Ligament Stabilization of the Unstable Thumb Carpometacarpal Joint
Richard Y. Kim
Robert J. Strauch
DEFINITION
Thumb carpometacarpal (CMC) joint instability can occur as a result of ligament laxity or trauma.
Regardless of the cause, injury to the stabilizing ligaments surrounding the CMC joint leads to instability and dorsoradial subluxation or dislocation of the thumb metacarpal.
ANATOMY
The thumb CMC joint is a biconcave-convex joint similar to a horseback rider’s saddle.5
The base of the thumb metacarpal has a prominent volar styloid process (beak) that articulates with a recess in the volar trapezium when in flexion.
There are 16 ligaments that provide stability to the thumb CMC joint.1 Of these ligaments, the two that provide the most restraint against dorsoradial subluxation of the thumb metacarpal are the dorsoradial and volar beak ligaments (FIG 1).1,5,11,15,18 A recent systematic review of the literature demonstrates that the dorsal ligaments are the primary stabilizers of the thumb CMC joint.10
The volar beak ligament (deep anterior oblique ligament, palmar ligament, ulnar ligament) originates from the volar central apex of the trapezium and inserts onto the volar beak of the thumb metacarpal.1 It lies immediately under a more widely based superficial anterior oblique ligament, which is located immediately deep to the thenar musculature and has a broad insertion across the base of the thumb metacarpal. More recent studies indicate that the beak ligament may not be as substantial as once thought.
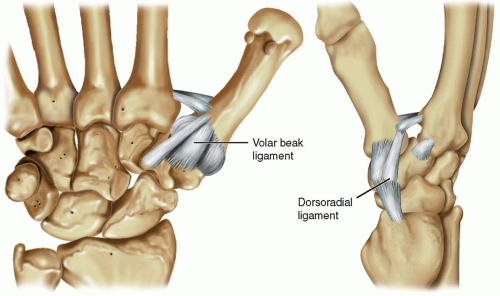
FIG 1 • The stabilizing ligaments of the thumb CMC joint. Of these, the dorsoradial and volar beak ligaments are the most important in preventing dorsoradial subluxation of the thumb metacarpal.
The dorsoradial ligament originates from the dorsoradial tubercle of the trapezium and inserts onto the dorsal base of the thumb metacarpal. It is the thickest, widest, shortest, and strongest of the CMC ligaments.5
PATHOGENESIS
The biconcave-convex nature of the thumb CMC joint allows for a wide range of thumb motion but is inherently unstable.8 Laxity or incompetence of the supporting ligaments, especially the dorsoradial ligaments, will cause instability of the thumb CMC joint.12,15 Especially in middle-aged women, the cause of the laxity is often idiopathic.
In addition, there is a population of patients who have inherent ligament laxity, such as those with collagen disorders such as Ehlers-Danlos syndrome.
NATURAL HISTORY
Ligamentous laxity at the thumb CMC joint may cause degenerative changes to the joint cartilage and lead to arthritis,
corresponding to higher stages in the Eaton-Littler staging system.3
If the ligamentous laxity is symptomatic and causing pain, ligament reconstruction can be successful in reducing pain in over 90% of patients. Ligament reconstruction has also been shown to potentially halt the progression of arthritis.6
For traumatic dislocations, a stable reduction is important for thumb function. If the thumb CMC joint remains unstable, functions such as key pinch and grasp may be compromised.
Open ligament reconstruction of these unstable thumb CMC joint dislocations may decrease the incidence of recurrent instability and joint degeneration compared to closed reduction and pinning.14
PATIENT HISTORY AND PHYSICAL FINDINGS
Nontraumatic Ligamentous Laxity
The history should include questions about ligament laxity involving other joints. Metabolic diseases such as Ehlers-Danlos syndrome are notable.
Radiographic findings often do not correlate with symptomatology. Therefore, it is important to elicit from the patient the exact symptoms and their severity.
Any history of previous nonoperative treatments should be noted. If splinting and steroid injections have not been attempted, it may be beneficial to attempt these treatment modalities before discussing surgery.
The physical examination should determine the degree of subluxation and reducibility of the thumb CMC joint.
The thumb metacarpophalangeal (MCP) joint should also be examined for possible hyperextension laxity.
Pinch strength and opposition should be tested and compared to the contralateral side.
The hand should also be evaluated for concomitant carpal tunnel syndrome, flexor carpi radialis tunnel syndrome, and de Quervain tenosynovitis, as these may also need to be addressed.
Traumatic Injuries
In addition to the evaluation cited for nontraumatic laxity, the history and physical examination should include the following:
Time and nature of the injury
Status of the thumb before injury
Stability of joint reduction: This is of major concern in the physical examination because assessment of stability will determine the treatment path.
Associated MCP joint collateral ligament injury and stability
Other associated hand injuries are important to note as well.
Tests to perform include the ballottement test and the grind test.
Tenderness associated with dorsal pressure indicates symptomatic subluxation.
Crepitance and pain are positive indicators of CMC pathology.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP), lateral, and oblique views of both thumbs should be obtained.
A true AP (Robert) view is taken with the forearm in maximal pronation and the dorsum of the thumb resting on the imaging table. The beam is then angled 15 degrees from distal to proximal.5
A true lateral film of the thumb is one in which the sesamoids volar to the thumb MCP joint overlap each other.
A 30-degree oblique stress view of the thumb CMC joint is performed by pressing the radial side of the thumb tips together. This maneuver will subluxate the thumb metacarpal base radially, thereby demonstrating the degree of laxity in the radial direction.17
DIFFERENTIAL DIAGNOSIS
de Quervain tenosynovitis
Flexor carpi radialis tunnel syndrome
C6 radiculopathy
Trigger thumb
NONOPERATIVE MANAGEMENT
For symptomatic ligament laxity and stage I or II basal joint disease, conservative management should first be attempted. This includes thumb spica splint immobilization and anti-inflammatory medications.7,16
If the symptoms do not improve, a steroid injection into the CMC joint can be attempted. The number of injections should be limited to a maximum of three; theoretically, more than three injections increases joint morbidity.
In the scenario of acute trauma, reduction of the CMC joint should be performed by applying axial traction and palmardirected pressure to the base of the thumb metacarpal, along with pronation of the thumb metacarpal. After reduction, if the joint remains reduced and is stable, the injury can be treated with cast immobilization.
If the joint is unstable at all after an attempt at closed reduction, surgical management is indicated.14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








