Limited Wrist Arthrodesis
Michael N. Nakashian
Andrew W. Cross
Mark E. Baratz
DEFINITION
Limited wrist arthrodeses are salvage procedures for posttraumatic and degenerative conditions of the wrist as well as symptomatic instabilities.
The goal is to reduce pain by selected fusion of the affected joints, thereby sparing motion, and improving the function of the remaining joints.
ANATOMY
The carpus consists of four bones in the proximal row (scaphoid, lunate, triquetrum, pisiform) and four bones in the distal row (trapezium, trapezoid, capitate, hamate).
The scaphoid and lunate bones are intimately joined by the scapholunate ligament both dorsally and volarly. This ligament is critical to the kinematics of the wrist.
Many other named ligaments hold the carpal bones stable as the wrist moves through its five planes of motion (flexion, extension, radial and ulnar deviation, and circumduction).
Most reconstructive wrist procedures require a dorsal approach to the wrist. The wrist and finger extensor tendons are separated into six compartments by the dorsal extensor retinaculum. The most common interval for exposure of the wrist is the third and fourth interval between the extensor pollicis longus (EPL) and extensor digitorum communis and extensor indices proprius tendons.
PATHOGENESIS
Distraction forces across the joint as well as twisting motions while the wrist joint is being loaded can both result in a ligament injury.
Failure of the scapholunate interosseous ligament, either by trauma or inflammatory arthritis, allows the scaphoid to flex and the lunate to extend, leading to dorsal intercalated segment instability (DISI).20,35 When this occurs, abnormal loading of the carpal bones results. This eventually leads to degenerative arthritis, particularly at the radioscaphoid joint due to the abnormal distribution of force across this elliptical joint.7 This has been termed scapholunate advanced collapse (SLAC).
Scaphoid nonunion advanced collapse (SNAC), perilunate dislocations, calcium pyrophosphate dihydrate deposition, and rheumatoid arthritis can also lead to this pattern of arthritis.
Other ligament injuries, Kienböck disease, and localized arthritis can lead to wrist pain, instability, and deformity.
NATURAL HISTORY
Much of our knowledge of the natural history of scaphoid nonunion was reported by Mack et al.23 We have learned that most ununited fractures of the scaphoid and SLAC wrists develop progressive osteoarthritis in a predictable pattern.
Cyst formation and bony resorption are the hallmarks of arthritis and are usually seen 5 to 10 years after injury.
PATIENT HISTORY AND PHYSICAL FINDINGS
Typically, the patient describes a traumatic injury to the wrist. The absence of trauma should not exclude traumatic causes.
Painful wrist motion and a limited arc of motion are common findings.
Methods for examining the wrist include the following:
Finger extension test.32 The wrist is passively flexed while the examiner resists active finger extension. A positive test yields pain and may represent periscaphoid inflammatory changes, radiocarpal or midcarpal instability, or Kienböck disease. A negative test essentially excludes dorsal wrist syndrome, Kienböck disease, midcarpal instability, and SLAC as the cause of pain.
Anatomic snuffbox palpation.32 The examiner palpates the anatomic snuffbox with the index finger while moving the wrist from radial to ulnar deviation.30 A positive test yields severe pain at the articular-nonarticular junction of the scaphoid. Periscaphoid synovitis, scaphoid instability, and radial styloid arthrosis from SLAC are possible causes.
Triscaphe (scaphotrapeziotrapezoid [STT]) joint palpation.32 The examiner palpates the second metacarpal proximally until it falls into a recess, the triscaphe joint. Pain with palpation indicates pathology of the distal scaphoid or the triscaphe joint.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs, including anteroposterior (AP), lateral, oblique, and scaphoid views, should be obtained.
The stage of wrist arthritis, as seen on plain radiographs, helps to determine the treatment options. Watson and Ballet31 classified the radiographic findings into stages I to III.
Stage IV, not originally described, demonstrates arthritis in most all joints of the wrist. Fortunately, the radiolunate joint is rarely involved and serves as the basis for several treatment options.
Arthritis involving the radiolunate joint is usually seen only in patients with inflammatory wrist arthritis.
NONOPERATIVE MANAGEMENT
Nonoperative measures include rest, anti-inflammatory medications, splinting, occasional casting for flare-ups of arthritis, and cortisone injections.
SURGICAL MANAGEMENT
Indications
Four-corner (capitate-hamate-lunate-triquetral [CHLT]) arthrodesis
Stage II or III SLAC wrist arthritis
Chronic symptomatic volar intercalated segmental instability (VISI) deformity or midcarpal instability
STT arthrodesis
Chronic static or dynamic scapholunate instability
STT arthritis
Kienböck disease
Radiocarpal instability
Lunotriquetral arthrodesis
Lunotriquetral ligament tears
Posttraumatic instability
Scapholunate arthrodesis
Posttraumatic instability
Scapholunate instability
DISI deformity
Scaphocapitate arthrodesis
Scaphoid nonunion
Chronic DISI deformity with rotatory scaphoid instability
Kienböck disease
Lunate nonunion
Radiolunate arthrodesis
Rheumatoid arthritis primarily involving the radiolunate joint
Ulnar translocation of the carpus (relative indication)
Capitolunate arthrodesis
Scaphoid nonunion
SLAC wrist arthritis
Preoperative Planning
The patient’s history and pertinent physical examination findings are reviewed.
Any prior surgical scars are noted.
All radiographs are reviewed, noting any associated pathology that might need to be simultaneously addressed to yield the best outcome.
Postoperative pain control should be discussed with the patient and the anesthesia team, and a local or axillary block should be considered for prolonged pain relief after surgery.
Positioning
The patient is placed in the supine position on the operating table with the arm draped to the side on a radiolucent arm board.
A tourniquet is used to control bleeding during the procedure.
Approach
The wrist is approached through a dorsal longitudinal incision between the third and fourth extensor compartments.
Alternatively, the fourth and fifth extensor compartment interval may be used to better visualize the CHLT articulations.
The EPL tendon sheath is opened and it is released both proximally and distally. The tendon is allowed to be transposed out of its compartment in a radial direction.
Although the EPL tendon is typically exposed and subsequently transposed, a more limited incision beginning just distal to the tubercle of Lister and proceeding distally may avoid significant exposure of the EPL tendon altogether.
All joints are exposed fully and a precise decortication is performed down to bleeding bone.
In almost every case, bone graft is harvested from the distal radius and used to augment the fusion.
Iliac crest graft may be substituted but is associated with higher donor site morbidity.
TECHNIQUES
▪ Four-Corner (Capitate-Hamate-Lunate-Triquetral) Arthrodesis Using Kirschner Wire Fixation
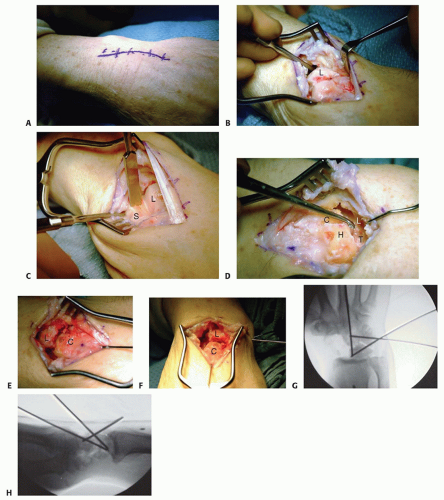
Make a standard dorsal longitudinal incision between the third and fourth extensor compartments using the tubercle of Lister as a landmark (TECH FIG 1A).
Incise the retinaculum over the third extensor compartment.
Incise the radial septum of the fourth extensor compartment and retract the tendons ulnarly.
Perform a ligament-splitting dorsal approach to the carpus as described by Berger et al.4
This capsular incision allows access to the carpus while preserving the dorsal intercarpal ligament and dorsal radiotriquetral ligament (see Chap. 70).
Inspect the radiolunate joint for articular cartilage wear (TECH FIG 1B).
Identify and excise the scaphoid either piecemeal with a rongeur or sharply using a scalpel (TECH FIG 1C).
Kirschner wires and tenaculum clamps facilitate the visualization and excision of the distal volar scaphoid.
Take care to protect the volar radioscaphocapitate ligament.
Once the scaphoid is excised, decorticate the opposing joint surfaces of the lunate, triquetrum, capitate, and hamate (TECH FIG 1D).
Longitudinal traction with fingertraps helps to distract these joints, making decortication easier.
Thorough removal of the volar-third cartilage from the lunate and capitate facilitates correction of the preexisting DISI deformity but shortens the intercarpal bone distances. This may restrict final wrist range of motion.
Once these joint surfaces are denuded, harvest distal radius bone graft and place it into the fusion bed.
Use a 0.062 Kirschner wire to joystick the lunate into a more flexed position, and apply dorsal pressure to volarly translate the
capitate on the lunate. Place one or two 0.062 Kirschner wires across this joint (TECH FIG 1E).
Verify correction of the DISI deformity using fluoroscopy.
Pin the lunotriquetral joint and the capitohamate joint with two 0.062 Kirschner wires (TECH FIG 1F).
Intraoperative fluoroscopic images should reveal a stable triangular construct of Kirschner wires traversing the four bones (TECH FIG 1G,H).
The Kirschner wires may be cut under the skin or left external, depending on the surgeon’s preference.
After irrigation, close the capsule with absorbable suture and repair the extensor retinaculum, leaving the EPL tendon transposed subcutaneously.
Close the skin in a routine manner.
Apply a large bulky dressing including a dorsal and volar forearm-based splint.
The previously described technique is taken from published data.2
▪ Four-Corner Arthrodesis Using a Circular Plate
The approach, scaphoid excision, and joint preparation are analogous to those described earlier.
Place a 0.062 Kirschner wire through the distal radius articular surface. Use a separate 0.062 Kirschner wire as a joystick to hold the lunate reduced in neutral alignment while advancing the Kirschner wire across the radiolunate joint in a dorsal to volar direction.
Obtain fluoroscopic images to verify correction of the dorsally tilted lunate.
After volarly translating the capitate (as described earlier) and fully correcting the DISI deformity, secure the triquetrum to the hamate and the lunate to the capitate with two additional Kirschner wires.
Place these Kirschner wires as volar as possible to avoid interference during rasping and plate placement.
Center the power rasp over the four bones in the AP and lateral planes and bury the rasp down to subchondral bone.
Ideal rasp placement does not always coincide with the central point between the four bones.
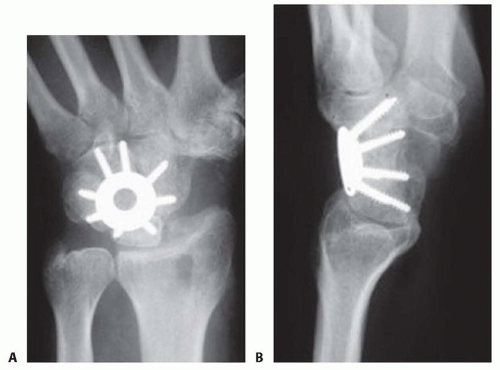
TECH FIG 2 • A,B. AP and lateral radiographs showing a circular plate fusion construct. On the lateral view, the plate is nicely seated to prevent dorsal impingement.
Pack bone graft, obtained preferably from the distal radius or iliac crest, between the four prepared bones.
Center the plate over the four bones in the AP and lateral planes and place the circular plate into the bony crater created by the rasp.
Rotate the plate to maximize screw purchase into each of the four bones. Two screws should be planned for each of the four carpal bones.
All screws must be placed in a unicortical fashion.
Place the first screw through the plate into the lunate. Do not tighten this screw completely or it will cause the circular plate to tilt up and compromise screw fixation in the remaining bones.
Place a second screw into the hole opposite the first screw. This sets the plate position.
Check a lateral fluoroscopic image to ensure the plate is well seated and there is no impingement with wrist extension.
Fill in the remainder of the holes with screws.
Placing the screws opposite one another and tightening them sequentially helps prevent malpositioning of the plate.
Obtain final images to check screw length and position, carpal reduction, and construct stability (TECH FIG 2).
Close the wound as described earlier. Apply the dressing and splint.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree