Malunited Calcaneal Fracture: Calcaneal Osteotomy Arthrodesis and Subtalar Distraction Arthrodesis
Michael M. Romash
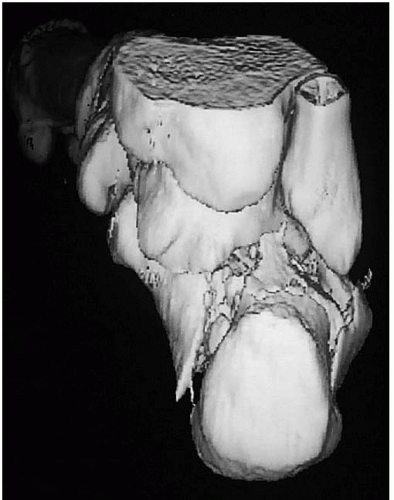
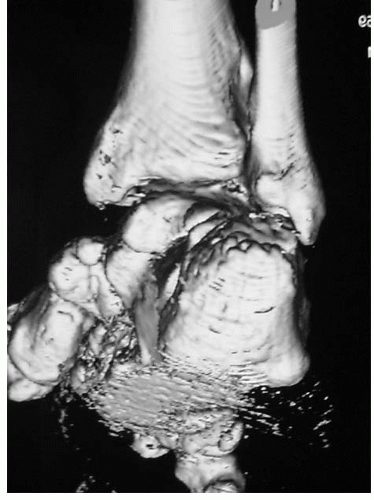
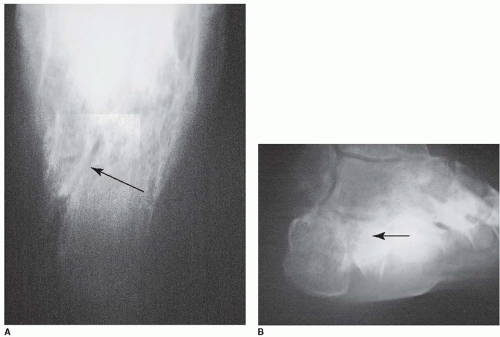
The symptoms caused by a malunited calcaneal fracture are predictable once the deformity and joint injury resulting from the fracture pattern are understood (1,2). The shear force that occurs through the calcaneus due to the noncollinear alignment of the laterally positioned tuberosity to the body of the talus marks the line of the oblique primary fracture line that runs from superior lateral to inferior medial and anterior lateral to posterior medial (Fig. 23.1). This splits the posterior facet (and sometimes splits the anterior facet). The tuberosity shifts lateral, proximal, and into varus (Fig. 23.2). As the lateral side of the posterior facet is driven into the talus, it is depressed into the body of the calcaneus and causes outward bulging of the lateral wall of the calcaneus. The calcaneus loses height and widens (Fig. 23.3).
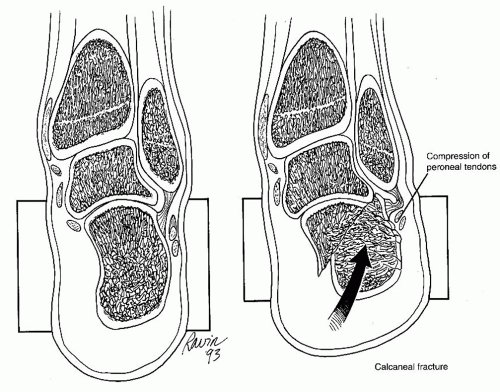
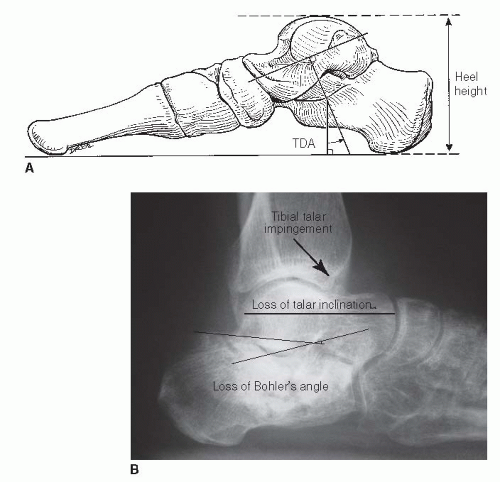
The resultant deformity of these fragments if the fracture heals in situ will cause a variety of symptoms (1,3). The lateral displacement of the tuberosity and lateral wall causes displacement of the peroneal tendons, sural nerve irritation, and fibulocalcaneal impingement (Figs. 23.4 and 23.5). The irregularity of the subtalar joint causes posttraumatic subtalar arthritis (Fig. 23.6). The loss of height causes talar dorsiflexion and can cause anterior tibial talar impingement (Fig. 23.7). The abnormal three-dimensional spatial relationships of the subtalar complex joints as well as the subtalar arthritis causes hindfoot stiffness.
