Ligamentous Lisfranc Joint Injuries: Leg/Ankle/Foot: Midfoot Injuries, Lisfranc
Michael S. Aronow MD
The tarsometatarsal (TMT), or Lisfranc, joints consist of the five metatarsals and their articulation with the corresponding cuneiforms and cuboid.
The first, second, and third TMT joints undergo slight dorsiflexion, plantarflexion, supination, and pronation motion that helps absorb shock; however, their principal function is to act as a rigid lever connecting the hindfoot to the forefoot.
In a Lisfranc injury, there is instability, subluxation, or dislocation of the TMT joints secondary to ligament disruption often with associated bone fractures.
In most displaced Lisfranc injuries, the relatively weak dorsal TMT ligaments are disrupted first, followed by rupture of stronger plantar and interosseus ligaments, which in conjunction with more substantial plantar soft tissue support, usually displaces the metatarsals dorsally.
In severe injuries with dislocation of the TMT joints, there is pain, swelling, deformity, inability to bear weight, and occasionally neurovascular compromise.
Visualization of the TMT joints is improved with the x-ray beam angled parallel to the TMT joint surfaces for the anteroposterior (AP) and 30 (degree) oblique views.
An anatomic reduction of the TMT joints restoring articular congruity decreases the risk of arthritic pain and functional loss. Pure ligamentous injuries do not always heal and may cause long-term disability.
Lisfranc injuries without subluxation on weight-bearing or stress x-rays are treated nonoperatively.
Immediate intervention is required in the presence of open injuries, forefoot compartment syndrome, or neurovascular compromise of the forefoot. Significant deformity and dislocation requires early reduction, preferably open reduction with fixation, to prevent further skin, soft tissue, or neurovascular compromise.
Outcomes after Lisfranc injury improve with quality of TMT joint reduction. Factors causing poor outcome include high-energy injuries with increased initial articular and soft-tissue damage, delay in diagnosis, and possibly pure ligamentous injuries.
Anatomy
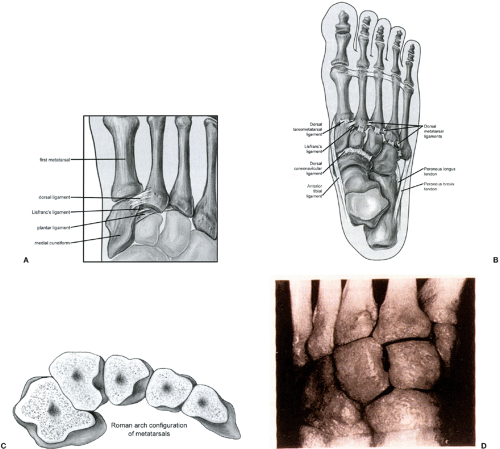
The tarsometatarsal (TMT), or Lisfranc, joints consist of the five metatarsals and their articulation with the corresponding cuneiforms and cuboid. TMT joint stability comes from a combination of bone morphology, ligaments, and soft tissue support (Fig 52-1). The second metatarsal base forms a keystone where it articulates with all three cuneiforms. The metatarsal bases, cuneiforms, and cuboid are wedge-shaped bones that form a stable roman arch configuration. Ligaments cross the TMT, naviculocuneiform, and intercuneiform joints. Ligaments connect the second through fifth metatarsal bases, but not the first and second. The strong interosseus Lisfranc’s ligament connects the medial cuneiform to the medial second metatarsal base. There is a less strong plantar ligament from the medial cuneiform to the plantar aspect of the second and third metatarsal bases and a weaker still dorsal ligament from the medial cuneiform to the medial second metatarsal base (1,2). Additional plantar arch support comes from the
intrinsic foot muscles, and the posterior tibial, anterior tibial, and peroneus longus tendons. The plantar fascia acts as a tie rod to support the arch.
intrinsic foot muscles, and the posterior tibial, anterior tibial, and peroneus longus tendons. The plantar fascia acts as a tie rod to support the arch.
Biomechanics
The first, second, and third TMT joints undergo slight dorsiflexion, plantarflexion, supination, and pronation motion that helps absorb shock; however, their principal function is to act as a rigid lever connecting the hindfoot to the forefoot. The fourth and fifth TMT joints have more motion which helps accommodate the forefoot on uneven terrain (3).
In a Lisfranc injury, there is instability, subluxation, or dislocation of the TMT joints secondary to ligament disruption and/or bone fractures. Lisfranc injuries occur by both direct and indirect mechanisms. Motor vehicle accidents and crush injuries are examples of direct injuries with dorsally or plantarly directed blows with a rotational component. The indirect mechanism of injury involves an axial force to a plantarflexed foot with subsequent rotation. Examples include a fall on the stairs, sports injuries when another player lands on the posterior heel of the plantarflexed foot, or with abduction of a foot fixed in a stirrup in equestrian and windsurfing injuries. In most displaced
Lisfranc injuries the relatively weak dorsal TMT ligaments are disrupted first, followed by rupture of stronger plantar and interosseus ligaments, which in conjunction with more substantial plantar soft tissue support, usually displaces the metatarsals dorsally.
Lisfranc injuries the relatively weak dorsal TMT ligaments are disrupted first, followed by rupture of stronger plantar and interosseus ligaments, which in conjunction with more substantial plantar soft tissue support, usually displaces the metatarsals dorsally.
History and Physical Findings
In severe injuries with dislocation of the TMT joints there is pain, swelling, deformity, inability to bear weight, and occasionally neurovascular compromise. In subtle injuries there is usually pain, swelling, and tenderness, although it is usually less extensive and may be limited to the area over Lisfranc’s ligament. Heel weight-bearing is painful, but often possible. There may be a plantar ecchymosis sign (4) in which there is ecchymosis of the plantar medial arch or a gap sign (5) in which there is diastasis between the hallux and second toe. There may be no deformity or loss of the medial longitudinal arch with weight-bearing only. Often the diagnosis is made late as the investigations are equivocal, or nonweight-bearing views obtained.
Imaging
Weight-bearing anteroposterior (AP), 30 degree oblique, and lateral views of the foot are taken with the ankle in dorsiflexion. For subtle injuries comparison views of the foot are performed at the same time. Visualization of the TMT joints is improved with the x-ray beam angled parallel to the TMT joint surfaces for the AP and 30 degree oblique views (about 17 degrees from perpendicular to the floor, which can be measured on the lateral x-ray). If x-rays do not show subluxation or dislocation, stress x-rays should be taken to rule out ligamentous instability. The cuboid and medial cuneiform are stabilized and then the AP view is repeated while abducting, adducting, and then divergently stressing the first and second metatarsals. Often a fleck sign (6) is seen, representing an avulsion fracture of the medial second metatarsal base at the attachment site of Lisfranc’s ligament. Other fractures within the midfoot can occur, including a compression fracture of the cuboid. Magnetic resonance imaging (MRI) and computed tomography (CT) may show fractures not seen by plain x-ray, TMT joint subluxation, and Lisfranc ligament disruption (7). In a cadaver study, unlike computerized tomography, plain radiographs could not detect 1 mm of second TMT joint displacement and could not detect 2 mm of displacement 33% of the time (8). Because MRI or CT can rarely be obtained with simulated weight-bearing, however, TMT joint subluxation may be missed on these investigations. Bone scans can confirm TMT joint injury or sprain in the absence of TMT joint subluxation.
Decision Making Algorithms and Classification
After the diagnosis of a Lisfranc injury has been made by history, physical examination, and imaging studies, the amount of TMT or inter-cuneiform joint malalignment must be determined. While multiple criteria for “significant” displacement have been advocated, the amount of subluxation or displacement resulting in a poorer functional outcome has not been definitively determined. Athletes tolerate less displacement as they expect a higher level of function.
In most clinical studies, the indications for surgical intervention and the assessment of reduction are based on the distance between the lateral border of the first metatarsal and the medial border of the second metatarsal (6,9,10,11,12,13,14,15,16,17,18,19). The radiographic criteria for an anatomic reduction has ranged from a first-second metatarsal distance of ≤2 mm (6,9,11,15,16) to ≤5 mm (12,19). In two studies (11,14), the foot with a Lisfranc injury had a first-second metatarsal distance of between 2 to 5 mm, while the distance in the normal contralateral foot was noted to average either 1.3 mm (10) or range from to 1 to 5 mm (14). As the anatomy varies between different patients the assessment should be based on the opposite uninjured foot.
Although it more directly reflects disruption of Lisfranc’s ligament, the distance between the lateral border of the medial cuneiform and the medial border of the second metatarsal has been used less commonly. In one study, MRI and weight-bearing x-rays were taken of both the injured and contralateral normal foot. The medial cuneiform-second metatarsal distance ranged from 2 to 5 mm on x-rays of the normal foot. On MRI, the distance ranged from 1 mm less to 3 mm more than the normal side in 18 patients with MRI-determined partial Lisfranc ligament tears, and was at least 2 mm greater than the uninjured foot in three patients with complete Lisfranc ligament ruptures (14).
Malalignment of the first and second TMT joints can be measured on the AP x-ray and the third and fourth TMT joints on the 30 degree oblique (20). The medial and lateral aspects of the first, second, and third metatarsal should line up with the medial and lateral aspects of the medial, intermediate, and lateral cuneiform, respectively. The medial aspect of the fourth metatarsal should line up with the medial aspect of the cuboid. In most displaced Lisfranc injuries at least one of the medial two TMT joints will be subluxed. The exception is isolated injuries to both the medial-intermediate intercuneiform and Lisfranc’s ligaments in which only the medial cuneiform-second metatarsal distance and first-second metatarsal distance will be increased. Open reduction and internal fixation has been recommended for 2 mm or more displacement of any of the TMT joints (21). In cadavers, 1 mm of dorsolateral displacement of the second metatarsal produced an average of 13.1% decreased second TMT joint contact, 2 mm of dorsolateral displacement produced an average of 25.5% decreased second TMT joint contact, and 4 mm of dorsolateral displacement produced an average of 50.6% decreased second TMT joint contact (22).
On an AP abduction stress x-ray, a Lisfranc injury is likely if a line drawn tangential to the medial aspect of the medial cuneiform and navicular does not intersect the first metatarsal base (23).
On the lateral x-ray the dorsal and plantar aspects of the metatarsals should line up with the corresponding cuneiform or cuboid. Faciszewski et al. (11) found patients with flattening of the longitudinal arch had a poor prognosis and should undergo open reduction and internal fixation. They defined a flattened arch as when the medial cuneiform was plantar to the fifth metatarsal base or when the same distance was 1.5 mm greater than the normal foot. Myerson et al. (6) recommended open reduction if the lateral talo-first metatarsal angle was greater than 15 degrees. However, all three of these lateral x-ray findings may be occasionally seen in patients with asymptomatic, atraumatic flatfoot deformities.
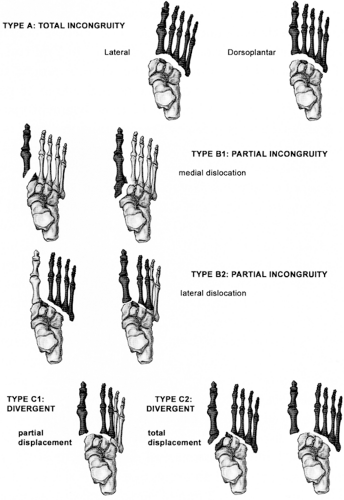
The most commonly used classification system is Myerson et al.’s (6) modification of Hardcastle et al.’s (24) modification of Quenu and Kuss’s (25) classification (Fig 52-2). There are three main types: Total Incongruity—all five metatarsals subluxing the same direction (Type A); Partial Incongruity—the first metatarsal subluxing medially (Type B1) or one or more of the lateral four metatarsals subluxing laterally (Type B2) with or without a component of dorsal/plantar subluxation; and Divergent—the first metatarsal subluxing medially and some (Type C1) or all four (Type C2) of the lateral four metatarsals subluxing laterally and/or dorsal/plantarly.
Nunley and Vertullo (26) described a midfoot sprain classification system for athletes. Stage I is a Lisfranc ligament sprain with no diastasis or arch height loss seen on weight-bearing radiographs but increased uptake on bone scintigrams. Stage II sprains have a 1 to 5 mm diastasis between the first and second metatarsals compared to the contralateral foot with no arch height loss. Stage III sprains have a first to second metatarsal diastasis greater than 5 mm and loss of arch height as described by Faciszewski et al. (11). Only Stage I and II sprains were reported on in their study.
The goal of treatment is a pain-free functional foot. An anatomic reduction of the TMT joints restoring articular congruity should decrease the risk of developing painful arthritis and preserve function. The reduction should be maintained until ligamentous stability has been restored to preserve the height of the longitudinal arch. With rare exception (27), most studies show outcome after Lisfranc injury improves with better TMT joint reduction (6,9,10,12,13,15,16,19,24,28,29,30,31,32,33,34,35). This stability may be obtained fairly quickly in incomplete ligament tears or after bone healing of large avulsion fractures attached to Lisfranc’s ligament. Ligamentous stability takes longer or may not occur at all in patients with pure ligamentous injuries or a small Lisfranc’s ligament avulsion fracture (32,33). As a principle of general trauma care, treatment should also minimize additional trauma to the soft tissues and articular surfaces.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree