral condyle. The posterior approach is made with an incision starting 5 cm above the popliteal crease and extending down to the distal end of the muscle belly. More commonly, however, for anterior traumatic defects surrounding the patellar and tibial region, the patient is positioned in the supine position with the leg internally or externally rotated to facilitate exposure of the medial or lateral heads, respectively. Lateral decubitus positioning is also an option for lateral gastrocnemius muscle elevation.
The patient may receive either general or spinal anesthesia. In additional, depending on associated injuries, the ipsilateral or contralateral thigh should be prepared for a skin graft donor site. After sterile preparation, the entire extremity is draped and fully exposed. Appropriate preoperative antibiotics should be given 30 to 60 minutes prior to incision.
Technique
Medial Gastrocnemius Muscle Flap
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree