Chapter 6 Management of Muscle Injury and Myofascial Pain Syndromes
Injury to the muscles of the cervical spine is extremely common from “whiplash” trauma, the most widespread being from motor vehicle collisions. When exposed to rapid stretch, individual muscle fibers may not have sufficient time to relax, resulting in rupture and damage to muscle and fascial structures.1 Injured muscles, when left untreated, significantly prolong healing time and often result in unnecessary disability. The residual of muscle strain is characterized by tender areas known as “trigger points,” readily palpable in the involved muscles.
Historical Overview of Muscle Pain Literature
German Literature
Prior to the 20th century, references to muscle pain syndromes appeared most extensively in the German literature.2 As early as 1843, the German literature referred to tendinous cords or wide bands in muscle as “muskelschwiele” (muscle callus).2 In 1876, Helleday described a myalgic condition characterized by nodules near the origin of muscles that were tender on palpation. The phenomenon of pain spreading from nodules in muscles was also reported by German students of the Dutch masseur Mezger.3
In 1912, Muller discussed fiber hardenings and insertion nodules on palpation of injured muscles. His unique contribution to the early German literature was the identification of insertion nodules, which he described as pressure sensitive. He reported that with pressure, some hardenings radiated pain to far-reaching areas, while others were even spontaneously painful. He noted that these hardenings were predictably found in specific locations in specific muscles.3 Muller pointed out that they were liable to be overlooked because doctors tend not to search for them in a systematic and skillful manner.4 Schmidt, in 1914, implicated muscle spindles as responsible for the painfulness of the muscle hardenings, because of the anatomical location and known sensory function of spindles.2
American Literature
The terms “trigger point” and “myofascial pain” permeate the American literature that describes muscle pain syndromes. As early as 1936, Edeiken and Wolferth5 used the term “trigger zone” to describe pain reported by coronary thrombosis patients referred to the shoulder and down the left arm in response to pressure over the upper part of the left scapula. Steindler,6 in 1940, used the phrase “trigger point” to describe areas from which pain was referred. He described the treatment of chronic pain by injection of trigger points with procaine. In 1942, Travell, with coauthors Ringler and Herman,7 first reported on her many studies on trigger points. Travell’s interest in myofascial pain stemmed from a painful muscle strain that she suffered in the course of her work. She reported in her autobiography that she could touch spots in the muscle that reproduced and intensified the pain that radiated from the trigger area.4 Since that time, Travell has written extensively on this topic, publishing, with Simons in 1983, Myofascial Pain and Dysfunction: The Trigger Point Manual.8 In addition to procaine injections, they described the less invasive treatment of trigger points, recommending stretching of the affected muscles, following topical spraying with vapocoolant. The vapocoolant acts as a distraction while stretching the affected muscle is the desired action.8
Good, who previously published under the names Gutstein and Gutstein-Good, reported in 1950 and 1951 that the patterns of pain referral from tender points in individual muscles are the same in everyone, mapping these in well-executed illustrations.4
Writing in the Journal of the National Chiropractic Association in 1957, Nimmo9 discussed the concept that excessive contraction produced by muscle strain, or other trauma, engages numerous receptors, producing a vicious cycle of noxious impulses. He developed a therapy in which pressure is applied to trigger points to interrupt the pain-spasm-pain cycle. Referred to by Travell and Simons8 as “ischemic compression,” this type of therapy has been widely used by chiropractors in the treatment of muscular trigger points.
Theoretical Models of Muscle and Myofascial Pain
An early model of pain put forward by Descartes postulated that there was a direct line between the peripheral tissues and the brain. He based this on philosophical reflections rather than experimental evidence.10 Von Frey, after correctly identifying pain receptors (“nociceptors”), concluded that the intensity with which pain arising in these structures is felt is in direct proportion to the strength of stimulus applied to them. Goldscheider theorized that the build-up and prolongation of the pain experience, often after a period of time, may be some form of pain-summation mechanism in the spinal cord.10 Livingston,11 in 1943, suggested the possibility of the initiation of activity in closed self-exciting neuronal loops he called “reverberating circuits.” He put aside the long-held view that pain signals pass uninterrupted to the brain and considered the possibility that they may be either augmented or suppressed as they pass through the peripheral and central nervous system. This is supported by the observation that the amount of pain suffered by individuals varies widely and that even seemingly innocuous stimuli may be pain producing.10
Local Response and Muscular Pain
The physical response to painful stimuli is determined by the responsiveness to the nociceptive and modulating system of the individual. Locally, muscle nociceptors take the form of free nerve endings markedly sensitive to chemical stimuli. The degree of pain perception for a given-strength stimulus depends first on the sensitivity of the receptor. Receptors may be sensitized by two different mechanisms, prior stimulation and a variety of chemical agents. These include histamine, prostaglandins, bradykinin, and serotonin.12 The results of their action locally may be not only sensitization of the pain receptors but also local inflammation and hyperirritability of myofascial trigger points. Bradykinin is one of the most potent inflammatory exudates found in damaged tissues. It not only activates nociceptors but also sensitizes them. Serotonin is released from platelet and mast cells as part of the inflammatory response to muscle tissue damage. Both bradykinin and serotonin have a strong vasodilatory effect that leads to the development of edema. It is because of the chemical sensitization of nociceptors that there is a lowering of the pain threshold, making them responsive not only to high intensity noxious stimuli but also to low intensity, mildly noxious or innocuous stimuli.13 In addition bradykinin has the effect of releasing prostaglandins from damaged tissue cells. These in turn have a powerful nociceptor sensitizing effect.10 The sensitization of nociceptors in the damaged muscle makes the myofascial trigger points exquisitely tender, provoking the patient to flinch involuntarily when pressure is applied.
Central Sensitization
Central sensitization can be defined as an exaggerated response of the central nervous system (CNS) to a peripheral stimulus that is normally painful (hyperalgesia) or nonnociceptive, such as touch (allodynia), denoting hyperexcitability and hypersensitivity of the CNS neurons. Characteristic of central sensitization is the persistence of pain.14 It is thought that noxious mechanical and chemical stimulation of nociceptors in the cervical muscles, sensitized by input in their respective fields, shows dramatic expansion of their neuronal activity in the spinal cord. Similar processes were described in the osteopathic literature by Korr,15 and later Patterson and Steinmetz,16 referred to the neurophysiological effect as the “facilitated state.” The reason for the development of secondary hyperalgesia is that the sensory afferent barrage set up by the activated and sensitized trigger point nociceptors causes neurons in the dorsal horn to develop a marked increase in excitability now known as central sensitization.14
The current view of the cellular mechanisms underlying neuroplastic changes indicates that sensitization is caused, at least in part, by changes in the intrinsic characteristics of the spinal neurons involved in addition to changes in the damaged peripheral tissues.17 The process appears to be dependent on an initial activation of nociceptive afferents and the subsequent release of excitatory amino acids and neuropeptides.10,18 Animal studies have demonstrated that the excitatory amino acids, glutamate and aspartate, and neuropeptides, substance P and calcitonin gene-related peptide, for example, trigger a cascade of cellular changes leading to enduring increases in neuronal excitability.19
This increased excitability with the consequent neuroplasticity is thought to lead to central sensitization.17 From other animal studies,20 it is believed that the sensitization of dorsal horn neurons brought about as a result of the sensory afferent barrage, developed in response to the activation and sensitization of nociceptors at the trigger point sites, has the following effects: (a) an increase in the receptive fields of dorsal horn neurons leading to the spread and referral of trigger point pain, (b) the development of secondary hyperalgesia in the zone of the trigger point referred pain, and (c) the perpetuation of dorsal horn neuronal activity, with, as a consequence, the persistence of the pain.10
Referred Pain from Myofascial Trigger Points
Lewis, in 1942, described pain that develops as a result of injury to muscle and perceived by the brain as arising some distance away from the affected site.10 This concept was first put forward in 1909 by Mckenzie and reintroduced by Ruch in 1940.10 The subsequent hypothesis put forward by Mense21 is the assumption that afferent fibers from a muscle’s nociceptors not only make synaptic connections with dorsal horn neurons responsible for conducting nociceptive information from that muscle upward, but also connect with neighboring neurons that normally transmit sensory information from other muscles. It is understood that one-to-one synaptic transmission is the exception rather than the rule in the CNS. A single neuron is acted upon by many other neurons and in turn acts upon multiple neurons. Based on this, it is reasonable to believe that pain originating in myofascial trigger points not only converges and sensitizes the afferent barrage in the dorsal horn neurons primarily responsible for transmitting nociceptive information upward, but also activates and sensitizes dorsal horn neurons that are responsible for transmitting information from distal muscles. The brain, through this mechanism, receives confusing messages and mislocates the pain, perceiving it as originating from a distal muscle and not just the pain-generating trigger point.
Inhibitory Controls
It has been demonstrated that the body produces endogenous pain-suppressing substances that produce analgesic effects in the CNS. These various substances are referred to as “opioid peptides” and include endorphins, dynorphins, and enkephalins.22 These morphine-like substances, which work as inhibitory mechanisms, use both GABA and opioidergic transmitter pharmacologies to suppress nociceptive neuron excitability.17 It is thought that mechanical forces produced by various therapies are of sufficient magnitude to coactivate both low threshold mechanoreceptors and high threshold nociceptive afferents that simultaneously activate antinociceptor systems, suppressing hyperexcitability of myofascial structures. These central antinociceptive mechanisms may operate in conjunction with peripheral antinociceptive mechanisms, particularly when there is inflammation in damaged peripheral tissues.
Pain Patterns from Myofascial Pain Syndromes
Myofascial pain syndromes are characterized by hypersensitive trigger points described as hard, indurated nodules in the muscle, which refer pain in patterns consistent from person to person. Single or multiple trigger points with a twitch response and accompanying taut band are characteristic of muscle exhibiting myofascial pain syndromes.8 Palpation across the muscle fiber reveals the taut band that includes the trigger point, whereas deep palpation along the length of the same muscle fibers gives the impression of a nodule at the trigger point. The local twitch response is seen or felt as a contraction of the fibers in the taut band and lasts as long as 1 second. A sustained burst of electrical activity that resembles motor unit action potentials has been monitored on electromyography (EMG).8
Once established in injured muscles, trigger points may persist for decades, restricting range of motion and recurrently referring pain in characteristic patterns when left untreated. Travell and Simons8 classified trigger points as either active or latent. When referred pain elicited by pressure applied to the trigger point is recognized by the patient as corresponding to his or her clinical complaint, then the trigger point is said to be active. A latent trigger point may persist for years after apparent recovery from injury. The latent trigger points are clinically silent but can become active, with minor overstretching, overuse, or chilling, predisposing to acute attacks. Active trigger points, when left untreated, can become latent and contribute to a poor prognosis or late whiplash syndrome. (See Chapter 11.)
Common Myofascial Pain Patterns from Whiplash Injuries
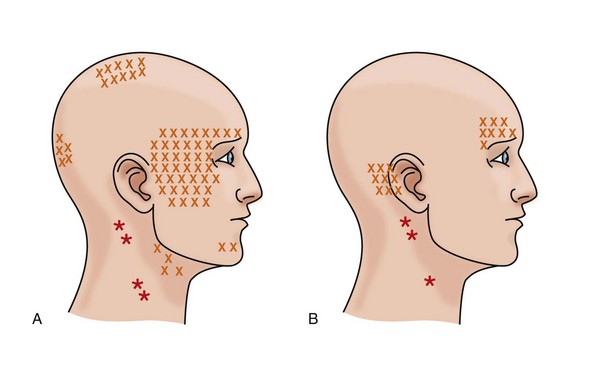
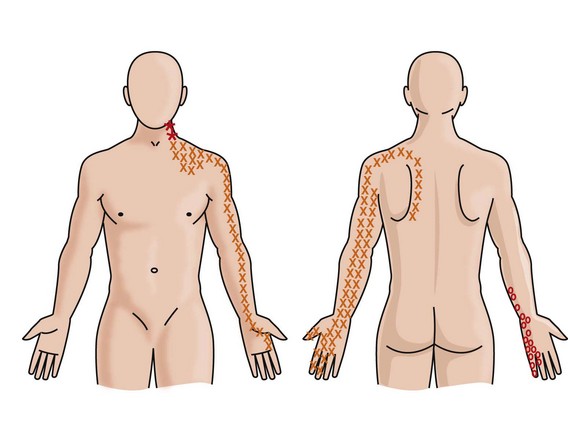
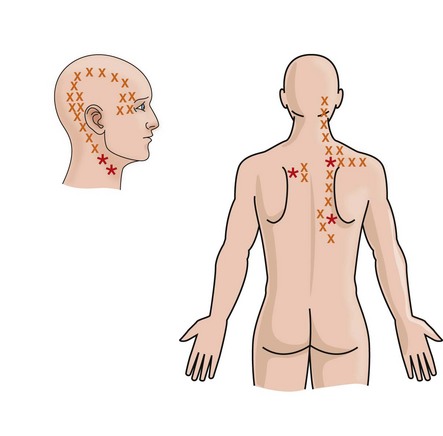
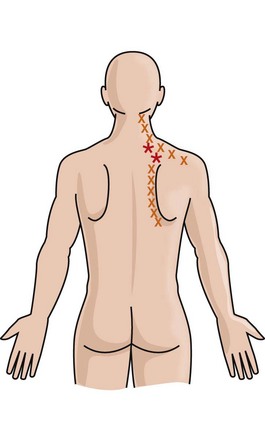
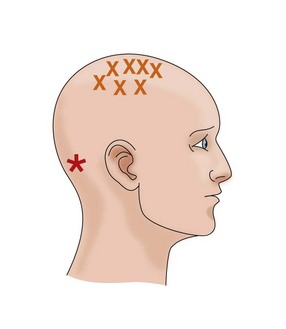
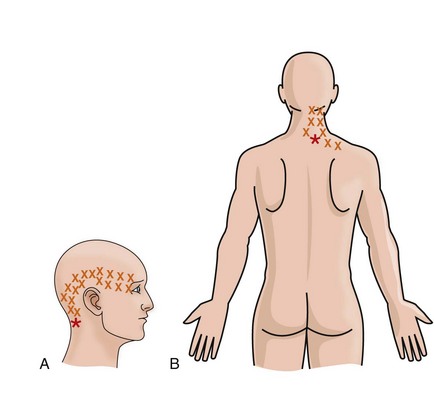
Trigger points in the SCM, in addition to those found in the upper trapezius, temporalis, posterior cervical, and suboccipital muscles, can be the cause of headaches following whiplash injuries. The scalene muscles, on the other hand, commonly refer pain down the upper extremity from entrapment of the lower trunk of the brachial plexus as a result of tautness of the scalene anterior and medius. (See Chapter 8.) This entrapment can cause ulnar pain, tingling, numbness, and dysesthesia. No nerve or vascular entrapment has been recognized as due to trigger points in the levator scapulae, but complaints of neck stiffness following whiplash injury to this muscle is common as both muscles acting together checkrein neck flexion.8 Pain drawings are useful tools that can suggest the location of trigger points and areas of referred pain. Figures 6-1 through 6-24 indicate the location of typical trigger points (*) and areas of referred pain (x).
Sternocleidomastoid (SCM) Muscle
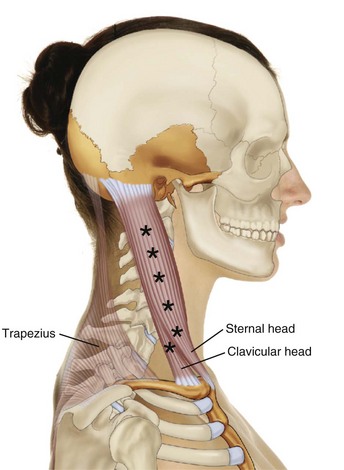
Anatomically, the sternocleidomastoid is a complex muscle with two divisions, the sternal, which is more medial and superficial, and the clavicular, which lies lateral and deeper (Figure 6-1). The muscle is attached above by a short tendon into the lateral surface of the mastoid process and to the lateral half of the superior nuchal line of the occipital bone. Below, the medial or sternal head is attached to the manubrium sterni running obliquely upward, laterally, and backward. The lateral or clavicular head attaches below to the medial third of the superior border of the anterior surface of the clavicle. It passes almost vertically upward behind the sternal head and blends, with its deep surface forming a thick rounded belly.23
The sternocleidomastoid is innervated by the accessory nerve, which arises within the spinal column from the ventral roots of the motor fibers of the upper five cervical segments. The motor nerve fibers ascend through the foramen magnum and then descend through the jugular foramen, where they unite with sensory fibers from the anterior primary division of the second and sometimes third cervical nerves.24
Acting unilaterally, the sternocleidomastoid muscle tilts the head toward the ipsilateral side while rotating the face to the contralateral side. Acting with the upper trapezius, it laterally bends the neck, drawing the ear toward the ipsilateral shoulder. It acts along with the scalene and trapezius muscles to compensate for head tilt due to postural distortion. Acting together, the two muscles draw the chin forward, assisting the longi colli in neck flexion, checking hyperextension of the neck, and resisting forceful backward movement of the head. Acting with the trapezius, the two muscles stabilize the head during talking and chewing. If the head is fixed, they assist in elevating the thorax in forced inspiration. The two muscles are also active when the head is raised while the body is supine.23
Trigger points in the SCM generate complaints of “soreness” of the neck and, most commonly, headaches. Figure 6-2 illustrates the typical site of trigger points and pain referral in the SCM. To palpate the SCM with the patient seated or supine, the neck and head are rotated contralaterally. As the head and neck are lifted, the SCM will visibly contract. The SCM can then be palpated along its length. Trigger points can be palpated when the muscle is slackened by laterally flexing the patient’s head toward the shoulder on the symptomatic side and rotating the face slightly to the contralateral side. Trigger points can then be located by grasping the muscle between the thumb and fingers.
Ischemic compression can be applied to the trigger points exerted by a pincer-like grasp rather than by direct pressure on the trigger point. The clavicular division of the SCM muscle can be stretched by extending the head and neck while rotating the face to the opposite side. To stretch the sternal division, the head is first rotated toward the side of complaint, and at full rotation, the chin is tipped downward toward the shoulder, elevating the occiput and mastoid to provide maximum stretch.8
Scalene Muscles
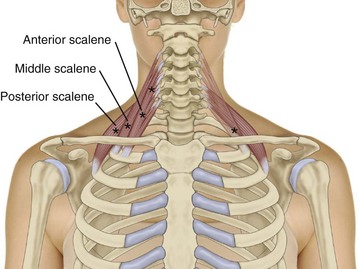
The anterior scalene muscle attaches above to the anterior transverse processes of C3 through C6 and below to the first rib (Figure 6-3). The middle scalene muscle attaches above to the posterior transverse processes of C2 through C7 (occasionally to only C4 and C5). This muscle runs diagonally and attaches below to the cephalad surface of the first rib. (See Figure 6-3.) The posterior scalene muscle attaches above to the posterior transverse processes of the lowest two or three cervical vertebrae and below to the lateral surface of the second and sometimes third rib. It lies deep to the levator scapulae muscle and posterior to the medial scalene muscle. (See Figure 6-3.) Innervation of the scalene muscles is by motor branches of the anterior primary rami of the spinal nerves C2 through C3, corresponding to the segmental level of muscular attachment.
Patients with a history of trauma to the neck should be examined for scalene muscle injury. Muscle strain of the scalene muscles frequently results from hyperextension from whiplash injuries. If the head is turned during impact or is hit from the side, the injury will be unilateral. The characteristic pain pattern referred from trigger points in the scalene muscles extends over the deltoid area, down the front and back of the arm (over the biceps and triceps), and along the radial side of the forearm, thumb, and index finger (Figure 6-4). When it occurs on the left side, it may be mistaken for referred pain from the heart. Posteriorly, the pain may be referred over the upper half of the vertebral border of the scapula and interscapular area. (See Figure 6-4.)
Entrapment of the brachial plexus between the anterior and middle scalene muscles refers pain down the ulnar side of the hand, with numbness due to sensory impairment. (See Figure 6-4.) With swollen and taut scalene muscles, referred pain and entrapment pain may be present along with active trigger points. Motion palpation of the first rib will differentiate costovertebral joint restriction, which should be differentiated.
Examination will reveal restricted lateral bending of the neck to the contralateral side. Placing the ipsilateral forearm across the forehead while raising and pulling the forearm forward lifts the clavicle off the underlying scalene muscles and brachial plexus, may relieve the pain,8 and may be used to differentiate cervical radiculopathy.
Stretching to prevent recurrence can be performed by the patient at home. To stretch the anterior scalene muscle, the head and neck are tilted toward the opposite side, and the head is pressed in a posterolateral direction. To stretch the middle scalene muscle, the head and neck are tilted toward the opposite side and pressed toward the contralateral shoulder. To stretch the posterior scalene muscle, the head and neck are not turned but are pressed in an anterolateral direction along the lines of the muscle fibers.8 Exercises to stretch the scalene muscles can be performed supine if the patient lacks the strength to perform them seated. Resistance exercise to improve strength should not be prescribed before the muscle has been stretched to its optimal length and range of motion restored.
Superficial Muscles of the Neck and Back
Two superficial muscles of the neck and back commonly strained in whiplash accidents are the trapezius and levator scapulae muscles. These muscles are vulnerable to forces produced by whiplash from the side or when the head is turned to one side on impact. The trapezius is the most superficial, with the levator scapulae comprising part of the second layer of back and neck muscles.23
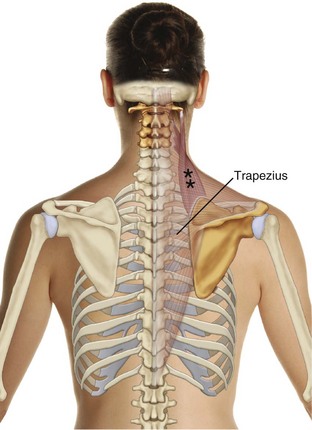
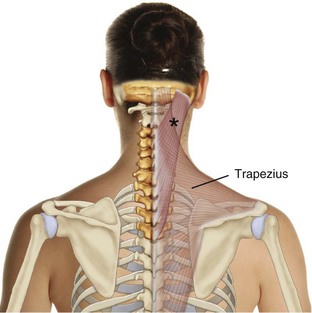
Trapezius Muscle
The trapezius is a tripartite muscle with upper, middle, and lower fibers that often function independently (Figure 6-5). It is a flat, triangular muscle extending over the back of the neck and upper thorax. It is probably the muscle most often beleaguered by trigger points,8 possibly because of its function as a stabilizer of the upper extremities. Once injured, trigger points often become chronic because of the frequent static loading of this muscle.
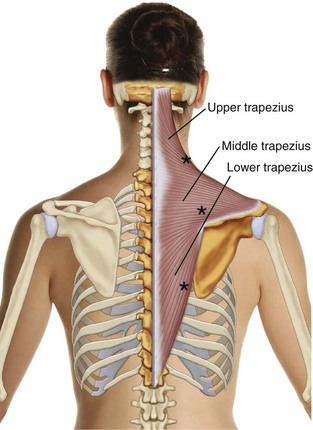
Figure 6-5 Posterior view of the right trapezius. The (*) indicate locations of typical trigger points.
Anatomically, the right and left trapezius muscles form a large trapezium from which they are named. They are attached to the medial one third of the superior nuchal line of the occipital bone, the external occipital protuberance, the ligamentum nuchae, the seventh cervical and all the thoracic spinous processes, and the corresponding supraspinous ligaments. The superior fibers pass downward, attaching to the outer third of the clavicle. The middle fibers attach laterally to the acromion and superior border of the spine of the scapulae. The lower fibers proceed upward, attaching to the tubercle at the medial end of the spine of the scapula, just lateral to the lower attachment of the levator scapulae muscle. (See Figure 6-5.)
Patients with trigger points in the upper fibers of the trapezius muscle complain of pain unilaterally upward along the posterolateral aspect of the neck to the mastoid process (Figure 6-6). These trigger points are a common source of neck ache and temporal headache on the ipsilateral side. Occasionally the pain may be referred to the angle of the jaw with a resultant misdiagnosis of cervical radiculopathy or atypical facial neuralgia.8 Trigger points in the upper fibers of the trapezius are found near the medial end of the spine of the scapula, just lateral to the attachment of the levator scapulae. (See Figure 6-6.)
Trigger points in the lateral lower trapezius fibers can refer pain downward along the vertebral border of the scapula. Those located more medially refer pain upward to the cervical region of the paraspinal muscles, the adjacent mastoid area, and the acromion (Figure 6-7). The lower fibers are strained by prolonged bending and reaching forward while sitting.
To examine for trigger points in the middle and lower fibers of the trapezius, the patient is seated with the arms folded in front of the body to protract the scapula and the trunk slightly flexed to place the muscle on stretch. The patient’s head can then be tractioned to the contralateral side to add further stretch, while deep pressure is applied directly to the trigger points.8 The patient may apply ischemic compression at home by lying on a tennis ball that is positioned to press on tender spots.8 Stretching of the trapezius muscles can be achieved by having the patient bend forward in a seated position.
Levator Scapulae
The levator scapulae are a common site of trigger points that produce complaints of a stiff neck and restricted range of cervical motion. They are frequently strained in whiplash injuries when the head is turned to one side.8 Neck motion is moderately restricted, as the patient tends to look sideways by turning the eyes or body rather than the neck. The head may be tilted slightly to the involved side.
The levator scapulae are attached above by tendinous slips to the transverse processes of the atlas and axis and the posterior tubercles of the transverse process of the third and fourth cervical vertebrae. They descend diagonally to attach below to the medial border of the scapula. They twist so that the C1 digitation is superficial to the others with the fibers vertical. The C4 digitation lies deepest and passes more diagonally to attach to the superior angle of the scapulae.8 Innervation is supplied directly by the third and fourth cervical spinal nerves and by the fifth cervical through the dorsal scapula nerve.
Trigger points develop in the levator scapulae just cephalad to the attachment of the muscle to the superior angle of the scapula and at the angle of the neck where the muscle emerges from the upper fibers of the trapezius. To locate the trigger points, the patient is seated with the neck turned toward the opposite side to stretch and tighten the muscle and to lift it toward the palpating fingers. To locate the lower trigger point, a stroking action back and forth across the muscle may be necessary. These trigger points are exquisitely tender to pressure and refer pain upward to the upper cervical region8 (Figure 6-8).
Intermediate Layers of Muscles that Act on the Posterior Cervical Spine
Both the splenius capitis and the splenius cervicis are susceptible to the trauma of a rear-end collision, especially if the head and neck are somewhat rotated at the time of impact. These muscles are not always protected by the more superficial neck muscles and are often associated with trigger points in the trapezius and levator scapulae, and SCM. Patients with trigger points in the splenius capitus and cervicis often complain of an “ache inside the skull.”8
Splenius Capitus
The splenius capitis attaches to the lower part of the ligamentum nuchae and spinous processes of C7 through C3 or C4 and inserts into the mastoid process, temporal bone, and occiput. The muscle passes upward and laterally under cover of the sternocleidomastoid muscle (Figure 6-9). Bilaterally, the two splenii capitii extend the head. Acting unilaterally, they laterally flex and rotate the face toward the same side.8
Trigger points in the splenius capitus, which overlies the occipital triangle, refers pain to the vertex of the head (Figure 6-10). Splenius capitus trigger points can be located by flat palpation within the upper portion of the muscular triangle bounded by the trapezius behind, the SCM in front, and the levator scapulae below and at the insertion of the muscle on the mastoid process.
Splenius Cervicis
The splenius cervicis originates from the spinous processes of T3-T6 inserting on the transverse processes of C1 through C3 or C4. Acting bilaterally, they extend the neck. When they contract unilaterally, they laterally flex and rotate the face toward the same side. Each is therefore synergistic with the contralateral sternocleidomastoid (Figure 6-11).
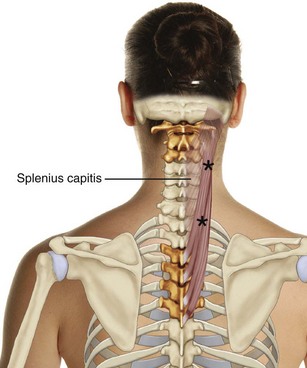
Figure 6-11 Posterior view of the right splenius cervicis. The (*) indicate locations of typical trigger points.
Trigger points in the upper splenius cervicis refer pain to the ipsilateral orbit with the pain seeming to shoot through the inside of the head to the back of the eye8 (Figure 6-12A). The lower splenius cervicis trigger points refer pain to the angle of the neck (Figure 6-12B).
Deep Layers of Muscles That Act on the Posterior Cervical Spine
The deep muscles that act on the posterior cervical spine produce complaints of neck stiffness. If entrapment of the greater occipital nerve is present, there may be complaints of numbness, tingling, and burning pain in the scalp over the ipsilateral occipital region (occipital neuralgia). The deep posterior cervical muscles checkrein neck and head flexion and to a lesser extent contralateral rotation. Caution is advised when needling or injecting these muscles because of the hazard to the vertebral arteries.8
Semispinalis Cervicis
The semispinalis cervicis is a thick mass of muscle that originates from the transverse processes of the upper five or six thoracic vertebrae and may also arise from the articular processes of the lower four cervical vertebrae. It inserts onto the spinous process of the axis and the spinous processes of C3 to C5. The semispinalis cervicis extends the neck and, acting alone, rotates the head to the opposite side.6
Semispinalis Capitis
The semispinalis capitis is a thick powerful muscle that arises from the transverse processes of C7 to T6 and the articular processes of C4 to C6 and inserts onto the occiput. Acting together, the muscles extend the thoracic and cervical portions of the spine. Acting alone, the muscle rotates the vertebral bodies to the opposite side.6 Trigger points in the semispinalis capitis refer pain in a band across the head just above the orbit. Trigger points in the upper splenius cervicis refer pain to the ipsilateral orbit with the pain seeming to shoot through the inside of the head to the back of the eye.8 The lower splenius cervicis trigger points refer pain to the angle of the neck.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree