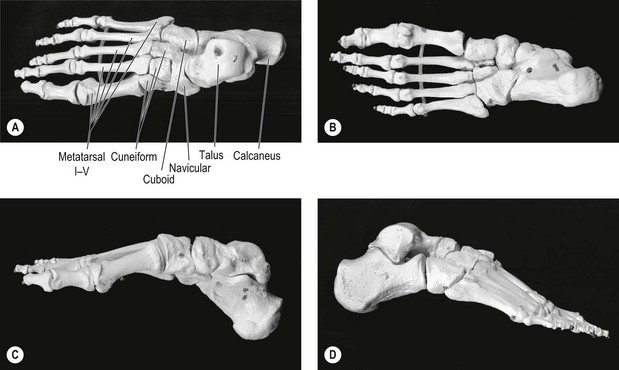
9 Foot and ankle problems are highly prevalent. Population-based studies indicate that between 18 and 63% of people report pain, aching, or stiffness in their feet ( Hill et al. 2008, Menz et al. 2010). Musculoskeletal foot and ankle problems are commonly seen in primary care consisting of 8% of all musculoskeletal consultations ( Menz et al. 2010). The role of manual therapy in the intervention of musculoskeletal foot and ankle disorders is well established ( Bronfort et al. 2010). In contemporary manual therapy practice musculoskeletal foot and ankle disorders should be considered in a multifactorial bio-psychosocial framework ( Kangas et al. 2011). Therefore, the role of manual therapy extends far beyond manual techniques. Manual therapy practice should be a process involving the evaluation of the disorder and implementing an intervention based on evaluation. This process should consider the physical and the psychosocial dimensions of the disorder. The foot consists of 28 irregularly shaped bones, over 30 joints, 32 muscles and over 100 ligaments. All these structures have to work synchronously to fulfill the high requirements of the foot and ankle. The foot alternates in form and function between a flexible structure for shock-absorption during loading response and a rigid lever for propulsion during terminal stance of the gait cycle. Considerable forces act on the foot and ankle during normal daily activities. For example, a joint contact force for the talocrural joint (TCJ) can range from three to five times the body weight during the stance phase of gait ( Kleipool & Blankevoort 2010). The foot can be divided into different regions based on anatomy, arches of the feet, functional regions and for examination and treatment purposes. Anatomically the foot can be divided into hindfoot, midfoot, and forefoot ( Fig. 9.1). The hindfoot consists of the talus and the calcaneus, the midfoot consists of the navicular, cuboid and cuneiform bones and the forefoot consists of the metatarsals (referred to as rays) and phalanges ( Hamill et al. 1995). Classically, the arches of the foot have been defined as medial longitudinal, lateral longitudinal and transverse. From a functional perspective, the arches can be divided into medial, central and lateral ( Fig. 9.2). The medial arch consists of the talus, calcaneus, navicular, medial cuneiform and the first metatarsal bones. The first metatarsal, medial cuneiform and the navicular bones form the first ray. The central arch consists of the intermediate and lateral cuneiforms and the second and the third metatarsal bones. The lateral arch consists of the calcaneus, cuboid and the fourth and the fifth metatarsal bones. The fifth metatarsal and cuboid bones form the fifth ray. Optimal function of the foot and ankle is based on the synchronization of the movements of individual joints. Single-joint movements occur in distinctively different directions ( Nester et al. 2001, Arndt et al. 2004, Tweed et al. 2008). However, in functional movements of the foot and ankle independent movements of single joints are seldom, if impossible. The actions of the joints are highly inter-related and an action at one single joint will influence the other joints. Moreover, movements are often combined or coupled between the joints. For example, in the ankle one-third of the inversion and eversion occurs in TCJ and two-thirds in STJ ( Kleipool & Blankevoort 2010). In this text, the terms eversion and inversion (EV and INV, respectively) are used to describe movements around an anteroposterior axis of the foot. These movements take place in the frontal plane. Plantar flexion and dorsiflexion are used to describe movements around a transverse axis of the foot. These movements take place in the sagittal plane. Abduction and adduction are used to describe movements around a vertical axis of the foot. These movements take place in the transverse plane ( Arndt et al. 2004). The terms pronation and supination (Pron and Sup) are used to describe the triplanar motions of the subtalar joint (STJ) and midtarsal joint (MTJ). These movements are assumed to occur around an axis of the STJ and MTJ ( Nester et al. 2001, Arndt et al. 2004) These definitions are used throughout the text – apart from in the section on techniques. In the section on passive movement techniques, pronation and supination are used to describe the triplanar movement of the whole foot and ankle. The movement of the hindfoot around the vertical axis has been called ‘rotation’. This is to make it easier to separate the hindfoot and forefoot movements. Furthermore, the rotations of the hindfoot are so closely related to the rotations of the lower leg, that it is reasonable to maintain the same terminology in clinical practice. In the section on techniques, the movement directions are defined in Figure 9.4. The distal tibiofibular (syndesmosis) joint is formed by two bones and four ligaments. The distal tibia