The physical exam will show a wide flattened foot, hindfoot stiffness, and loss of the sulcus between the fibula and calcaneus. The treatment of the malunion can be tailored to the magnitude of the deformity and the symptoms produced. Sanders described a system grading the calcaneal fracture malunion deformities (4).
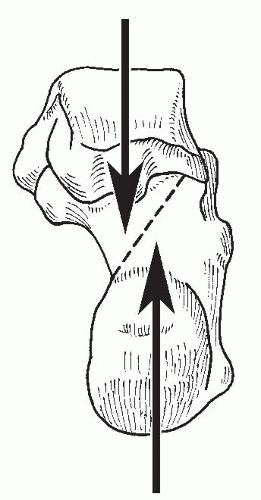 FIGURE 23.1 Drawing of calcaneus from posterior view shows shear force on calcaneus with resultant fracture. |
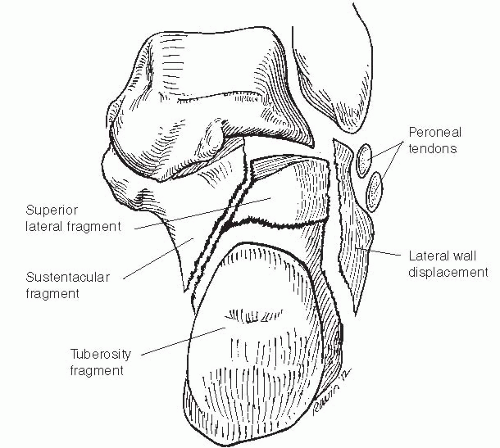 FIGURE 23.2 Drawing shows calcaneal fracture displacement with calcaneofibular impingement and compression of peroneal tendons. |
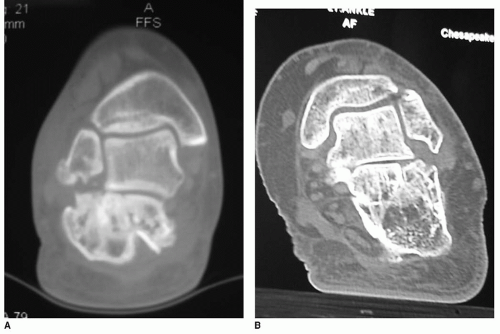 FIGURE 23.6 A: CT scan in coronal view shows malunion, posttraumatic arthritis, and lateral displacement. B: CT scan shows posttraumatic arthritis and lateral displacement. |
INDICATIONS AND CONTRAINDICATIONS
This procedure is indicated for malunions with posttraumatic subtalar arthritis, lateral fibulocalcaneal impingement, displacement of the peroneal tendons, and sural nerve irritation (2,5, 6, 7 and 8).
The loss of height should not exceed 15 mm, as correction greater than this is not obtainable.
The vascular status should be secure.
Relative contraindications include vascular disease, diabetes mellitus, tobacco use, and infection.
Adequate bone stock is needed.
As stated above, a loss of height greater than 15 mm cannot be addressed adequately by this procedure.
PREOPERATIVE PLANNING
A computed tomography (CT) scan with three-dimensional volumetric reconstruction will provide the best blueprint plan for the procedure (Fig. 23.8) (9). Other radiographs include axial heel view, Broden view, anteroposterior (AP) foot view to image the calcaneocuboid joint (Fig. 23.9), and weight-bearing lateral view (see Fig. 23.7B). A weight-bearing lateral view of the uninjured foot can provide a normal height of the calcaneus so the difference in height can be measured.
SURGICAL TECHNIQUES
Technique 1: Oblique Calcaneal Osteotomy and Arthrodesis
The patient is placed in the lateral decubitus position with the affected limb up and supported on a pad.
Make an incision in the line of the fourth ray from anterior to the calcaneocuboid joint to just behind the fibular malleolus (Fig. 23.10A).
The sural nerve is identified and protected and decompresses if there were neurologic symptoms preoperatively. Peroneal tendons are exposed and mobilized (Fig. 23.10B).
The extensor digitorum brevis is mobilized and retracted, sinus tarsi is cleared of scar tissue, and subtalar joint is opened.
The contracted calcaneofibular ligament is incised, posterolateral capsule is also incised about the joint, and Baby Inge lamina spreaders are used to open the joint.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree