Inversion ankle sprains are among the most common injuries in active people. Many patients experiencing ankle sprains will suffer recurrent sprains and ultimately chronic instability, estimated between 20% and 40% (
1). When approaching the patient with lateral instability, it is important to define the origin and extent of instability. In general terms, this can be defined as isolated lateral (tibiotalar) instability, isolated subtalar instability (
2,
3,
4,
5 and
6) sinus tarsi syndrome (
7,
8 and
9), or combined ankle/subtalar instability.
Rubin and Witten (
10) were the first to suggest clinical significance of subtalar instability. They developed a foot holding device to evaluate patients, obtaining varus stress tomograms. Among the 27 patients tested in their series, only 17 had symptoms of instability—and none were found to have abnormal tomogram. Laurin et al. (
11) performed cadaver ligament sectioning and obtained stress tomograms, identifying the calcaneofibular ligament (CFL) as an important stabilizer of the subtalar joint. They determined that manual testing is as good as a foot holding device. Chrisman and Snook (
12) recognized subtalar instability in combination with ankle instability intraoperatively. Their modification of the Elmslie technique eliminated subtalar instability in patients with combined ankle/subtalar instability (
12). Brantigan et al. (
13) employed the method of Rubin and Witten in patients with subtalar instability, advocating stress tomograms for diagnosis of this entity.
It is believed by many that repair of locally scarred tissues, as with a standard Broström procedure, is inadequate in high-demand individuals. This concern applies regardless of the level of injury, whether tibiotalar, subtalar, or a combination. Thus, augmenting the standard Broström and Broström/Gould procedures with a split transfer of the peroneus brevis may be beneficial in certain individuals. The procedure is described herein.
The Evans procedure is a nonanatomical lateral ligament reconstruction described in 1953 (
14) as a dynamic stabilization of the ankle and subtalar joints. In this technique, the peroneus brevis tendon is divided below the musculotendinous junction and passed through a tunnel drilled in the fibula, then reattached to its muscle belly. Since the initial description, the procedure has been modified by two main variations. The first variation involved routing the entire peroneus brevis tendon through a fibular tunnel posteriorly-superiorly, and then attaching it to periosteum (
15,
16) or alongside its insertion at the base of the fifth metatarsal (
17,
18), allowing it to act as a tenodesis rather than a dynamic stabilizer. In the second variation, the “split Evans” procedure, a portion of the tendon is divided, remaining attached at its distal insertion, advanced through the fibular tunnel and sutured to the fibular periosteum (
19,
20). Some are concerned that the Evans procedure “locks” the subtalar joint in eversion, increasing joint forces laterally and leading to subtalar degeneration. The split Evans procedure described in this chapter takes care to avoid overtightening the subtalar joint by tensioning the transfer in neutral and therefore acting as a checkrein to inversion forces, while permitting a reasonable degree of eversion.
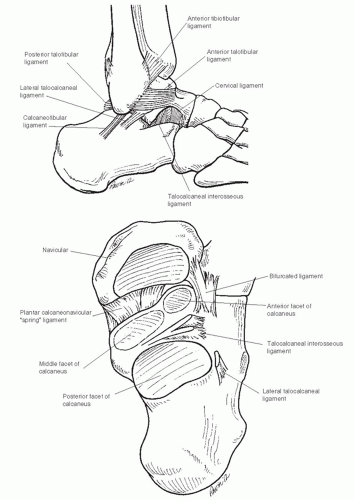
The subtalar joint is complex in its articulations, ligamentous support, and motion. The joint is stabilized by both external and internal ligamentous restraints. The external restraints include
The CFL is a primary stabilizer of both the ankle and subtalar joints and is the greatest contributor to stabilization of the subtalar joint (
21). Internal restraints include (
Fig. 30.1)
Fibulotalocalcaneal ligament (ligament of Rouviere)
The ligament of the anterior capsule of the posterior facet joint
Cervical ligament (this ligament runs obliquely from anterior calcaneus to the superior talar neck)
Interosseous ligament (which lies between the anterior and middle facets) (
2)
The spring ligament may also impart some medial subtalar stability.
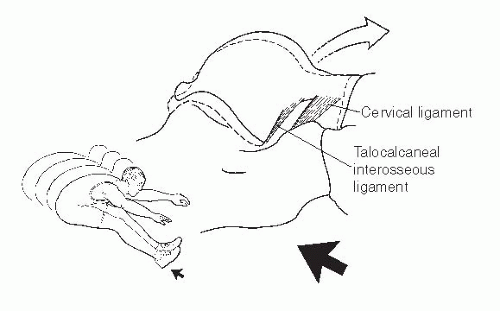
Patients will frequently describe an acute inversion type of injury and complain of pain and swelling in the lateral ankle. Pisani (
3) described a “whiplash mechanism” of injury to the interosseous ligament (
Fig. 30.2). This abrupt impact and deceleration of the calcaneus leads to stretching of the TCL and interosseous ligament and chronic laxity in jumping athletes (basketball players and triple jumpers).