and fibula form the osseous part of the syndesmosis and are linked by the distal anterior tibiofibular ligament, the distal posterior tibiofibular ligament, the transverse ligament and the interosseous ligament ( Hermans et al. 2010). The main function of the distal tibiofibular syndesmosis is to provide stability for the ankle ( Norkus & Floyd 2001, Hermans et al. 2010). Stability of the distal tibiofibular syndesmosis is necessary for proper functioning of the ankle and lower extremity. Ankle sprain injury may result in widening of the ankle mortise due to increased length of the syndesmotic ligaments ( Hermans et al. 2010). This may be felt in passive mobility examination of the distal tibiofibular joint. During ankle plantar flexion and dorsiflexion, some movement normally occurs at the distal tibiofibular joint. When the foot is moved from a plantar flexed position to a dorsiflexed position, the joint permits approximately 1 to 2 mm of widening at the mortise ( Norkus & Floyd 2001). Movement of the fibula occurs at the distal tibiofibular joint. While in the fibular groove of the tibia, the fibula rotates around its vertical axis when the ankle is plantar flexed and dorsiflexed. Lateral fibular rotation is approximately 3° to 5° with dorsiflexion, and medial rotation is 3° to 5° with plantar flexion ( Norkus & Floyd 2001). The talocrural joint (TCJ) is formed between the articulation of the distal parts of the tibia and fibula with the talus. The TCJ may be considered to have a single axis of movement. When the TCJ is in a neutral position, the axis of the joint passes through the medial malleolus just below the lateral malleolus. Since the lateral malleolus lies more distally, the axis of the TCJ is angled 20°–30° in the frontal plane. Therefore, the dorsiflexion of the TCJ is coupled with abduction and plantar flexion is coupled with adduction ( Hamill et al. 1995). The normal range of motion of the TCJ in dorsiflexion is 20°–30°, and in plantar flexion 40°–50° ( Schuenke et al. 2006). However, there are individual variations: a professional ballet dancer would have difficulty managing with only average mobility, whereas another person with different requirements may have below average mobility without any problems. The subtalar joint (STJ) is located between the talus and the calcaneus, and it has three separate articulations. The axis of rotation of the STJ runs obliquely along the line from the plantar posterolateral surface of the talus to the dorsal anteromedial surface of the talus. The movements of the STJ are pronation and supination ( Hamill et al. 1995). The normal range of motion of the STJ in pronation is 10°, and in supination 20° ( Schuenke et al. 2006). Movements of the TCJ and STJ are partially combined. The maximal range of motion for inversion–eversion occurs at two-thirds of the level of the STJ and at one-third of the level of the TCJ ( Kleipool & Blankevoort 2010). The midtarsal joint (MTJ) is capable of movement in all three cardinal body planes, either in isolation or in combination ( Nester et al. 2001, Tweed et al. 2008). The predominant motion plane of the MTJ varies between subjects; some subjects have a predominance of frontal plane motion, and others have a predominance of transverse plane motion ( Nester et al. 2001). In MTJ, eversion and inversion movements can be coupled in a different manner during the stance phase of gait. Between heel strike and forefoot loading, the MTJ can invert, adduct and dorsiflex, but it everts, abducts and plantar flexes after heel-off. This illustrates the complex and variable functional characteristics of the MTJ ( Nester et al. 2001). During the stance phase of gait, frontal plane movements of the MTJ occur in the opposite direction of the hindfoot ( Tweed et al. 2008). The rays are formed in the longitudinal line of the foot. The tarsometatarsal joints are the main articulation of the rays. These joints are gliding planar joints and are numbered one to five ( Hamill et al. 1995). The intertarsal joint between the medial cuneiform and navicular bones may be included in the first ray. The axes of the first and fifth rays are oblique. In the first ray dorsiflexion is coupled with inversion and adduction, and conversely, plantar flexion is coupled with eversion and abduction. Whereas, in the fifth ray dorsiflexion is coupled with eversion and abduction, and plantar flexion is coupled with inversion and adduction ( Hamill et al. 1995). It is noteworthy, that the first and the fifth rays are the only rays that can be actively supported towards plantar flexion, i.e. on the ground. There are five metatarsophalangeal (MTP) joints. However, the movements of the first MTP joint have a crucial role in the functioning of the foot and ankle. The movements of the first MTP joint are dorsiflexion and plantar flexion. The normal range of motion of the first MTP joint in dorsiflexion is 70°s, and in plantar flexion 45° ( Schuenke et al. 2006). During pre-swing of the gait the first MTP joint is dorsiflexed 55° ( Perry 1992). The motion of the first MTP joint is coupled with the movements of the first ray. Dorsiflexion of the first MTP joint is diminished as the first ray dorsiflexes ( Roukis et al. 1996). This means that the plantar flexion of the first ray is a prerequisite for the dorsiflexion of the first MTP joint in closed kinetic chain. This phenomenon is easy to prove in a clinical setting. Normally in the standing position dorsiflexion of the first MTP joint will result in plantar flexion of the first ray and rising of the longitudinal arch. Whereas if plantar flexion of the first ray does not occur it will limit the dorsiflexion of the first MTP joint. The dorsiflexion of the MTP joints is related to an important function called the ‘windlass’ mechanism. This mechanism provides stability of the foot during propulsion and contributes to the efficient transfer of force during propulsion ( Herrmann 1995). Plantar heel pain is a common disorder which is estimated to affect 10% of the general population at some time during their life ( Crawford & Thomson 2003). The exact etiology of plantar fasciitis is unknown in most cases. However, multiple risk factors have been associated with plantar fasciitis, particularly obesity, prolonged weight bearing, and limited ankle dorsiflexion ( De Vera Barredo et al. 2007). Plantar fasciitis affects the hindfoot, specifically the insertion of the plantar aponeurosis at the medial calcaneal tubercle ( De Vera Barredo et al. 2007). In some cases, pain under the heel is diagnosed as a heel spur syndrome or plantar heel pain syndrome. Heel spur syndrome refers to the existence of plantar calcaneal spur. However, 50–55% of patients with heel pain do not have a calcaneal spur and 15–20% of non-painful heels manifest a spur ( Irving et al. 2006, De Vera Barredo et al. 2007). Therefore, the presence of structural pathology (i.e. calcaneal spur) does not correlate necessarily with pain. Plantar heel pain syndrome is, as indicated by its name, a general definition for the location of pain, but it does not specify the structure of pain origin. Several different structures can be a source of pain under the heel. The plantar surface of the calcaneus serves as an insertion for several structures. Structures connected directly to the medial calcaneal tubercle, lateral calcaneal tubercle or adjacent to these tubercles include: short plantar ligament, long plantar ligament, plantar aponeurosis, m. flexor digitorum brevis (FDB), m. abductor halluces (AbdH), m. quadratus plantae (QP) and m. abductor digiti minimi (AbdDM) ( Acland 2010). Therefore, diagnosing plantar heel pain every time as plantar fasciitis is a simplification and can often misdirects the treatment. Identifying the specific source of the pain might be challenging and even in a case where it can be identified it does not explain the mechanism leading to pain. Considering the structures in the heel it is reasonable to argue that very different movement patterns of the foot and ankle may cause overloading and sensitization to one of these structures leading to plantar heel pain. For example, constant flexion of the toes during weight bearing can potentially cause irritation of FDB, QP, and AbdH muscle insertions. Constant loading of the lateral arch during weight bearing can potentially lead to overloading of short and long plantar ligaments and AbdDM muscle. Constant medial loading of the foot during weight bearing collapses the longitudinal arches of the foot potentially leading to overstretching of the plantar aponeurosis. All these loading patterns of the foot may become a mechanism resulting in plantar heel pain. Therefore, identifying the movement patterns of the foot and ankle that can potentially lead to overloading and sensitization of the structures is essential when planning and implementing the intervention. Obviously, all the above mentioned examples require different interventions. In addition to symptomatic structures interventions should target the underlying mechanisms that lead to or maintain the plantar heel pain. Ankle ligament injuries are among the most common musculoskeletal injuries ( Pijnenburg et al. 2000, Beynnon et al. 2001, Kerkhoffs et al. 2007). Functional treatment has been recommended for the treatment of ankle ligament injuries since the early nineties ( Kannus & Renström 1991, Kaikkonen et al. 1996). The elements of functional treatment include: RICE (rest, ice, compression, elevation), protection of the injured ligament, early weight bearing and exercises ( Kaikkonen et al. 1996, Konradsen et al. 2002, van Rijn et al. 2010). However, despite functional treatment residual symptoms and disability are very common after inversion sprain ( Konradsen et al. 2002, van Rijn et al. 2010). After an acute ankle sprain 10–20% of people develop chronic ankle instability (CAI) ( de Vries et al. 2006). Two primary causes for CAI are mechanical ankle instability (MAI) and functional