Lower Extremity Nerve Entrapment
Daniel J. Fuchs
Bryant S. Ho
Anish R. Kadakia
DEFINITION
Care of peripheral nerve problems requires knowledge and understanding of nerve pathology, anatomic nerve variations, patterns of nerve damage and entrapment that follow trauma and common operative procedures, and specialized surgical techniques for manipulation of the damaged peripheral nerve.
Unlike other surgical disciplines, a large proportion of peripheral nerve pathology is secondary to postoperative neuropathy, with subsequent treatment reoperative in nature.
Lateral Femoral Cutaneous Nerve
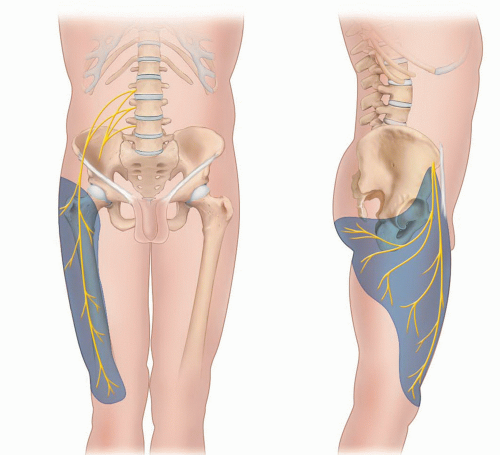
The lateral femoral cutaneous nerve (LFCN) compression is termed meralgia paresthetica and can cause symptoms of pain, numbness, or paresthesias in the anterolateral thigh, as shown in FIG 1.
Compression can be spontaneous or iatrogenic, most commonly following procedures in proximity to the anterior superior iliac spine (ASIS), the inguinal region, or the anterior thigh.
Saphenous Nerve
Saphenous nerve compression or irritation is an often unrecognized cause of knee pain that can mimic other knee conditions and lead to unnecessary, unsuccessful surgical intervention.
Compression most commonly occurs in the upper leg are at the adductor (Hunter) canal and injury most commonly occurs from iatrogenic injury at the level of the knee.
Pes anserinus bursitis and space-occupying lesions are other causes of saphenous nerve compression that have been reported.5
Common Peroneal Nerve
Common peroneal nerve (CPN) injury is characterized by weakness of ankle and foot dorsiflexion (foot drop) as well as loss of sensation over the anterolateral leg and dorsum of the foot.
Surgical procedures and trauma to the lateral knee both represent potential etiologies of CPN injury.
The nerve can become entrapped in postoperative scar tissue, stretched with knee or ankle dislocations, or inadvertently directly damaged, resulting in neuropathy.
Superficial Peroneal Nerve
Superficial peroneal nerve (SPN) pathology is most commonly characterized by pain at the area of compression or injury and symptoms are often activity related.
SPN injury can result from entrapment where the nerve exits the deep crural fascia or from iatrogenic injury during surgery on the lower leg and ankle.
Entrapment as the nerve exits the deep crural fascia can result from a fascial defect with herniation of the peroneal musculature. Alternatively, it can occur at this level from traction injuries that occur in the setting of chronic ankle sprains.
ANATOMY
General Nerve Anatomy
The peripheral nerve has a significant intrinsic blood supply that permits the surgeon to lift the nerve from its anatomic bed, open the epineurium, and operate between the fascicles.11
The endoneurial and perineurial microvessels maintain excellent vascularity to the peripheral nerve. Segmental blood vessels enter the peripheral nerve through the mesoneurium. In addition, an extensive number of longitudinal vessels in the epineurium, perineurium, and endoneurium supply the nerve.12
The “safe” length a nerve can be elevated from its bed (its segmental vascular supply) is a distance of about 60 times the diameter of the nerve.13 The nerve should be
mobilized into an area free from possible external compressible, with care to ensure that the vascular supply is not compromised.
Extreme caution should be exercised in repeat neurolysis of a peripheral nerve due to risk of nerve devascularization.
Lateral Femoral Cutaneous Nerve
The LFCN arises from direct contributions of the L2 and L3 spinal nerve roots, passing between the psoas and the iliacus, and traveling in the retroperitoneal space before reaching the anterior thigh.