Patients complain of symptoms that are similar to those described for ankle instability. There is often a history of frequent ankle inversion sprains (foot rolls under the patient), particularly on uneven ground and during athletic activities when cutting or sudden direction change. Sometimes, a relatively benign action such as stepping on a pebble may induce an inversion episode. The physical examination of subtalar instability can be difficult and subjective. Functional instability usually has normal exam. Manually stressing the foot into varus with the ankle in dorsiflexion assesses the integrity of the CFL and TCL. In cases of subtalar instability, calcaneus tilts into varus while talus remains stable within mortise. Occasionally, a “click” or “clunk” may be perceived. Comparison to the contralateral extremity is important since patients will have different degrees of inherent ligamentous laxity.
It can be difficult to differentiate ankle from subtalar instability. Many patients will present with combined instability, manifesting as a gap between lateral talar process and distal fibula, often with a dimple in the skin. It is likely that with mechanical instability of the subtalar joint, there is rupture or attenuation of the CFL, and some degree of lateral ankle instability would be present as well since the CFL is a primary stabilizer of both joints. Again, a thorough history and comparison to the contralateral ankle are key to the diagnosis (
Tables 30.1 and
30.2).
Weight-bearing anteroposterior (AP), mortise, and lateral plain radiographs should be obtained routinely. In the absence of fracture or obvious subchondral abnormality, plain radiographs are usually normal. Stress views of ankle can also be obtained. A normal ankle will have a tibiotalar tilt that is less than 12° or within 5° of the contralateral ankle. Stress radiographs with Broden’s views of the subtalar joint can indicate angular instability (demonstrated by loss of facet parallelism) (
2) although it has been suggested that this method does not sufficiently address translation and rotatory instability (
4). Anterior translation of the posterior facet of the calcaneus relative to the talus has also been suggested as a method to diagnose subtalar instability (
5), although these views are difficult to obtain.
Live fluoroscopy can provide a reasonable dynamic evaluation to determine whether significant hypermobility exists. Arthrography has also been suggested as a method to determine the extent of injury to the subtalar joint (i.e., delineate injury to the ligamentous stabilizers of the subtalar joint) (
6,
9), although this invasive study may not be feasible in clinical practice due to additional expense and morbidity. MRI can be useful to assess for changes in the sinus tarsi (sinus tarsi syndrome) and to identify tears in the CF, cervical, and interosseous ligaments (
22). Associated intraarticular and tendinous injuries can also be identified by MRI. Subtalar arthroscopy can be a useful diagnostic and therapeutic tool in some patients (
23,
24).
Hindfoot varus is the most commonly associated condition in patients with chronic lateral and combined ankle instability (
25) and is a common cause of failure of lateral ligament reconstruction (
26). On clinical examination, it is important to assess hindfoot alignment and determine whether the heel is in true varus or whether it is secondary to plantarflexed first ray. On standing examination, the “peek-a-boo” heel sign, or visualization of the heel while viewing the patient from the front, can indicate hindfoot varus (
27). The Coleman block test can be used to determine flexibility of the hindfoot (
28). Peroneal tendon tears and tenosynovitis can also be associated with cavovarus alignment and result in loss of dynamic support for lateral ankle. It is important to assess clinically for injury to the peroneus brevis and peroneus longus and for painful os peroneum syndrome (POPS).
INDICATIONS AND CONTRAINDICATIONS
As is the case with the large majority of ankle sprains, appropriate nonoperative treatment can be successful in the majority of acute injuries to the ankle and/or subtalar joint. Nonoperative treatment includes aggressive peroneal strengthening, proprioceptive reeducation. General indications for surgical intervention include
Failure of nonoperative care
Inability to brace (skin/work/dancer)
Recurrent sprains with daily activities (risk for degenerative joint disease (DJD), varus malalignment)
When approaching a lateral ankle ligament reconstruction, it is always important to consider how much soft tissue reconstruction is necessary. Based on the location and degree of subtalar instability, stabilization of the subtalar joint beyond that achieved with a standard Broström may be indicated. It is important to consider whether there is isolated subtalar or combined subtalar-ankle instability and that any procedure stabilizing the subtalar joint may also reduce the joint’s ability to compensate to uneven terrain. A Gould modification to the Broström (augmentation using the extensor retinaculum) may be sufficient if adequate tissue can be found. While there is not currently a rigorous guideline, we will commonly consider augmenting the repair with a split peroneus brevis tendon graft technique in addition to a Broström in appropriate patients when subtalar instability remains despite a satisfactory Broström/Gould repair.
Although it has been demonstrated that the split Evans procedure does not reduce peroneal strength, it can reduce subtalar motion with inversion stress (
19). We therefore do not recommend this procedure in those patients whose performance would be substantially adversely affected by this potential loss of motion, including ballet dancers, gymnasts, and ice skaters.