ankle instability (FAI) ( Hubbard et al. 2007). MAI is defined as ankle movement beyond the physiological limit of the ankle’s range of motion, whereas FAI is defined as the subjective feeling of ankle instability (‘giving way’) and/or recurrent symptomatic ankle sprains ( Tropp 2002). It is noteworthy that MAI means objectively measurable movement of the ankle and FAI is a person’s subjective symptoms and disability. MAI and FAI are often seen as dichotomous causes of chronic ankle instability. However, recent research has found relationships between MAI and FAI measures. For example, increased anterior laxity correlated with increased dorsiflexion strength and increased centre-of-pressure excursions ( Hubbard et al. 2007). Instability as a term refers to increased mobility. By definition, this is true in MAI when the physiological range of movement is tested passively. Objective assessment of mechanical ligamentous laxity is often carried out using the anterior drawer test and talar tilt test ( Hubbard et al. 2008). However, increased mechanical laxity in passive movement testing does not correlate with the functional mobility of the ankle. Similarly, in FAI the subjective feeling of instability, i.e. ‘giving way’, does not mean that functional mobility of the ankle is increased. Based on clinical evidence, patients with CAI often have movement impairments of the ankle. This feature of CAI is often missed. Contrarily to increased mobility, reduced ankle dorsiflexion range is known to predict future lateral ankle sprains ( de Noronha et al. 2006), whereas generalized joint hypermobility does not increase risk of injury in the ankle region ( Pacey et al. 2010). Pain is a common symptom related to ankle instability ( Kannus & Renström 1991, Konradsen et al. 2002, de Noronha et al. 2007). Pain areas vary a lot after initial ankle injury and the pain area may change over time. The different pain areas are often related to the variety of structures that might be involved in inversion sprains, whereas the change of pain area is thought to indicate multi-tissue involvement ( Konradsen et al. 2002). The change of pain area over time may also be related to the person’s behaviour as caused by the injury. After initial injury people adopt, either consciously or instinctively, movement patterns to avoid pain. These movement patterns can be considered protective, that is, an adaptive mechanism to support healing process. However, if these movement patterns persist beyond normal tissue healing time they may become pain provocative, that is, maladaptive mechanisms, and result in ongoing pain. Depending on the movement pattern the person has adopted, different areas of the foot and ankle are predisposed to abnormal loading. This might be one explanation for the change of pain area over time after an ankle sprain. In acute injury, the escape from a harmful situation and the associated withdrawal behaviour promotes healing. In some individuals immediate withdrawal behaviours do not lead to the anticipated reduction of pain, which may be interpreted as a signal of continuous threat. Negative interpretation may not always reflect the real threat and catastrophic misinterpretations of benign physical sensations may occur. Catastrophic interpretations lead to fear reactions. Pain-related fear is likely to cause a cascade of psychological and physical events including hyper-vigilance, muscular reactivity, avoidance and guarding behaviours and physical disuse, which in turn are responsible for the persistencee of the pain problem ( Vlaeyen & Linton 2002). Pain-related fear of movement, or kinesiophobia, has been shown to contribute to disability in foot and ankle patients ( Lentz et al. 2010). Many foot and ankle pain disorders do not fit into existing medical diagnosis categories and, in many cases, even where pathoanatomical diagnosis can be made it does not explain the mechanism leading to the disorder. Examples given earlier in this chapter highlight the need to consider the multifactorial nature of musculoskeletal foot and ankle disorders. Chronic musculoskeletal disorders are particularly challenging as specific diagnosis is rarely achieved. The tendency for pain and disability to persist in the absence of obvious, ongoing primary peripheral pathology is challenging ( Zusman 2002). Therefore, further classification of chronic foot and ankle disorders is required. A new classification system for chronic musculoskeletal foot and ankle disorders has been proposed ( Kangas et al. 2011). This new approach is based on identifying the underlying mechanisms of the disorder. Within a multifactorial bio-psychosocial model, all factors that are maintaining the disorder should be considered. Without the identification of these mechanisms, the optimal intervention for the patient’s disorder cannot be determined ( Zusman 2002). Chronic pain disorders may change motor control around the foot and ankle region and appear to result in monotonic movement and loading patterns, with specific parts of the foot and ankle loading unchangingly. Typically, these loading patterns present in a directional manner and are relatively independent of the movement task or activity the patient is performing ( Kangas et al. 2011). Identifying the direction of impairment is the basis for identifying the mechanisms involved in movement and motor control-related disorders of the foot and ankle region and for planning and implementing a specific intervention ( Kangas et al. 2011). Maladaptive motor control and movement impairments are considered underlying mechanisms for chronic foot and ankle disorders. Within these impairments, faulty movement patterns and coping strategies result in chronic abnormal tissue loading, pain, disability and distress. Different underlying pain mechanisms of motor control and movement impairments require further subclassification. These impairments can present with or without pathoanatomical findings ( O’Sullivan 2005). In motor control impairments, lack of motor control results in monotonic loading patterns and pain in the foot and ankle. In movement impairments, movement is lost in the direction of pain provocation. In patients with motor control and/or movement impairments, the patient’s maladaptive movement behaviour is the underlying mechanism for the pain. An analysis of all potential factors affecting this movement behaviour should be based on a comprehensive subjective and physical examination and should aim to identify the underlying mechanisms maintaining the chronic foot and ankle disorders. Identifying this underlying mechanism also demands the integration of the proposed classification approach for foot and ankle disorders within a clinical reasoning process ( Kangas et al. 2011). The inclusion of psychosocial factors in the conceptual framework of pain theory helps to explain the limited association between organic pathology and pain severity ( Turk & Wilson 2010). Avoidance behaviour may be reinforcing in the short term through the reduction of distress associated with noxious stimulation. If allowed to persist, it may become a maladaptive response leading to increased fear, limitation of activity, and other physical and psychological consequences that contribute to disability and persistence of pain ( Turk & Wilson 2010). Catastrophic interpretations such as the belief that the presence of, or onset of, pain indicates pathology and therefore harm, are thought to contribute to the development of pain-related fear ( Turk & Wilson 2010). A theoretical approach to the development of chronic pain and disability is the fear–avoidance model. This model is an attempt to highlight the importance of cognitive and behavioural factors in a chain of events linking the experience of pain to disability. The model stresses the role of catastrophic thinking following the pain experience and the consequent fear and hyper-vigilance. Avoidance behaviour features prominently, largely fuelled by the fear that activity will cause harm and will worsen the pain problem ( Boersma & Linton 2006). Fear–avoidance beliefs, catastrophizing, and depression have been identified as important psychological variables in the development of a pain problem ( Boersma & Linton 2006). The relationship between pain, catastrophizing, depression, fear–avoidance beliefs and function at the individual level is an integrated, interacting, and complex process ( Boersma & Linton 2006). Psychological variables might operate differently for different people. Therefore, to understand these processes within individuals, there has been a need to identify distinctive patterns of psychological factors ( Boersma & Linton 2006). A study by Boersma & Linton (2006) shows that distinct profiles of psychological functioning can be extracted and that these profiles are related to development of disability. Fear–avoidance, beliefs and catastrophizing were strongly related. These factors can be, but are not necessarily, accompanied with signs of depression. People in the subgroups ‘pain-related fear’, ‘pain-related fear + depressed mood’, and ‘depressed mood’ reported substantially more functional difficulties and pain and sick leave compared to ‘medium pain-related fear’ and ‘low risk’ subgroups. Pain processing is regulated by different mechanisms that modulate noxious information at the spinal level. This modulation is based on endogenous descending inhibitory and facilitatory pathways that reach the dorsal horn ( Weissman-Fogel et al. 2008). It has been proved that these inhibitory pathways are negatively influenced by catastrophizing ( Weissman-Fogel et al. 2008). Growing evidence is showing that psychological processes have biological effects. For example, cognitive and affective processes within the construct of catastrophizing have been shown to exert an effect on the neuromuscular, cardiovascular, immune and neuroendocrine systems, and the activity in the pain neuromatrix within the brain ( Campbell & Edwards 2009). Studies have shown that higher levels of pain catastrophizing correlate with a lower pain threshold, lower pain tolerance, higher pain intensity and greater pain temporal summation ( Weissman-Fogel et al. 2008). Pain-related fear of movement has been identified as a strong contributor to disability in the foot and ankle ( Lentz et al. 2010). The risk factors and consequences of traumatic and non-traumatic lower limb pain are not the same. Traumatic lower limb pain is associated with practising vigorous exercise and a high level of physical fitness, while non-traumatic pain is correlated more with psychosomatic symptoms ( El-Metwally et al. 2006). Greater numbers of depressive symptoms have been found to associate with greater impairment in lower extremity functioning ( McDermott et al. 2003). Lifestyle factors, such as obesity, have been related to foot and ankle pain disorders ( Irving et al. 2006, Gaida et al. 2010). There is evidence of an association between increased body mass index and chronic plantar heel pain ( Irving et al. 2006). Achilles tendon pathology is associated with central fat distribution among men and with peripheral fat distribution among women ( Gaida et al. 2010). Jobs that necessitate prolonged standing and walking activities are commonly associated with worker’s complaints of foot and ankle pain. The foot and ankle area has been identified as the most frequently affected body region among salespersons in department stores ( Pensri et al. 2010). Prolonged standing is associated with foot and ankle symptoms among salespersons ( Pensri et al. 2010). Furthermore, prolonged standing has been associated with the occurrence of chronic plantar heel pain ( Irving et al. 2006). Increased time spent walking is associated with foot and ankle disorders among assembly plant workers ( Werner et al. 2010). The patient’s story may reflect that psychosocial factors are contributing to their foot and ankle disorder. The role of these factors is individual. Therefore, it is reasonable to use standardized questionnaires to screen these factors. For example, the Örebro musculoskeletal pain questionnaire (ÖMPQ) can be used for screening for ‘yellow flags’. The Tampa scale of kinesiophobia (TSK) has been used to determine the influence of pain-related fear of movement on foot and ankle disability ( Lentz et al. 2010). However, the neurogenic symptoms vary greatly depending on the local structure involved and the disorder. The symptoms differ depending on the pathophysiology related to the nerves. Radiculopathy, conduction block of the spinal nerve or its root, results in numbness or weakness. Radiculopathy alone does not cause pain. In radicular pain that arises as a result of irritation of the spinal nerve or its roots, pain is shooting and band-like. Radicular pain may occur with or without radiculopathy ( Bogduk 1997). In a neuropathy, symptoms related to sensory innervation include sensory loss, dysaesthesia and/or paraesthesia. Dysaesthesia includes symptoms like burning, pricking, tingling, cramping and throbbing. The most typical presentation of paraestheasia is spontaneous tingling that is often described as pins and needles. It is important to realize that numbness and increased sensitivity may be at the same site. The neuropathic process involving motor nerves will result in muscle wasting and weakness ( Bennett 2006). Foot and ankle symptoms relating to radicular pain or neuropathy are often spontaneous and/or variable, but independent from foot and ankle loading. The main question in behaviour of the symptom is: what makes the symptoms worse and/or better? The main questions at this stageare: when and how did the symptoms start? The onset of radicular foot and ankle pain is often associated with the onset of low back pain and related movement impairment. The most common cause of radicular pain is disc herniation ( Bogduk 1997). Therefore, the progression of radicular foot and ankle pain often follows the course of low back pathology and associated symptoms. The main question at this stage of the subjective examination is: how has the patient managed with the problem since it started? With this question the therapist aims to identify the strategies the patient has used to cope since the beginning of the disorder. This stage should particularly focus on the psychological process involved in pain perception and behaviour and the attention and attributes the patient gives to noxious stimuli, coping strategies and behaviour ( Linton 2002). This information is crucial to understanding the patient’s behaviour according to the disorder and for determining if the patient’s coping strategies will promote healing and recovery or reinforce the disorder. These questions are for the screening of possible precautions and contraindications relating to physical examination and treatment. Questions concerning the patient’s general health, medication, diagnosed diseases and medical screenings should be asked routinely. With the foot and ankle ankle region particular care should be taken, for example, with diabetic patients. Sensorimotor neuropathy and vascular insufficiency may predispose to infections in the diabetic foot ( Powlson & Coll 2010). 