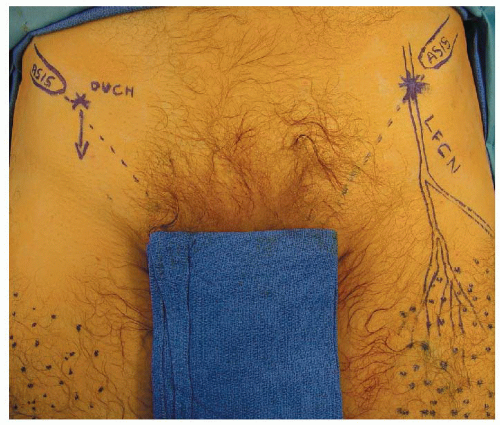
The nerve typically courses medially to the ASIS and traverses the groin crease deep to the inguinal ligament (on average 1 cm medial to the ASIS) as it descends to innervate the thigh.
The nerve course is variable, and LFCN can pass superficially to the inguinal ligament or laterally to the ASIS, running over the iliac crest where there is increased risk of iatrogenic injury.1
The surface anatomy and the most common sites of impingement can be seen in FIG 2.
Saphenous Nerve
The saphenous nerve is a large sensory branch of the femoral nerve that runs with the superficial femoral artery through the adductor canal (Hunter canal).
The adductor canal is located in middle third of thigh and connects the anterior and medial compartments. The apex of the femoral triangle marks the superior extent, and an opening in the adductor magnus, termed the adductor hiatus, marks the inferior extent. The boundaries of the canal are the vastus medialis (lateral), adductor longus and magnus (posteromedial), and a fascial band deep to the sartorius (anterior).
The saphenous nerve divides into two branches prior to becoming subcutaneous at the level of the knee. The infrapatellar branch pierces the sartorius and fascia before turning transversely and running laterally inferior to the patella. The sartorial branch pierces the fascia between the tendons of the gracilis and sartorius before continuing down the medial aspect of the lower leg (FIG 3).
Common Peroneal Nerve
The CPN is one of two main divisions of the sciatic nerve, formed from contributions from the sacral plexus from L4 to S2.
Pathology of the CPN classically occurs when it wraps around the neck of the fibula, deep to the peroneus longus muscle just before splitting into deep and superficial branches (FIG 4).
The CPN, via the deep peroneal nerve branch, innervates the muscles for foot dorsiflexion as well as sensation to the first web space. The SPN branch innervates the peroneals, which perform eversion and provide sensory innervation to the anterolateral lower leg and the majority of the dorsum of foot and toes.
Superficial Peroneal Nerve
The SPN courses inferiorly down the leg most commonly in the lateral compartment, then curves anteriorly and pierces the crural fascia approximately 10 to 12 cm above the tip of the lateral malleolus.
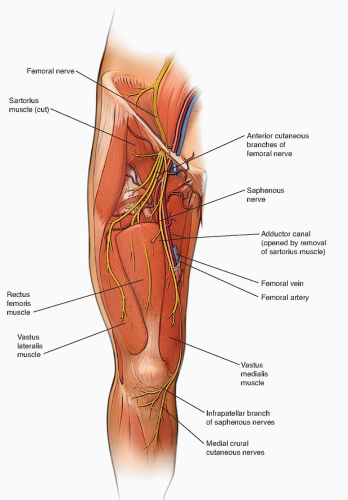
FIG 3 • Anatomy of the saphenous nerve. Note the anatomic relationships of the adductor canal and the division into the infrapatellar and sartorial branches at the level of the knee.
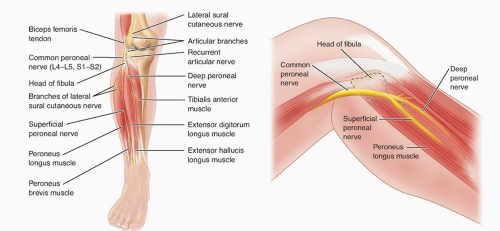
FIG 4 • Anatomy of the CPN. Note the proximity of the nerve to the fibula as it wraps anteriorly on the lower leg.
Variations do exist in which the nerve travels in the anterior compartment and pierces the anterior crural fascia.18
Distally, the nerve courses in the subcutaneous tissue and branches into the intermediate and dorsal cutaneous nerves approximately 6 to 7 cm proximal to the tip of the lateral malleolus.
PATHOGENESIS
Peripheral nerve pathology is due to any process that interferes with neuronal conduction outside of the central nervous system.
Those processes amenable to surgical intervention include nerve damage due to (1) physical compression from anatomically adjacent structures, (2) trauma, and (3) iatrogenic injury.
Peripheral nerve surgery encompasses repair of two common pathophysiologic entities:
Accidental nerve transection or direct crush injury that leads to nerve dysfunction and possible painful neuroma formation.
Scar formation from prior procedures or trauma can engulf a peripheral nerve and compress it; symptomatic relief can then be accomplished through surgical decompression of the peripheral nerve.
Peripheral nerve injury becomes symptomatic either when a critical function is lost or when paresthesia and pain replace normal sensory signaling.
Partial or complete nerve transection causes loss of sensory or motor function because of loss of nerve continuity or disruption of the nerve’s blood supply. The nerve’s regenerative capacity then either reestablishes neuronal continuity or forms a disorganized scar within a mature end-bulb neuroma.
Similarly, compression on a peripheral nerve causes ischemia and neuroma formation.11
A neuroma contains bundled, disorganized nerve endings within a collagenous mass and is an anatomic source of the localized pain and paresthesia following peripheral nerve damage.
Lateral Femoral Cutaneous Nerve
Many cases are iatrogenic and injury to the nerve is a known complication of both orthopaedic and nonorthopaedic surgeries. In the field of orthopaedics, a postoperative nerve palsy can occur following acetabular fracture surgery, pelvic osteotomies, iliac crest bone harvest, anterior total hip arthroplasty, and hip arthroscopy. In other fields, the injury has been noted following laparoscopic hernia repair, bariatric, and gynecologic surgeries.8
LFCN injury can occur as a result of direct mechanical compression. This can be external from a belt or tight-fitting pants and can also be internal from increased intra-abdominal pressure secondary to obesity, pregnancy, or intra-abdominal tumor.
Metabolic factors have been shown to contribute and are often comorbidities in spontaneous cases of LFCN injury. These include diabetes, alcohol abuse, and chronic systemic inflammatory conditions such as lupus.
Saphenous Nerve
Compression of the nerve commonly occurs at the distal aspect of the adductor canal, most commonly from external compression. Other causes include iatrogenic, space-occupying lesions, pes anserinus, or idiopathic. Compression at this level was previously reported in surfers who clenched the surfboard between their legs at the distal aspect of the femur.7 At this level, compression can also occur secondary to thrombosis of the superficial femoral artery.
Iatrogenic injury to the saphenous nerve can occur at the level of the infrapatellar branch as it crosses the knee inferior to the patella. There have been reports of injury at this level following knee arthroscopy or through open surgery using the medial parapatellar approach.15 Injury can occur along the sartorial
branch of the nerve as well at the level that it runs with the greater saphenous vein. The nerve is commonly injured at this level in vein stripping or vein harvesting procedures.16
Common Peroneal Nerve
CPN injuries have a particularly wide range of etiologies.
Trauma is a common etiology of CPN injury—either direct blow to the lateral knee, ankle fracture with a proximal fibula fracture, or a high energy or sports injury causing a multiligament knee injury.
Iatrogenic injury can occur from arthroscopic or open knee procedures. Total hip arthroplasty and total knee arthroplasty have low but reportable incidences of CPN palsy that are often secondary to external compression from intraoperative positioning.
Space-occupying lesions can compress the CPN. These include intraneural ganglia and proximal tibia-fibular joint cysts.2
Metabolic conditions including diabetes mellitus and hyperthyroidism can result in mononeuropathies of the CPN.
Superficial Peroneal Nerve
Compression often occurs at the level where the SPN pierces the crural fascia and becomes subcutaneous. There can be focal herniation of the peroneal musculature at this level, causing compression. This pathology can occur in isolation or can be in addition to an underlying exertional compartment syndrome.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree