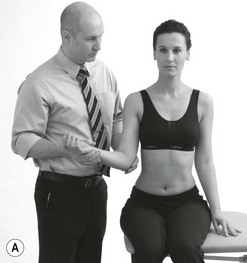
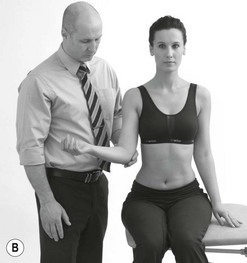
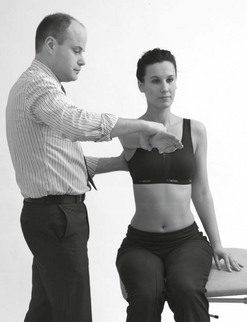
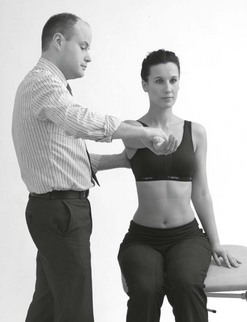
4 A brief introduction to the role of the extended scope physiotherapist Diagnostic considerations – a perspective from the medical profession, an ESP role and the traditional physiotherapy role The diagnosis and diagnostic titles of shoulder conditions Shoulder conditions – a perspective from an ESP role ESP role practice and the diagnostic task The importance of screening for red flags Screening for conditions which require early medical attention Screening for extrinsic sources – analytical assessment and differentiation Shoulder conditions – a physiotherapy perspective Physiotherapy diagnosis and shoulder conditions Physiotherapy diagnosis and shoulder conditions – the American Physical Therapy Association perspective Other developments and considerations in the physiotherapeutic management of shoulder conditions Integration of the Maitland Concept into contemporary physiotherapy practice relating to shoulder conditions This chapter aims to demonstrate how many of the fundamental principles on which Geoffrey Maitland developed his concept are still applicable to contemporary physiotherapy practice both for those physiotherapists performing a traditional role and those undertaking an extended scope role. This discussion will be set within the context of disorders affecting the shoulder complex, repeatedly described as one of the most challenging areas in neuromusculoskeletal practice (Robb et al. 2009ab). The complexity of the shoulder and shoulder girdle combining articulation at the glenohumeral (G/H), acromioclavicular (A/C), sternoclavicular (S/C) and scapulothoracic (S/Th) joints together with the exceptionally large range of functional demands required and placed upon the shoulder complex provides the background to the challenges facing clinicians. The high prevalence of structural pathology in asymptomatic individuals and common occurrence of multiple co-existing structural pathologies further compounds this issue. Although limited to discussion of the shoulder and shoulder girdle, it is hoped that the reader is able to appreciate the applicability of the principles outlined and presented in this chapter to the other body regions affected by neuromusculoskeletal conditions. • The two introductory sections (A brief introduction to the role of the extended scope physiotherapist, and Diagnostic considerations – a perspective from the medical profession, an ESP role and the traditional physiotherapy role) discuss the development of extended scope physiotherapy roles and more specifically address diagnostic considerations as they relate to physiotherapists performing a traditional role and those undertaking an extended scope role. • The third section (Diagnosis and diagnostic titles of shoulder conditions) considers the diagnosis and diagnostic titles of shoulder conditions from a biomedical perspective and discusses the implications for both ESP and traditional physiotherapy practice. • The fourth section (Shoulder conditions – a perspective from an ESP role) and the fifth section (Shoulder conditions – a physiotherapy perspective) discuss the assessment and management of shoulder conditions from the perspective of an ESP and from a traditional physiotherapy role respectively. The United Kingdom’s Chartered Society of Physiotherapy (CSP) defines an ESP as ‘a clinical physiotherapy specialist, in any recognized speciality, with an extended scope role, e.g. requesting X-rays, scans, blood tests, nerve conduction studies etc.’ Traditionally tasks such as these would have been undertaken by the medical profession, but with additional training and development may be performed by physiotherapists with an extended role. In the UK, ESPs practice under the Chartered Society of Physiotherapists’ fourth pillar of practice, ‘kindred methods of treatment’ ( CSP 2008). This is providing that the member is competent in the activity and able to demonstrate that practice is also linked to the curriculum framework and the World Confederation of Physical Therapists’ (WCPT) definition of physiotherapy ( CSP 2008). Within the UK, physiotherapists who are able to demonstrate these requirements are therefore able to perform tasks in extended roles as part of their individual scope of practice and be covered to practice by the CSP’s Professional Liability Insurance ( CSP 2008). Recently, Syme (2009) has developed and published a document on behalf of the ‘Chartered Physiotherapists working as extended scope practitioners’, a clinical interest group of the CSP in the UK, entitled, ‘A resource manual and competencies for extended musculoskeletal physiotherapy roles’ (2009). This document serves as a framework for ESPs to assist individual clinicians in demonstrating their competence to practice specific tasks in extended roles and hence meet the requirements stipulated by the CSP. ESPs working within the musculoskeletal specialty may perform any number of a variety of tasks traditionally undertaken by other professions ( CSP 2008). These tasks vary from those with a therapeutic focus, to those with a diagnostic focus and are dependent upon both the needs of the service in which the individual works and the level to which the individual is educated, trained and competent to undertake the particular task ( CSP 2008). As recognized by Syme (2009) ESPs ‘are not homogenous groups of individuals, even within a specific speciality’. Some of the tasks typically undertaken by an ESP within the musculoskeletal speciality include: • Screening referrals to the orthopaedic speciality. • Undertaking orthopaedic assessments and managing General Practitioner (GP) referrals which previously would have been managed by orthopaedic consultants. • Where appropriate and indicated, referring and interpreting investigations including as examples radiological studies, haematology, clinical biochemisty and electrophysiology. • Referring the patient to a variety of other professionals. As Jette (1989) has discussed, the primary difference in diagnostic classification between the medical profession and the physiotherapy profession relates to the phenomena that are classified as follows: • Medical diagnosis is concerned with ‘the determination of the cause of a patient’s illness or suffering by the combined use of physical examination, patient interview, laboratory tests, review of the patient’s medical records, knowledge of the cause of observed signs and symptoms, and differential elimination of similar possible causes’ (Mosby’s Medical dictionary 2009). • Physiotherapy diagnosis is concerned with classifying the consequences of a patient’s disease, injury or disorder – the impairments, functional limitations and disabilities ( WCPT 2007, Zimny 2004, Jette 1989, Gucione 1991). Figure 4.1 serves to highlight this distinction in the concept of diagnosis between the medical and physiotherapy professions, and sets within this, the position of the ESP which is discussed further in the section ‘Diagnosis and the ESP in the neuromusculoskeletal specialty’. It is pertinent to revisit the position statement relating to the description of physical therapy (physiotherapy) published by the World Confederation of Physical Therapy ( WCPT 2007) in specific regard to both the nature of the physiotherapy and consideration of diagnosis within the profession. Diagnosis is considered by the WCPT (2007) as a professional responsibility of physiotherapists and is described as: As previously discussed in the first section of this chapter, ESPs in the neuromusculoskeletal speciality may perform any number of a variety of tasks traditionally undertaken by other professions ( CSP 2008). A common task undertaken by ESPs is to assume the responsibility for establishing an appropriate medical diagnosis on which decisions regarding a patient’s management and prognosis can be determined and communicated appropriately to other health professionals and the patient. With regard to this requirement, three competencies described by Syme (2009) are particularly relevant and are detailed in Figure 4.1. In contrast to the physiotherapy diagnosis, which seeks to guide decisions regarding the physiotherapeutic management of a patient, the medical diagnosis provided by the physician or the ESP seeks to determine the type of treatment required in the management of the patient. With respect to shoulder conditions, treatment options that are commonly employed include medications including analgesics, NSAIDs and oral steroids ( Green et al. 1998, Buchbinder et al. 2006), corticosteroid injections ( Buchbinder et al. 2003), physiotherapy ( Green et al. 2003), arthrographic distension ( Buchbinder et al. 2008), ultrasound guided barbotage, acupuncture ( Green et al. 2005), topical glyceryl trinitrate ( Cumpston et al. 2009) and a variety of surgical procedures ( Singh et al. 2010, Coghlan et al. 2008, Pulavarti et al. 2009, Tamaoki et al. 2010). A fundamental principle central to the evolution of the Maitland Concept was Maitland’s explicit understanding of the difficulties, limitations and obstructions to patient management should treatment be directed by the medical diagnosis alone ( Maitland 1986). Maitland recognized that ‘even within medicine, many diagnostic titles are sometimes inadequate, incorrect, or they may be merely linked with patterns of symptomatology, they may even be suppositions’. Acknowledgement of the incompleteness and controversies in the theoretical understanding of pathology further added to this contention. Furthermore, using evidence from Macnab (1971), Maitland demonstrated how a single clinical presentation may have several diagnostic titles and conversely how a single diagnostic title may present with several clinical presentations further supporting this opinion ( Maitland 1986 p 6). Maitland advocated that the manipulative physiotherapist should adopt a mode of thinking (two compartment) unique to the Maitland Concept. This has become the symbolic permeable brick wall which lies at the heart of the concept, whereby thoughts regarding the theoretical aspects of a patient’s presentation (known and speculative) are separated from the clinical evidence in the clinician’s mind. Maitland felt that such a mode of thinking ‘prevents thoughts relating to the theory of a disorder overriding the clinician’s decision-making processes and does not inhibit the clinician from discovering the patient’s disorder in terms of its history, its symptoms and its signs in fine detail. It allows for safe and effective management of disorders where there is an incomplete or uncertain diagnosis’. This concept allows the clinician to base intervention primarily on clinical evidence, i.e. ‘the primacy of clinical evidence’, while acknowledging and drawing on evidence from the theoretical compartment for the purpose of hypothesis generation and testing and the choice of treatment technique. Maitland (1986) stated that ‘by basing treatment on symptoms and signs useful treatment may be effected while the medical profession and its scientists continue to work towards understanding more in regard to diagnostic titles’. Beyond the broader concept of ‘shoulder pain’ numerous diagnostic labels have been applied to conditions affecting the shoulder. The derivations of these labels are varied such as ‘painful arc syndrome’, directly labelled from the clinical signs and symptoms, whilst others such as ‘rotator cuff tendonitis’ are derived from hypotheses regarding the pathology producing the clinical signs and symptoms. The pathoanatomical model on which the majority of diagnostic titles are derived seeks to explain the source of the patients presenting symptoms and signs based on the presence of specific structural pathology identified through isolated or combined physical examination, imaging and histopathological analysis. It has been proposed by some authors that identification of a specific structural pathological diagnosis on which clinical decisions regarding patient management can be made is essential to improving treatment outcomes ( Green et al. 1998, Cyriax 1982). In contrast, as discussed, Maitland (1986) viewed the diagnostic or theoretical considerations related to a patient’s presentation secondary in importance to the ‘clinical evidence’ (presenting signs and symptoms) on which the clinician’s decision-making processes are based. The nomenclature used to describe and define shoulder conditions in the international literature is extremely varied, as illustrated in Box 4.1. In 1998, Green et al. demonstrated and confirmed the lack of uniformity in the way shoulder conditions were labelled and defined for the painful shoulder. In a systematic review of 24 randomized controlled trials of interventions which specified a distinct diagnosis to characterize the study sample, only 16 provided definitions of the subgrouping strategy. Furthermore, the selection criteria used to define the shoulder disorders studied demonstrated no between-study standardization and indeed in many cases conflicting criteria were often used to describe the same type of condition in different studies. Ten years on since Green et al.’s (1998) observation and analysis, Schellingerhout et al. (2008) reported that the criteria used to define diagnostic labels for shoulder pain in randomized controlled trials (RCTs) which investigate treatment for shoulder pain with a specific diagnosis continue to fail to demonstrate uniformity. This variability in the criteria used to classify a diagnosis in research is illustrated in Table 4.1. Table 4.1 Criteria used to define a variety of shoulder diagnoses for research purposes In recognition of this lack of uniformity of nomenclature, several attempts at standardizing the use of diagnostic labels using classification systems have been made. Most classification systems have evolved from the pathoanatomical model such as those proposed by Cyriax (1982), Neer (1983), Waris et al. (1979), Viikari-Juntura (1983), Silverstein (1985), McCormack et al. (1990), Uhthoff & Sarkar (1990), ICD-10 ( WHO 2010) and Palmer et al. (2000). Unfortunately, even in the presence of clearly defined operational definitions and criteria for inclusion of a patient to a discrete diagnostic category, studies of the proposed classification systems have demonstrated unsatisfactory levels of inter-rater reliability in all but two papers ( Liesdek et al. 1997, Bamji et al. 1996, de Winter et al. 1999, Walker-Bone et al. 2002, Norregaard et al. 2002, Pellecchia et al. 1996, Palmer et al. 2000, Hayes & Peterson 2003, Hanchard et al. 2005). Other methodological shortcomings of these classification systems have been reported including a failure to be comprehensive and failure of classification categories to be mutually exclusive ( Buchbinder et al. 1996; de Winter et al. 1999). In recognition of these findings the development of a reproducible classification system for shoulder disorders has been considered a research priority by numerous authors, including Kromer et al. (2010), Braun & Hanchard (2010), Kuhn (2010), Mitchell et al. (2005), Green et al. (2008), Schellingerhout et al. (2008), Green et al. (2003) and Buchbinder et al. (2003) to name but a few. Prior to reviewing the current evidence relating to the diagnostic accuracy of tests relating to shoulder conditions it is pertinent to briefly review the concepts and statistical tests associated with diagnostic test accuracy. Six of the most commonly used statistics are detailed in Table 4.2. Table 4.2 Some of the more common statistical concepts associated with defining the accuracy of diagnostic tests Furthermore, when considering diagnostic accuracy studies, bias can significantly inflate the diagnostic value of a test. It is essential that the quality of individual diagnostic accuracy studies in systematic reviews is undertaken and several quality assessment tools have been devised including the QUADAS (Quality Assessment of Diagnostic Accuracy Studies) ( Whiting et al. 2003) and STARD (Standards for the Reporting of Diagnostic Accuracy Studies) ( Bossuyt et al. 2003). Several systematic reviews of shoulder tests, the details of which are provided in following sections, have used such measures of quality. In the evaluation of shoulder pain numerous physical examination orthopaedic special tests have been reported in the literature, which aim to differentially diagnose pathologies of the shoulder. For interested readers, Tennent et al. (2003ab) produced a detailed descriptive two-article review of these ‘special tests’ presenting them as described by the original authors. The diagnostic utility (usefulness) of these orthopaedic special tests has been an area of relatively high publication rate in recent years. In a recent, rigorous systematic review with meta-analysis of individual physical examination tests of the shoulder, Hegedus et al. (2008) critiqued 45 diagnostic accuracy studies. With respect to pathoanatomical diagnoses including impingement, rotator cuff integrity, glenoid labrum or long head of biceps pathology, instability and acromioclavicular pathology, there appear very few orthopaedic special physical tests that are diagnostically discriminatory. These results are supported by findings from other recent systematic reviews of the diagnostic accuracy of physical examination tests of the shoulder, including Beaudreuil et al. (2009), Hughes et al. (2008) and Lewis and Tennent (2007) with respect to rotator cuff pathology, and Dessaur and Magarey (2008), Walton and Sadi (2008), Calvert et al. (2009), Jones and Galluch (2007), Mirkovic et al. (2005) and Munro and Healy (2009) with respect to pathology of the glenoid labrum. As a general feature the tests appear to possess either high sensitivity/low specificity or low sensitivity/high specificity thereby compromising their diagnostic utility. Similar findings were reported with regard to the reliability of these orthopaedic special physical examination tests in a recent systematic review of 36 studies by May et al. (2010). May et al. (2010) concluded that none of the tests reached an acceptable level of reliability. Appraising the overall literature the authors stated that evidence regarding the reliability of these physical examination tests of the shoulder was contradictory ( May et al. 2010). Furthermore, there is apparent poor reproducibility of results between studies and a general trend to suggest that as the methodological quality of the trial improves, the results relating to the diagnostic accuracy of the special orthopaedic physical tests worsens. Numerous methodological shortcomings have been identified with regard to this literature base including small sample sizes, use of inappropriate reference tests and bias. In particular, it is pertinent to note that in the systematic review by Hegedus et al. (2008) only two of the 44 studies included which investigated the diagnostic utility of special orthopaedic physical tests were adequately powered (sufficient sample size) to detect high specificity and sensitivity values. In respect to rotator cuff integrity, no tests demonstrated likelihood ratios to a satisfactory level to modify the post-test probability of diagnosing a rotator cuff tear by a moderate or large amount, thereby questioning their clinical utility ( Hegedus et al. 2008) (see Table 4.2 for a description of statistical terms). At best, based on results from one underpowered and poorly designed study ( Walch et al. 1998), Hornblower’s sign may be diagnostic of ‘severe degeneration or absence of the teres minor muscle’ and the external rotation lag sign diagnostic of an ‘infraspinatus muscle tear’ ( Fig. 4.2). The bear-hug and belly-press tests may assist ruling in a subscapularis tear (specificity 0.98), based on results from a well-designed but underpowered study ( Barth et al. 2006) ( Fig. 4.3). Similar findings were reported by Hughes et al. (2008) in a further systematic review of the diagnostic utility of physical examination tests to detect rotator cuff pathology. Slightly more promising results were reported in a single good quality study undertaken by Park et al. (2005) (QUADAS score 10/14) included in the meta-analysis by Hegedus et al. (2008). Park et al. (2005) used stepwise logistic regression analysis (a statistical method for making predictions of an outcome) and determined that if a patient was more than 65 years of age, and presented with a positive drop-arm sign and tested weak with the ‘infraspinatus test’ or external rotation lag sign ( Fig. 4.4), the likelihood of a rotator cuff tear was >90%, with 28% likelihood of a full thickness tear. Figure 4.2 Hornblower’s sign ( Walch et al. 1998). With the arm in 90° scapular elevation and 90° elbow flexion, add resisted external rotation of the arm. Positive test = an inability to externally rotate the arm. Figure 4.3 Belly press test ( Gerber et al. 1996). In sitting the patient exerts pressure against the abdomen A with or B without the therapist’s hand in between whilst moving the elbow forwards to increase the internal rotation. Positive test = weakness demonstrated by the elbow dropping back. Figure 4.4 External rotation lag sign ( Hertel et al. 1996). A External rotation lag sign – in sitting, the elbow is passively flexed to 90°, and the shoulder is held at 20° scapular elevation and near maximum external rotation. B The patient is then asked to actively maintain the position of external rotation as the therapist releases the wrist while maintaining support of the limb at the elbow. Positive test = when a lag or angular drop occurs. In their systematic review with meta-analysis, Hegedus et al. (2008) considered studies investigating the biomedical diagnostic term of ‘shoulder impingement’ against a reference standard of tissue pathology thought to be associated with the concept including ‘subacromial bursitis or tendonitis’ or a ‘partial rotator cuff tear’ identified at surgery or with the magnetic resonance imaging modality. Unfortunately, meta-analysis was only possible on two tests (Neers and Hawkins–Kennedy, Fig. 4.5) due to a lack of statistical homogeneity (comparing like with like). Results showed that neither test had sufficient diagnostic utility. Based on the results from a single study, Park et al. (2005) report that at best the supraspinatus/empty can ( Fig. 4.6) or infraspinatus tests may help confirm an impression of impingement due to higher specificity values (0.82 and 0.84 respectively). Lower sensitivity values (0.53 and 0.51) questions their clinical usefulness as screening tests. The validity of the use of the identification of tissue pathology as a reference standard for shoulder impingement is open to question given results from studies such as Frost et al. (1999) and Birtane et al. (2001), discussed further in the section ‘Subacromial impingement and imaging’. Figure 4.5 Hawkins–Kennedy test ( Hawkins & Kennedy 1980). Support the arm in 90° elevation with 90° of elbow flexion and forcibly internally rotate the arm. Positive test = pain reproduced in the subacromial space area. Figure 4.6 Empty can test ( Jobe & Jobe 1983). With the arm in 90° scapular elevation and full internal rotation the patient is asked to resist downward pressure. Positive test = pain and/or weakness. Cali Of special orthopaedic physical tests purported to be able to diagnose pathology of the glenoid labrum, individual studies have demonstrated promising results of some physical examination tests, only to be confounded by poor reproducibility of the results by different authors under more stringent conditions. Numerous systematic reviews including those undertaken by Walton and Sadi (2008), Calvert et al. (2009), Mirkovik et al. (2005), Munro and Healy (2009), Hegedus et al. (2008) and Dessaur and Magary (2008) all conclude that at present there are no good single physical examination tests that are able to accurately diagnose the presence or absence of a SLAP (superior labrum anterior posterior) lesion. Some examples are demonstrated in Figures 4.7–4.10. Figure 4.7 O’Brien’s active compression test ( O’Brien et al. 1998). In 90° frontal elevation, 15° horizontal adduction and full internal rotation, resisted elevation is applied. The test is then repeated with the palm fully supinated. Positive test = if deep pain or a click within the glenohumeral joints is elicited during the first manoeuvre, and reduced or eliminated with the second. Figure 4.8 Biceps load I test ( Kim et al. 1999). In supine with the arm in 90° abduction the arm is externally rotated and the forearm supinated. The patient is then asked to flex the elbow while resisting the elbow flexion by the therapist. Positive test = if resisted elbow flexion is pain provocative. Figure 4.9 Biceps load II test ( Kim et al. 2001). In supine with the arm in 120° abduction the arm is externally rotated and the forearm supinated. The patient is then asked to flex the elbow while resisting the elbow flexion by the therapist. Positive test = if resisted elbow flexion is pain provocative. Figure 4.10 Crank test ( Lui et al. 1996). With the arm in elevation and 90° elbow flexion an axial load is applied to the arm while the arm is internally and externally rotated and circumducted. Positive test = pain, catching or clicking. One method used to improve the accuracy of clinical diagnostic physical examination tests is to combine them into clusters. Such an approach has been reported in other body regions with more positive tests increasing the likelihood of the presence of a given disorder ( Laslett et al. 2005, Cook et al. 2010). Results from a single study of such an approach for clinical testing of the glenoid labrum (SLAP), unfortunately has failed to demonstrate any more impressive results ( Guanche & Jones 2003). Positive results from combinations of two or three tests had the effect of only small increases in specificity but consequently reduced the sensitivity values of a single test. Further studies into such an approach are clearly required before any conclusions about the usefulness of combinations of physical tests for identifying SLAP lesions in clinical practice are made. Results from diagnostic accuracy studies investigating the concept of instability appear more promising. Although there was insufficient data to perform meta-analysis, Hegedus et al. (2008) suggest that the apprehension ( Fig. 4.11), relocation ( Fig. 4.12) and anterior release tests ( Fig. 4.13) are useful to diagnose anterior instability, especially when apprehension as opposed to pain is considered as the finding to indicate a positive test. A similar conclusion is reached by Fisher and Dexter (2007). Figure 4.11 Apprehension test ( Rowe & Zarins 1981). In supine passively rotate the arm into maximum external rotation in 90° abduction and apply a posteroanterior force to the humeral head. Positive test = apprehension to the movement with or without pain. Figure 4.12 Relocation test ( Jobe et al. 1989). Repeat the apprehension test with a posterior directed force on the humeral head. Positive test = an increase in the external rotation range before symptom/apprehension reproduction. Figure 4.13 Anterior release test ( Gross & Distefano 1997). Repeat the relocation test and at the limit of external rotation release the posterior directed force. Positive test = a feeling of apprehension with or without a sudden pain. With regard to acromioclavicular joint pathology, again Hegedus et al. (2008) report of insufficient power to undertake meta-analysis. None of the tests studied appeared clinically valuable based on likelihood ratios. Suggestion was made that due to high sensitivity values (0.96) ( Walton et al. 2004), an absence of pain on palpation of the acromioclavicular joint may prove beneficial as an exclusion test of acromioclavicular joint pathology. Results relating to the active compression test, although appearing promising, are confounded by results which indicate worsening of the diagnostic utility of the test as the methodological quality of the studies improve ( Hegedus et al. 2008). Restriction of passive movement of the shoulder, particularly lateral rotation is necessary to assist in the diagnosis of frozen shoulder ( Bunker 2009, Hanchard 2011). A recent review by Hanchard et al. (2011) reported that reliability measuring lateral rotation using visual estimation, reflective of most clinical practice is difficult. Hanchard et al. (2011) cited evidence from studies including those by Croft et al. (1994) who found that visual estimation of external rotation range of movement was poorly reproducible between six experienced rheumatology primary care physicians (ICC 0.43), and Terwee et al. (2005) who demonstrated that a change of 35° or more of lateral rotation was required to establish between tester agreement of two physiotherapists. It must also be recognized that the clinical sign of restriction of shoulder external rotation is not exclusively a feature of frozen shoulder but also of other shoulder conditions (i.e. osteoarthritis). The diagnostic considerations of frozen shoulder and the other conditions described in this section are discussed in the section ‘Summaries of the most common shoulder disorders’. Anatomical basis – Green et al. (2008) sought to review systematically the literature relating to the common clinical tests for the shoulder to establish whether a valid anatomical basis for the test has been established and whether it supported the conceptual theory on which the tests were developed. Of 34 orthopaedic special tests identified in the literature search only six had been studied with respect to anatomical validity, highlighting the dearth of investigation into theory on which the tests were developed. Interestingly, in this review only four orthopaedic special tests (active compression (O’Brien’s test), shoulder quadrant, lift-off test and Hawkins–Kennedy manoeuvre) were identified with a degree of consensus to have a valid anatomical basis. Furthermore, Tucker et al. (2011) in a pilot study on one cadaver investigated the anatomical validity of the Hawkins–Kennedy test. This study failed to demonstrate evidence of supraspinatus compression within the subacromial space, which was the proposed mechanism by the original authors ( Hawkins & Kennedy 1980). In contrast, Tucker et al. (2011) found evidence to suggest that the long head of biceps brachii and the rotator cuff interval, structures which are rarely implicated in impingement syndrome, were compressed. These findings are broadly consistent with the results of Yamamoto et al. (2009) who, in addition, also found the subscapularis tendon to be compressed during the Hawkins–Kennedy test. Face validity – The face validity of orthopaedic special tests which seek to selectively stress individual tendons of the rotator cuff has also been disputed, given the anatomical interdigitation and confluence of the rotator cuff tendons ( Lewis 2009, Burkhart et al. 1993, Clark & Harryman 1992). Pain inhibition – Studies by Ben-Yishey et al. (1994), Steenbrink et al. (2006), Park et al. (2008) and Cordasco et al. (2010) have all demonstrated significant increases in muscle strength around the shoulder complex in subjects with a variety of diagnoses including full thickness rotator cuff tears, partial thickness rotator cuff tears and impingement syndrome following the administration of a subacromial local anaesthetic injection. These findings demonstrate the significant inhibitive effect pain has on the ability to generate muscle force in the shoulder and therefore challenges the face validity of physical examination procedures which purport to implicate the integrity of a specific muscle or tendon through strength testing. Pain source – In a review article, Lewis (2009) acknowledges the evidence which appears to implicate the subacromial bursa as a potential source of shoulder pain. Work from authors such as Gotoh et al. (1998, 2002), Sakai et al. (2001), Voloshin et al. (2005) and Santavirta et al. (1992) have demonstrated a positive correlation between shoulder pain and levels of proinflammatory cytokines and the neuropeptide substance p contained within the subacromial bursa. Naredo et al. (2002) and similarly Lewis (2009) contend that many orthopaedic special tests which purport to differentially assess the rotator cuff tendons, subacromial bursa and subacromial space will lead to mechanical stimulation of the subacromial bursa and hence the nociceptors within. A positive pain response may therefore merely represent stimulation of the subacromial bursa as opposed to the selective structure the test is purported to stress and therefore lead to poor specificity of the examination procedure and inability to make a specific diagnosis. Operational definitions – Hanchard et al. (2011) discuss how unclear operational definitions when assessing shoulder range of movement may affect both the intra-rater and inter-rater reproducibility of results. Considerations such as determination of the end point of range of movement, that is, onset, increase or where pain becomes intolerable, patient positioning during the assessment of range of movement and whether external stabilization of the trunk or scapula is provided are such factors ( Hanchard et al. 2011). A lack of clarity with regard to the specific performance and interpretation of results (operational definitions) of the other physical tests discussed in this section must also be considered. Reference test – As discussed, diagnostic accuracy studies seek to compare a given test against a reference standard. Many of the physical tests reported in the preceding sections have used observed findings at shoulder arthroscopy or imaging findings as the reference standards. As Mohtadi et al. (2004) note, the validity of surgical findings at arthroscopy is yet to be firmly established and additional research is required to determine the accuracy and reliability of findings at arthroscopy. Similar work remains to be undertaken with regard to imaging modalities including MRI and ultrasound. Furthermore, the use of pathoanatomical reference tests may not be the ideal choice as the relationship between pain and tissue pathology in shoulder conditions remains unclear given the high presence of asymptomatic tissue lesions in shoulder investigations. Subacromial impingement as a clinical presentation also fails to possess a gold standard with which to compare physical examination tests. Some of the pertinent issues in respect of the use of imaging are discussed in the section ‘Subacromial impingement and imaging’. The use of a subacromial injection test as a criterion measure is also open to problems as it is reliant on the accuracy of the injection and the anatomical integrity of the subacromial or subdeltoid bursa and the glenohumeral joint. It is evident that at this stage in scientific enquiry, physical examination tests which seek to evaluate the shoulder with regard to identifying pathoanatomical structural diagnosis are abound with uncertainty. In the majority of cases they appear to fail to demonstrate satisfactory diagnostic accuracy and reliability to make a discriminative diagnosis for which the tests were intended. This evidence provides the explanation for the unsatisfactory levels of inter-rater reliability of classification systems proposed based on a pathoanatomical model. Furthermore, the lack of uniformity of diagnostic labels on which management decisions are made is problematic as commonly patients are put into diagnostic groups based on the results of these special orthopaedic tests. There is an obvious need for further methodologically robust studies in the field of diagnostic accuracy of physical examination tests in shoulder conditions given the generally poor quality of the current literature base ( Hegedus et al. 2008, Fisher & Dexter 2007, Beaudreuil et al. 2009, Hughes et al. 2008, Dessaur & Magarey 2008, Mirkovic et al. 2005, Munro & Healy 2009). It is clear, therefore, that clinical decision making regarding the conservative management of an individual with shoulder pain which is based on a clinical diagnosis and use of diagnostic labels arrived at using special orthopaedic tests is flawed. In recognition of these problems, several authors suggest a different model of assessment and treatment be considered, with abandonment of the diagnostic biomedical pathological model in conservative care ( Lewis 2009, Hughes et al. 2008, May 2010, Schellingerhout et al. 2008). In contrast to the biomedical model and perspective of diagnosing tissue pathology to determine management decisions, diagnosis within physiotherapy, which guides the prognosis and intervention strategies for patients, is considered at the level of impairments, functional limitations and abilities or disabilities (World Confederation of Physical Therapy ( WCPT 2007). The requirement for such an impairment-based approach in the management of shoulder conditions is clear when considering the discussion in this and the next section ‘Imaging and the diagnosis of shoulder conditions’. It is interesting to note some of the recommendations in the recent literature with regard to shoulder conditions. Hughes et al. (2008) have stated, ‘perhaps clinicians should be describing signs and symptoms and speculating on pathology rather than trying to localize a specific pathologic structure’. Lewis (2009) proposes a model which helps the ‘clinical decision making process’ with regard to a patient’s conservative treatment based on a patient’s clinical response (symptom modification) to a variety of manual therapy techniques applied to the components of the shoulder complex, cervical and thoracic spine. It is particularly interesting to note how this contemporary stance appears to mirror the contention that Maitland arrived at more than 40 years ago, recognizing the problems associated with diagnosis and diagnostic titles. Maitland’s concept allowed the clinician to base intervention on clinical evidence, i.e. ‘the primacy of clinical evidence’. A quote from Maitland – ‘by basing treatment on symptoms and signs useful treatment may be effected while the medical profession and its scientists continue to work towards understanding more in regard to diagnostic titles’ – appears as valid today as the date when Maitland first developed his concept. A reinterpretation and redefinition of the special orthopaedic tests with respect to the Maitland Concept and their applicability to physiotherapy practice is proposed in the section on orthopaedic special tests on page 223. The presence of abnormal morphology in asymptomatic individuals, anatomical variants which are clinically irrelevant, reporting error, inability of imaging to detect clinically significant pathology and technical factors have all been reported as explanation to signify caution when interpreting findings from radiological investigation ( Khan et al. 1998). Results from a variety of studies suggest that both ultrasonography (USS) and magnetic resonance imaging (MRI) are accurate in the diagnosis of full thickness rotator cuff tears with pooled sensitivity values of 0.95/0.89 and specificity values of 0.96/0.93 respectively, with no statistically significant difference between the two imaging modalities ( Ottenheijm et al. 2010, Shahabpour et al. 2008, de Jesus et al. 2009). For the detection of partial rotator cuff tears, accuracy is much lower. Pooled sensitivity values of 0.72 and specificity values of 0.93 for ultrasound have been reported, indicating that ruling out a partial thickness tear using this modality may be difficult ( Ottenheijm et al. 2010). Similar results have been reported with respect to the ability of MRI to detect partial thickness rotator cuff tears (sensitivity 0.64/specificity 0.92) in a meta-analysis undertaken by de Jesus et al. (2009). Again no statistically significant differences were found between the MRI and USS for the detection of partial thickness rotator cuff tears. Combining MRI with gadolinium enhanced arthrography improves the ability to detect partial rotator cuff tears (sensitivity 0.86/specificity 0.96) ( de Jesus et al. 2009). Important considerations must however be acknowledged when interpreting these findings. Numerous authors have demonstrated the presence of a variety of pathoanatomical features using a variety of imaging modalities in shoulders of asymptomatic individuals. Using magnetic resonance imaging (MRI) Sher et al. (1995) reported an overall prevalence of rotator cuff tears of 34% in 96 asymptomatic individuals. The frequency of tears increased significantly with age, with a prevalence of 54% in those individuals aged over 60 years (28% full thickness, 26% partial thickness tears). In those individuals aged 19–39 none had a full thickness tear and only 4% had a partial thickness tear. Similar findings have been reported by Milgrom et al. (1995), Templehof et al. (1999), Worland et al. (2003) and Yamaguchi et al. (2006) utilizing ultrasonography. In asymptomatic individuals aged over 50, full thickness rotator cuff tears have a reported incidence of 40% ( Worland et al. 2003), and a 50% prevalence of a combination of partial and full thickness tears ( Milgrom et al. 1995). All these studies have reported a high correlation between increasing age and the presence of rotator cuff tears (either partial or full thickness), regarded by some authors as part of the ‘natural ageing process’ ( Worland et al. 2003) or ‘normal degenerative attrition, not necessarily causing pain and functional impairment’ ( Tempelhof et al. 1999). Lewis and Tennant (2007) eloquently conclude ‘there is good evidence that both ultrasound and MRI are accurate at identifying full thickness tears in the rotator cuff and to a lesser extent diagnosing partial thickness tears. However the significance of these findings is open to interpretation as neither of the imaging modalities is capable of detecting a symptomatic tear from a tear not associated with pain or functional loss’. Subacromial impingement syndrome is classically described as an abnormal contact and compression of the rotator cuff, long head of biceps and subacromial bursa within the subacromial space ( Bigliani & Levine 1997, Neer 1983). Current opinion suggests a vast array of possible causes which have been broadly grouped into intrinsic and extrinsic factors and further classified as of either primary or secondary etiology ( Bigliani & Levine 1997) (see Table 4.4). As such, subacromial impingement syndrome encompasses a wide spectrum of possible pathologies with different aetiologies and has been considered by some authors to represent a clinical presentation as opposed to a diagnosis ( Mohtadi et al. 2004). MRI as an imaging modality provides only a static evaluation of the shoulder and as such is only able to provide an indirect suggestion of subacromial impingement based on the presence of pathology thought to be associated with the diagnosis such as subdeltoid or subacromial bursitis, rotator cuff tendinopathy and/or rotator cuff tears ( Bureau et al. 2006; Birtane et al. 2001). Studies by Frost et al. (1999) and Birtane et al. (2001) demonstrate some of the potential problems with MRI and the diagnostic label of subacromial impingement. Lesions of the rotator cuff, especially supraspinatus, are widely believed to be associated with the clinical signs of impingement of the shoulder ( Neer 1983, Iannotti 1991; Tan 1998). In a study of 42 patients with, and 31 age-matched individuals without signs of subacromial impingement (diagnosed clinically), Frost et al. (1999) demonstrated that 55% of subjects in the symptomatic group and 52% of subjects in the asymptomatic group possessed a pathologic supraspinatus tendon. As opposed to being related to the clinical sign of impingement, the pathologic supraspinatus lesions were associated with age. Similar findings were reported by Birtane et al. (2001) who used a physiological standard of reference, namely a subacromial injection of local anaesthetic (lidocaine) to investigate the value of MRI in subacromial impingement syndrome. MRI-based pathologic findings of lesions in the rotator cuff demonstrated a high sensitivity (98.85%) but low specificity (36.84%) in terms of discriminating the subacromial injection test based diagnosis of subacromial impingement syndrome ( Birtane et al. 2001). Although open MRI is able to offer dynamic evaluation, limited availability and restriction of evaluation to single-plane shoulder motion are cited as limiting factors at the current time ( Bureau et al. 2006). Dynamic ultrasonography has also been used to investigate subacromial impingement syndrome, with features such as bunching of the subacromial bursa or pooling of fluid in the subacromial bursa purported to represent the subacromial impingement ( Read & Perko 1998, Bureau et al. 2006, Awerbuch 2008). Unfortunately, the reliability of dynamic ultrasonography is yet to be convincingly demonstrated in the diagnosis of subacromial impingement syndrome ( Read & Perko 1998, Bureau et al. 2006; Awerbuch 2008). Furthermore, although MRI and ultrasonography have been reported to demonstrate high diagnostic accuracy in the identification of the soft tissue lesions associated with the diagnosis of impingement such as rotator cuff tendinopathy and tears and subacromial or subdeltoid bursitis, it must be remembered that these pathoanatomic features possess a high presence in asymptomatic individuals. Radiographic evaluation may provide valuable information regarding the presence of features considered as potential causes of primary subacromial impingement (acromioclavicular osteoarthritis, os acromiale and acromion morphology). However, conflicting results have been reported regarding the relevance of such findings ( Michener et al. 2003, Bigliani & Levine 1997, Lewis & Tennant 2007). Lesions of the subacromial bursa are often considered to be associated with subacromial impingement syndrome and as such a possible source of shoulder pain ( Bigliani & Levine 1997, Neer 1983). Unfortunately, at the present time, there appears to be a lack of standardization when assessing the status of the subacromial or subdeltoid bursa using ultrasonography ( O’Connor et al. 2005, Awerbuch 2008). Furthermore, bursal changes have been reported with high incidence in the asymptomatic individuals in studies such as Naranjo et al. (2002) using ultrasonography and Zanetti et al. (2000) using MRI. van Holsbeeck and Strouse (1993) have demonstrated that abnormal fluid collection within the subacromial bursa may result from communication from the glenohumeral joint in the presence of rotator cuff tear, and therefore has the potential to be as common a finding as asymptomatic rotator cuff tears ( Awerbuch 2008). Furthermore, Svendsen et al. (2004) consider that such bursal changes may be physiological reflecting the protective role of the bursa.
Management of shoulder and shoulder girdle disorders
Introduction
A brief introduction to the role of the extended scope physiotherapist
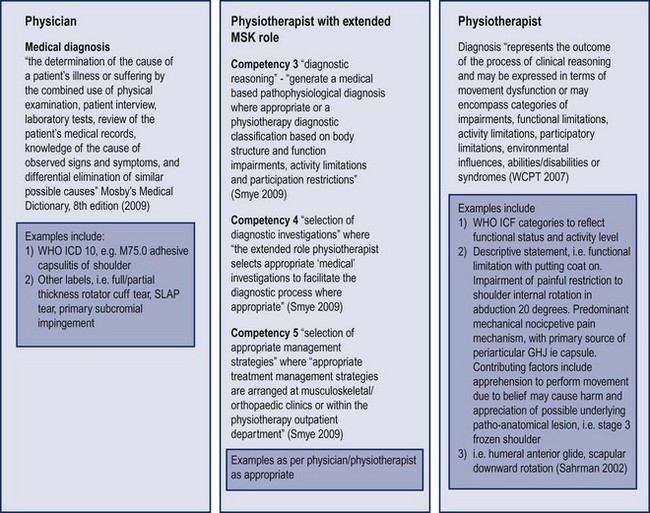
Diagnostic considerations – a perspective from the medical profession, an ESP role and the traditional physiotherapy role
Physiotherapy diagnosis
Diagnosis and the ESP in the neuromusculoskeletal specialty
The diagnosis and diagnostic titles of shoulder conditions
Diagnosis and the Maitland Concept
The biomedical perspective
Diagnostic labels and shoulder conditions
Diagnostic label/concept
Criteria used to define diagnostic label – examples
Shoulder impingement syndrome
More than 30 different inclusion and 40 different exclusion criteria identified across the 16 RCTs reviewed by Kromer et al. (2009)
Only 4 of 15 RCTs (two of which were the same study at a different follow-up periods) which were reviewed by Schellingerhout et al. (2008) used the same combination of inclusion criteria
Adhesive capsulitis/frozen shoulder/painful stiff shoulder
Absence of consistent description of clinical presentation across 21 RCTs reviewed by Schellingerhout et al. (2008). Inconsistency with degree, type (active or passive) and direction of restriction of shoulder movement ( Schellingerhout et al. 2008)
Calcific tendonitis
9/13 RCTs reviewed by Schellingerhout et al. (2008) used the Gartner radiological classification system, with a range of additional inclusion criteria between studies
Rotator cuff tendinopathy/including terms such as rotator cuff tendonitis/tendinosis/supraspinatus tendinitis
In a review of 13 RCTs by Schellingerhout et al. (2008) 5/13 studies failed to report inclusion criteria (physical examination findings), 3/13 studies used Cyriax classification, 3/13 studies’ inclusion criteria included increasing pain with abduction, 2/13 studies used painful arc sign as inclusion factor
Rotator cuff tear
Poor detail of inclusion/exclusion criteria with all 4 RCTs reviewed by Schellingerhout et al. (2008)
Shoulder instability including terms such as voluntary, traumatic, unidirectional, multidirectional, bidirectional
Comparison of four classification methods on 168 patients led to diagnosis of ‘multidirectional instability’ between 1.2% to 8.3% dependent on classification system used; based on result of laxity testing range of diagnosis for MDI was 8.3% to 82.7% ( McFarland et al. 2003)
Kuhn (2010) identified 17 different classification systems of glenohumeral joint instability noting an absence of clear definition, a ‘great amount of discordance’ and ‘different features’ used in the variety of systems reviewed. Kuhn (2010) presented a further classification system
Physical examination related to the differential medical diagnosis of shoulder conditions
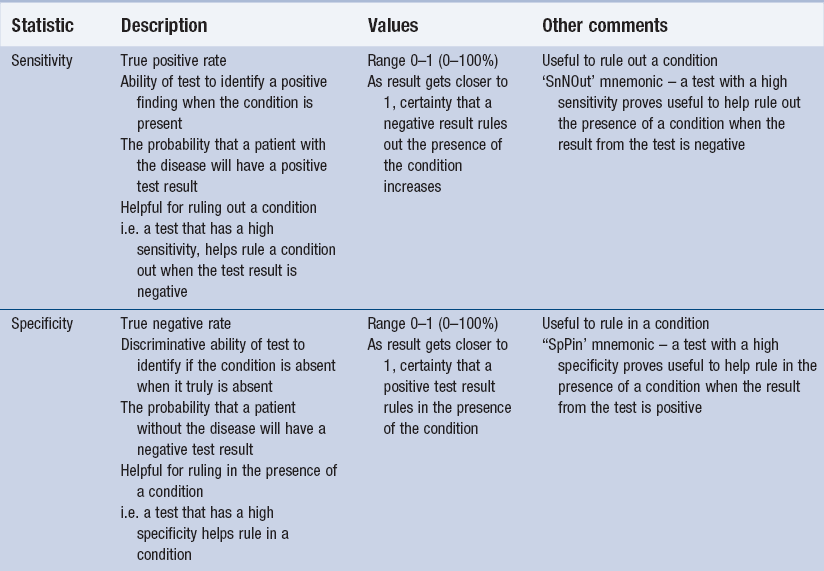
Diagnostic accuracy – a brief review
Diagnostic accuracy of physical tests
Rotator cuff integrity and diagnosis based on physical examination tests



Impingement and diagnosis based on physical examination tests


 et al. (2000) used an alternative reference standard in their study of 120 patients with shoulder pain to identify the presence of ‘subacromial impingement syndrome’, namely the subacromial injection test (SIT). Cali
et al. (2000) used an alternative reference standard in their study of 120 patients with shoulder pain to identify the presence of ‘subacromial impingement syndrome’, namely the subacromial injection test (SIT). Cali et al. (2000) considered a diagnosis of subacromial impingement in patients who reported ‘marked relief of pain and almost total improvement in passive and/or active range-of-movement (ROM) values 30 minutes after injection’ with an absence of calcific lesions identified on radiograph. Results demonstrated that the physical tests either possessed high sensitivity and low specificity (i.e. Hawkins–Kennedy – sensitivity 92.1%, specificity 25%) or low sensitivity and high specificity (i.e. painful arc – sensitivity 32.5%, specificity 80.5%) thereby compromising their diagnostic accuracy and utility. Considerations regarding the SIT as reference test for subacromial impingement syndrome are discussed in the section on ‘Diagnosis of shoulder conditions based on physical examination tests’.
et al. (2000) considered a diagnosis of subacromial impingement in patients who reported ‘marked relief of pain and almost total improvement in passive and/or active range-of-movement (ROM) values 30 minutes after injection’ with an absence of calcific lesions identified on radiograph. Results demonstrated that the physical tests either possessed high sensitivity and low specificity (i.e. Hawkins–Kennedy – sensitivity 92.1%, specificity 25%) or low sensitivity and high specificity (i.e. painful arc – sensitivity 32.5%, specificity 80.5%) thereby compromising their diagnostic accuracy and utility. Considerations regarding the SIT as reference test for subacromial impingement syndrome are discussed in the section on ‘Diagnosis of shoulder conditions based on physical examination tests’.
Glenoid labrum pathology and diagnosis based on physical examination tests




Shoulder instability and diagnosis based on physical examination tests



Acromioclavicular joint conditions and diagnosis based on physical examination tests
Frozen shoulder diagnosis based on physical examination tests
Diagnosis of shoulder conditions based on physical examination tests – an appraisal
Medical diagnosis of shoulder conditions based on physical examination tests – a summary
Imaging and the diagnosis of shoulder conditions
The use of imaging in the diagnosis of shoulder conditions
Rotator cuff integrity and imaging
Subacromial impingement and imaging
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Management of shoulder and shoulder girdle disorders