3. Neurophysiological pain mechanisms 4. Direction of the impairment 7. Precautions and contraindications The nature of the musculoskeletal foot and ankle disorder is multifactorial. The term disorder contains the physical and psychosocial factors related to disorder and their effects ( Elvey & O’Sullivan 2004). For example, inversion sprain of the ankle may result in the rupture of the anterior talofibular ligament (ATFL). This represents the pathology of the disorder. The physical effect of this is that the patient cannot do plantar flexion of the ankle because of the pain. Injury and resulting pain is always accompanied by psychosocial factors. Pain is psychologically processed and it will influence the patient’s behaviour. These effects are considered as psychological effects. Impairments of movement are consequences of physical and psychosocial factors related to the disorder. For an impairment of movement to be relevant it has to be in the context of the nature of the disorder. All these pain mechanisms require a different approach in the examination and treatment of the disorder. Pain mechanisms are explained in detail in Jones (2014), Blake & Beames (2014). This hypotheses category aims to clearly define the direction of impaired movement in the disorder. For an impairment of movement to be relevant it should present in the direction of the pain. Movement may be lost or movement or loading increased in a specific direction. The direction of the impairment may be related to physical or psychological effects of the disorder. For example, after an acute inversion sprain the direction of the impairment correlates with structural pathology related to injury, whereas, in more chronic disorders the direction of the impairment is related to loading patterns of the foot and ankle. Both motor control and movement impairments of the foot and ankle present in a directional manner ( Kangas et al. 2011). Intervention is a term used to embrace manual therapy procedures of treatment and strategies of management. Treatment is regarded as specific intervention performed by the clinician. Management is intervention performed by the patient under the direction or by the prescription of the clinician ( Elvey & O’Sullivan 2004). Within this hypotheses category, hypotheses are generated relating to the need for treatment procedures and management strategies. For example, in motor control impairments of the foot and ankle, management strategies (i.e. exercise intervention) is the primary approach, whereas with movement impairments restoring normal physiological range of movement of the foot and ankle often requires specific treatment (i.e. mobilization or manipulation) before exercise intervention is initiated. Within this hypotheses category, hypotheses are generated in two directions. The first direction considers the possible need for cautious examination and/or a need for immediate referral to medical care in thecase of serious pathology, i.e. a ‘Red Flag’. The second direction considers the indication for manual therapy intervention and whether a manual therapy intervention has the ability to favourably influence a disorder towards recovery ( Elvey & O’Sullivan 2004). For example, in tibialis posterior tendon insufficiency therapeutic exercise may be helpful if the tendon is not ruptured, but in the case of tendon rupture surgery is warranted.
Management of foot and ankle disorders
Introduction
Anatomy and regions of the foot and ankle
Movements of the foot and ankle
Axes and planes of movements
Movements of the single joints
Distal tibiofibular joint (syndesmosis)
Talocrural joint
Subtalar joint
Midtarsal joint
Rays
The first metatarsophalangeal joint
Musculoskeletal foot and ankle disorders
Typical medical diagnoses of the foot and ankle
Plantar fasciitis
Diagnosing plantar heel pain
Chronic ankle instability
Chronic ankle instability and mobility of the ankle
Chronic ankle instability and pain
Cognitive processes and injury
Chronic musculoskeletal foot and ankle disorders
Psychosocial factors of pain and disability
Psychosocial factors and neurophysiological pain mechanisms
Psychosocial factors and musculoskeletal foot and ankle disorders
Lifestyle factors and musculoskeletal foot and ankle disorders
Work-related factors and musculoskeletal foot and ankle disorders
Subjective examination
Symptom area(s)
Behaviour of the symptom(s)
History of the symptoms
History of the patient’s behaviour according to the disorder
Medical screening questions
Planning the physical examination
Expressing hypotheses categories
Nature of the disorder
Neurophysiological pain mechanisms
Direction of the impairment
Intervention
Precautions and contraindications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine