Chapter 27 Management of Acute Knee Dislocation before Surgical Intervention
CLASSIFICATION
A patient with two or more torn major ligaments may have sustained a knee dislocation.54 This definition accounts not only for those knees that are dislocated at the time of evaluation but also for those that have spontaneously reduced. Clinically, the degree of ligament disruption can be misleading. Because ligaments can stretch and may not appear completely disrupted, especially on MRI, the severity of these injuries can be easily underestimated.
The following variables are the basis for classification and complete description of a dislocated knee: (1) direction of dislocation, (2) open or closed, (3) high- or low-energy trauma, and (4) time from dislocation.16 Schenck50 has also recommended that the extent of ligamentous injury be included in the classification of knee dislocations (see Chapter 26, Classification of Knee Dislocations).
The direction of dislocation may be unidimensional (anterior, posterior, medial, or lateral) or a rotatory combination. If the knee has spontaneously reduced, classification is based on direction of instability.46 Anterior dislocations caused by hyperextension of the knee are the most common, occurring in 40% according to Green and Allen’s review17 of 245 knee dislocations. Posterior dislocations, often caused by high-energy dashboard mechanisms, accounted for 33% of the cases. Medial and lateral dislocations were present in 18% and 4% of the cases, respectively.
In 1963, Kennedy’s biomechanical study26 in cadavers elucidated the mechanisms for both anterior and posterior dislocations. This investigation demonstrated that by progressively hyperextending the knee, the posterior capsule ruptured followed by the PCL and the ACL. Without adequate ligamentous restraint, the knee dislocated in an anterior direction. A high posteriorly directed force on the proximal tibia in knee flexion caused a posterior dislocation.
Posterolateral dislocations are the most common type of rotatory dislocations. The flexed and non–weight-bearing knee undergoes a sudden rotatory moment that abducts and internally rotates the lower leg on the femur.44 This causes the medial femoral condyle to “buttonhole” through the anteromedial capsule, which may be irreducible. Inspection of the knee will reveal a transverse groove in the skin along the medial joint line secondary to invagination of the medial capsule. This “dimple sign” becomes more prominent with attempted reduction and is pathognomonic of the irreducible posterolateral dislocation.16,38,45,48,49
Open dislocations of the knee are emergencies that require antibiotics and urgent irrigation and débridement in the operating room. Open injuries, present in 19% to 35% of knee dislocations, are most commonly seen with anterior and posterior mechanisms.36,55
VASCULAR INJURIES
Arterial trauma associated with knee dislocations represents limb-threatening injuries. The incidence of popliteal artery disruption during a knee dislocation is 32% to 45%.17,24 Delay in diagnosis longer than 6 to 8 hours is associated with an increasing amputation rate.17,24 Because of the high rate of injury and the devastating consequences associated with a delay in diagnosis, it is imperative to recognize vascular injuries early. An abnormal vascular examination should prompt an immediate vascular surgery consultation.
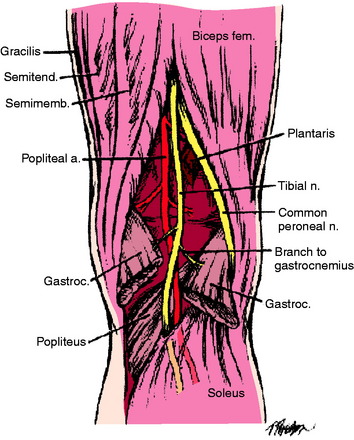
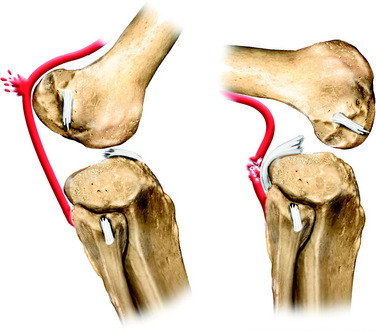
The popliteal artery is at risk of injury during a knee dislocation owing to its anatomic location (Fig. 27-1). The popliteal artery is tethered proximally by the adductor hiatus and distally by the soleus arch. The artery bifurcates into the anterior and posterior branches at the soleus arch. Collateral circulation in the form of the genicular arteries originates within the popliteal fossa. The geniculate arterial system is usually not sufficient to perfuse the limb should there be obstruction or transection of the popliteal artery.16,40 Anterior dislocations of the knee can place significant traction on the popliteal artery, leading to extensive intimal injury and/or vasospasm (Fig. 27-2).17 Posterior dislocations can result in complete transection of the artery (Fig. 27-3).41

FIGURE 27-2 Angiogram demonstrates diffuse irregularity in the popliteal artery with intimal dissection.
Critical Points VASCULAR INJURIES
The diagnosis of a vascular injury should be made on the assimilation of a variety of clinical and diagnostic tests including physical examination, ankle/brachial index (ABI), and arteriography. The dorsalis pedis arterial pulse is palpated on dorsum of the foot, and the posterior tibial arterial pulse is palpable posterior to the medial malleolus. The presence of these pulses with a warm foot is not a guarantee that an arterial injury is not present. There are multiple reports of vascular occlusion or intimal tears with normal distal pulses; the incidence is reported to be 5% to 15%.1,24,33,61 In 2004, Barnes and coworkers4 performed a meta-analysis that included 284 multiligamentous knee injuries in seven studies. Seven of 52 patients requiring vascular surgery had normal pulses on presentation. Thirteen of 140 patients with normal pulses who underwent arteriography had nonocclusive intimal defects that were safely observed. Abnormal pulses had a sensitivity rate of 0.79 (95% confidence interval [CI], 0.64–0.89), specificity rate of 0.91 (95% CI, 0.78–0.96), positive predictive value of 0.75 (95% CI, 0.61–0.83), and a negative predictive value of 0.93 (95% CI, 0.85–0.96). The low sensitivity and specificity may be associated with hypotension in the acutely traumatized patient, as well as intimal lesions that may initially present with normal pulses.
The ABI is the second diagnostic tool to be used. ABIs are determined by measuring the systolic blood pressure for all four extremities using a Doppler probe and a standardized blood pressure cuff. For the lower extremity, the systolic pressure is measured at the posterior tibial and dorsalis pedis arteries. ABI is then calculated by dividing the highest measured pressure in the ankle or foot by the higher of the brachial arterial pressures. An ABI of less than 0.90 is considered abnormal and should prompt arteriography. In 2004, Mills and associates37 demonstrated that 11 of 11 patients with ABIs less than 0.90 required a reverse saphenous vein graft for popliteal artery injury (3 popliteal artery transections, 6 popliteal artery occlusions, 1 common femoral and peroneal artery thrombosis, and 1 high-grade superficial femoral artery occlusion with intimal flap altering popliteal artery flow). None of the 27 patients with ABIs greater than 0.90 had evidence of vascular injury by serial examination or duplex ultrasonography. The sensitivity and specificity was 100%. In 1998, Cole and colleagues8 evaluated 70 consecutive patients with blunt trauma and found no arterial injury with ABI greater than 0.90, whereas an ABI lower than 0.90 had a positive predictive value of 88%. Lynch and Johansen31 studied blunt and penetrating trauma in 100 consecutive patients and found an ABI less than 0.90 predicted vascular surgery with a sensitivity of 87%, specificity of 97%, and positive predictive value of 91%.
Arteriography, developed in the 1960s, has improved outcomes and reduced the number of negative explorations. Many authors have advocated routine use of arteriography to evaluate the limb after a suspected knee dislocation.1,9,17,25,26,30,32,33,67 The routine use of arteriograms for suspected knee dislocations is justified by the relative low morbidity of the test, the high incidence of popliteal injury, and the devastating consequences of a delay in diagnosis.46 However, clinicians should be aware that not all arterial trauma is detectable with arteriography. Stretch injuries of the intimal wall and small intimal flap tears may not be visualized on the arteriogram, but may subsequently clot and result in arterial occlusion. Those patients who worsen usually do so within the first 3 months, but more commonly, within a week after injury. McDonough and Wojtys34 reported on three patients with normal initial arteriograms. Two patients who had loss of pulse after tourniquet release during ligament reconstruction were found to have chronic intimal flaps with thrombi at immediate revascularization. One patient developed a pseudoaneurysm, which was recognized by a second arteriorgram after there was significant postoperative swelling.34
Arteriograms can be performed in the operating room if there are obviously diminished pulses or if the delay in obtaining a formal arteriogram in the angiography suite would compromise limb survival. Six to 8 hours of warm ischemic time will significantly compromise a lower extremity.17 Formal angiography is performed with a femoral artery puncture followed by insertion of a pigtail catheter. Next, a bolus of contrast is injected and an angiographic unit is used to capture images. The length of the segment to be imaged determines the number of acquisitions needed. Intraoperative arteriogram can be performed by injecting 45 mL of contrast through an 18-gauge catheter with a single film exposure35 or a vascular fluoroscopic unit.
Unfortunately, arteriography is not without risks, costs, and false-negative results. The complication rate has been reported to be 1.7% and includes thrombosis, arteriovenous fistulae, bleeding, renal failure, reaction to contrast material, and pseudoaneurysm formation.3,27,37,61,66 The reported false-positive results have ranged from 2.4% to 7%, which could lead to unnecessary surgical intervention.3,58,61,66 The cost of the arteriograms ranged from $750 to $1,500 per study in 1990; a more recent figure was $5,240 in 2003.3,58,61
In addition to formal angiography, new techniques such as computed tomographic angiography (CTA) and magnetic resonance angiography (MRA) are being developed. These techniques make use of readily available imaging techniques often with a bolus of contrast to define the lower extremity arterial system. Potter and coworkers43 demonstrated 100% correlation between conventional angiography and MRA in a small cohort of patients (six patients: four normal, one intimal tear, one decreased flow).
NEUROLOGIC INJURIES
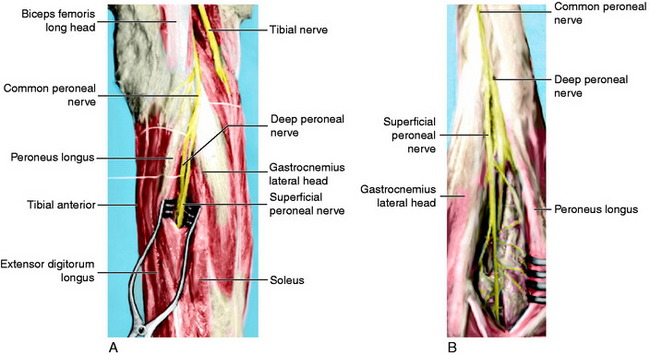
Neurologic damage occurs in 16% to 40% of knee dislocations.2,57 This may range from a stretch injury (neurapraxia) to a complete transection (neurotmesis). The peroneal nerve is most commonly injured as it is stretched over the fibular neck during a posterolateral dislocation (Fig. 27-4).14,47,60,62,67 A common presentation for peroneal nerve injuries is a patient with a drop foot and sensory deficit over the dorsum of the foot. Tibial nerve injury associated with a popliteal artery injury has also been reported.67 Although difficult, a complete neurologic examination of both lower extremities should be performed both before and after any attempt at reducing a knee dislocation. Repeated examinations are recommended during the course of treatment because there is a potential for nerve compromise due to soft tissue swelling and compartment syndrome, pressure, immobilization, and/or positioning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree