Management of Major Upper Limb Amputation
Tsu-Min Tsai
Huey Y. Tien
Indications/Contraindications
Replanting the upper limb above wrist level involves a large quantity of muscle and, consequently, is regarded as major replantation. Because muscle does not tolerate anoxia well, the success of arm replantation depends on the effects of ischemia, and warm ischemic time is much more detrimental than cold ischemic time. The tissue damage caused by 1 hour of warm ischemia is equal to that caused by 20 hours of cold ischemia. When warm ischemic time is more than 6 hours, the success rate is markedly decreased and the complication rate is significantly increased. When arm amputation is incomplete, there might be a venous blood regurgitation that causes capillary refill to be present. In this situation, health care personnel may be unaware that the injured limb is devascularized, and therefore fail to keep the injured limb in a cool environment. This oversight further lengthens warm ischemic time and jeopardizes the survival of the injured limb. Furthermore, one should remember that on-table time to revascularization is often warm ischemia time, as well. Daigle and Kleinert reported that the average warm/total ischemia times were 4.8/14.8 hours in failed replantation, which is significantly higher compared with the average of 1.1/7.5 hours in successful replantation.
As a rule, the more proximal the amputation, the poorer the prognosis. Although some debate its efficacy in cases of amputation proximal to the mid forearm, the upper limb should be replanted if at all possible, both for function and cosmesis. However, there are some conditions that contraindicate arm replantation, including:
Significant associated injury
Extensive injury to the affected limb or to the amputated part
Severe medical illness
Significant associated injury to major organs prolongs the patient’s time in surgery and, therefore, increases blood loss and the need for transfusion. Limb replantation is clearly contraindicated if it may jeopardize the life of the patient. Injury factors that require significant consideration are:
Avulsion versus guillotine injury
Ischemia time elapsed
Quantity of tissue loss
Presence of multiple levels of injury
Degree of wound contamination
Chronic illness also may complicate, and even contraindicate, limb replantation. For example, vessel anastomosis may be more difficult among patients with diabetes, who have a higher prevalence of arteriosclerosis. Diabetes, autoimmune disorders, and prolonged steroid use increase patients’ susceptibility to infection. Serious illnesses, including organ failure, preclude replantation surgery.
In addition to severity of injury to the limb and chronic medical illness, one also needs to take patient factors into consideration. Although there is no absolute cut-off age for replantation, the prognosis for a favorable functional outcome decreases with the increase of age. Children, as a rule, tend to be excellent candidates for major upper limb replantation. They have an advantage over adults in tissue regeneration generally, and especially in nerve regeneration. Patient factors in addition to age include the patient’s occupation, hobbies, and wishes.
Preoperative Planning
Of course, always treat any life-threatening associated injury first. As soon as possible, control bleeding on the amputated stump with pressure dressings. Do not use any clamp instrument to try to stop bleeding because this increases the chance of damaging the vital structures (e.g., nerve) next to the bleeding vessels. The cut arterial end, however, can be tied to stop bleeding. Preserve the amputated part in a plastic bag, and cool it in ice slurry to just above freezing, usually 4°C. Then arrange rapid transportation to the replantation center.
In cases of incomplete amputation, wrap the limb snugly with gauze and elastic bandage so that bleeding stops, but not so tightly that blood flow is cut off to healthy tissue. Then, splint the injured area and place a regular ice pack on it. Special attention should be paid for any sign of hypovolemia.
While the patient is prepared for surgery or during transportation, the amputated part can be perfused with organ preservation solution, for example, Tsai’s solution or UW solution, as shown in Table 36-1. Perfusion may have several benefits over simple immersion for large tissue parts, including the physical benefits of more rapidly cooling deep tissues and flushing stagnant blood. If the ischemic time is more than 6 hours, and especially if the amputation is incomplete, the amputated part also can be perfused with 1 unit of heparinized arterial blood obtained from the patient (Fig. 36-1). When the amputated part is brought to the operating room for cleaning and initial debridement, continue to keep it in a cool condition at all times.
Surgery
The patient is taken to the operating room and placed on the operating table in the supine position. Because arm replantation surgery may take as long as 16 to 18 hours, general anesthesia is practically
always required. The patient is given a dose of intravenous antibiotics 30 minutes before surgery. The patient’s injured limb is prepared and draped in standard sterile fashion. An upper-arm tourniquet is inflated to 100 mm Hg above the patient’s systolic pressure to minimize bleeding. If necessary, the contralateral lower limb is also prepared and draped for possible skin, nerve, and/or vein grafting; it may even be used to provide a free flap.
always required. The patient is given a dose of intravenous antibiotics 30 minutes before surgery. The patient’s injured limb is prepared and draped in standard sterile fashion. An upper-arm tourniquet is inflated to 100 mm Hg above the patient’s systolic pressure to minimize bleeding. If necessary, the contralateral lower limb is also prepared and draped for possible skin, nerve, and/or vein grafting; it may even be used to provide a free flap.
Table 36-1. Solutions Used in Arm Replantation | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
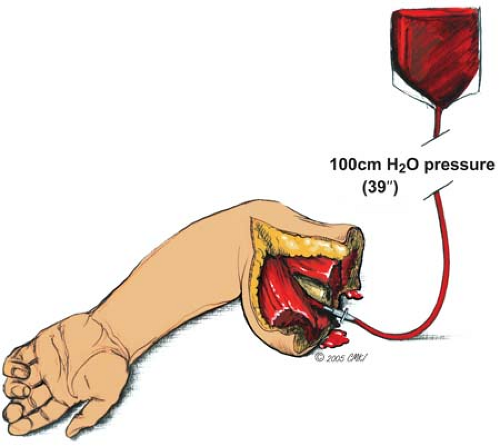 FIGURE 36-1 Perfusion of an amputated limb with heparinized blood. The blood bag is hung 100 cm above the amputated limb and the infusion flows by gravity. |
The order for arm replantation is quite different from finger replantation. Before proceeding with replantation, lactated Ringer’s solution or plasma is used to flush organ preservation solution from the limb. The recommended order of surgical procedures is as follows:
Arterial shunt or perfusion to shorten anoxia time
Thorough debridement
Bone fixation
Artery and vein repair, with or without vein graft
Repair of nerves
Repair of muscle and tendon
Skin grafting or flap for coverage
If indicated, fasciotomy
The artery from the amputated limb is cannulated with a standard vascular shunt to establish the connection between the proximal and distal artery and to intermittently perfuse the devascularized limb. A segment of regular intravenous infusion tube can also be used if no vascular shunt device is available. During perfusion, if the patient becomes hypotensive, temporarily clamp the perfusion. After 20 minutes, the venous shunt can be performed to minimize blood loss.
Thorough debridement is essential for a successful replantation. The injury may occur in an environment such as a farm, an automobile accident, or water sport in which the wound would be severely contaminated. Any crushed, grossly contaminated tissue must be removed. Muscles distal to the amputation level that have lost their contractility must be debrided. Effective debridement converts a dirty, crushed wound to a clean and guillotine-like wound. Residual dead tissue provides a substrate for bacterial growth after major limb replantation. The resulting gas gangrene or septicemia from postoperative infection may be life threatening. In addition, bone infection may result in non-union, delayed functional recovery, and secondary amputation.
Bone shortening is almost always the rule; usually a shortening of at least 2 to 3 cm is required. Bone shortening not only provides more healthy bony structure for an improved chance of bone
healing, but also helps to release tension on the soft tissue and eliminates the need for vein grafting, nerve grafting, or tendon grafting.
healing, but also helps to release tension on the soft tissue and eliminates the need for vein grafting, nerve grafting, or tendon grafting.
Either internal or external bone fixation can be used, depending on the surgeon’s preference. Internal fixation can be chosen for more definitive treatment, especially if there is minimal concern for infection. Plates and screws provide better stability and are most commonly used. Kirschner wires can be used when the amputation is around wrist level. Although intramedullary nailing is an option, it is rarely used. External fixation should be considered when there is a high risk of infection or when internal fixation is contraindicated. External fixation can be used for temporary fracture stabilization until soft tissue is healed. When the limb is viable, internal fixation can be implemented. Occasionally, however, external fixation can be a problem when free tissue transfer is required for soft tissue coverage. If this is the case, external fixation should be switched to internal fixation at the time of the free tissue transfer procedure or should be avoided from the beginning, if at all possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








