CHAPTER 1 Knee Arthroscopy: Setup, Diagnosis, Portals, and Approaches
ANATOMY
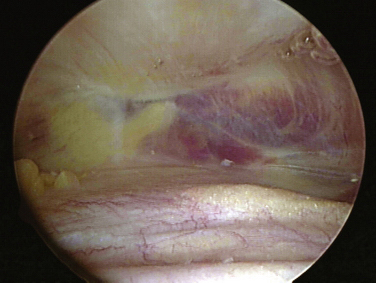
The knee joint, as other joints, is composed of a synovial lining within the capsule. Superior to the patella the synovium extends to form the suprapatellar pouch (Fig. 1-1).1 Superior medial or lateral portals are commonly placed within this pouch. A layer of fat separates the pouch from the distal anterior femoral shaft. The pouch extends medially and laterally along the femoral condyles into the medial and lateral gutters. The suprapatellar pouch and gutters are frequent locations for loose bodies.
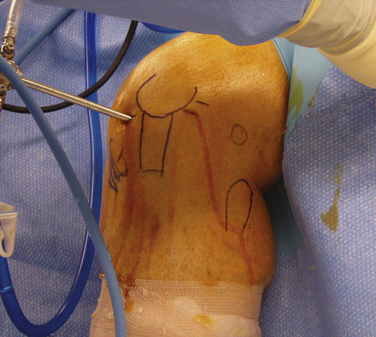
The bony anatomy of the knee relevant to arthroscopic knee surgery includes the distal femur, the proximal tibia, and the patella. With the knee at 60 degrees of flexion, the inferior pole of the patella is located above the lateral joint line and is an important guide for anterolateral portal placement (Fig. 1-2). Exceptions to using this landmark, however, occur in cases of patellar alta, baja, dysplasia, or congenital absence. These conditions should be identified preoperatively with physical examination and standard radiography.

FIGURE 1-2 Photograph of knee showing inferior pole of patella relative to high anterolateral portal placement.
The femoral trochlea consists of medial and lateral trochlear ridges that arise from the corresponding femoral condyle.1 The medial femoral condyle is larger than the lateral from proximal to distal and anterior to posterior. The lateral femoral condyle, however, is wider at the level of the femoral notch. Distally, the femur opens into a notch that contains the femoral origins of the anterior and posterior cruciate ligaments. The notch serves as a target for careful, controlled introduction of cannulas and instruments from anterior portals to avoid injury to articular cartilage (Fig. 1-3). When using the scalpel for anterior portal placement, the blade should be pointed toward the notch but blind insertion beyond the skin and capsule should be avoided, because this would risk injury to the cruciate ligaments.
The medial tibial plateau is larger than the lateral plateau; the two are separated by an intercondylar sulcus or fossa.1 Adjacent to the fossa is a medial and lateral tibial spine that separates the fossa from the corresponding tibial plateau. The femoral condyles and tibial plateaus are incongruous without the medial and lateral menisci. The fibula, although extra-articular, has direct relevance to arthroscopic knee surgery, because it serves as a landmark for portals and surgical approaches. The proximal fibula forms a joint with the proximal posterior surface of the tibia (tibiofibular joint). It also serves as an insertion for the lateral collateral ligament and biceps femoris tendon.
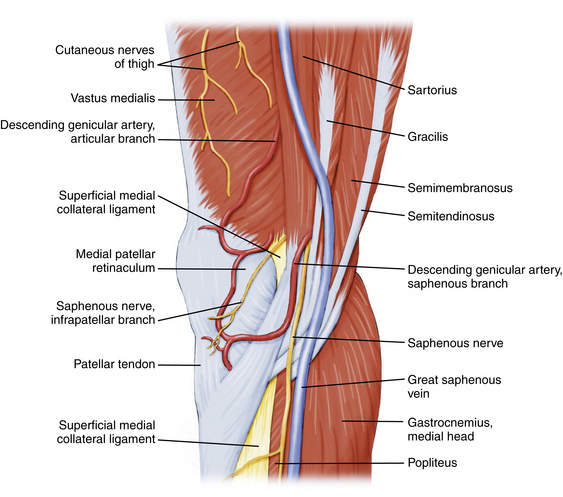
A knowledge of neurovascular anatomy around the knee joint is important for preventing iatrogenic injury during portal placement and surgical approaches.2 Posteriorly, in the midthigh, the sciatic nerve branches into the tibial (or popliteal) and common peroneal nerves. At the posterior joint line of the knee just posterior to the joint capsule, the tibial nerve passes between the two heads of the gastrocnemius muscles, along with the popliteal artery and vein. From medial to lateral, the structures include the nerve, artery, and vein (Fig. 1-4).1 Although Matava and colleagues3 have shown that knee flexion increases the distance between the tibial insertion of the posterior cruciate ligament (PCL) and the popliteal neurovascular structures, other studies have not confirmed this. At 100 degrees of knee flexion, they reported a maximum distance of slightly less than 1 cm between the popliteal artery and PCL insertion.
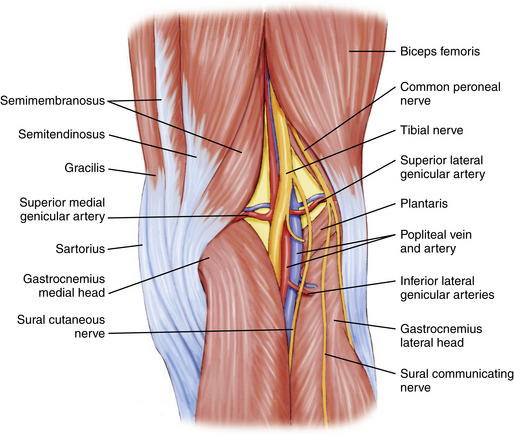
FIGURE 1-4 Posterior aspect of knee showing tibial nerve, popliteal artery, and vein within popliteal fossa.
The common peroneal nerve passes posterior to the biceps femoris tendon and courses between it and the lateral head of the gastrocnemius toward the fibular head (Fig. 1-5).1,2 It then courses laterally around the fibular neck and into the peroneus longus tendon. In most individuals, the biceps femoris tendon insertion onto the fibular head can be palpated in 90 degrees of knee flexion. Placing incisions, portals, and retractors anterior to this landmark will help avoid injury the common peroneal nerve.
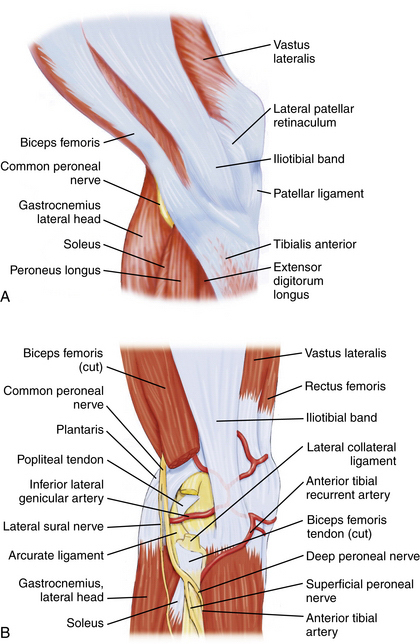
FIGURE 1-5 Lateral aspect of knee. A, Common peroneal nerve passing posterior to biceps femoris tendon. B, Common peroneal nerve passing laterally around the fibular neck.
On the medial aspect of the knee, the saphenous nerve and its infrapatellar branch are at risk for injury during placement of medial and posteromedial portals, as well as during all medial approaches to the knee. The nerve and its branch have a variable course and number of terminal branches.1,2 In general, the saphenous nerve passes between the gracilis and sartorius muscles approximately 3 cm posterior to the medial femoral epicondyle. The infrapatellar branch courses beneath the sartorius (i.e., posterior to it) and runs along the anteromedial aspect of the knee, where it can terminate medially or laterally to the medial border of the patellar tendon (Fig. 1-6).
TREATMENT
Anesthesia Options
Knee arthroscopy can be performed under general, spinal, or local anesthesia. The choice primarily depends on surgeon and patient preference, but in some cases may be influenced by the patient’s medical history. In a prospective randomized study of 400 patients, Jacobson and associates4 compared three anesthesia options and concluded that local anesthesia was technically feasible in 92% of patients undergoing elective knee arthroscopy. However, when comparing patient satisfaction, the local anesthetic group had 90% satisfaction versus 97% for the general anesthesia group. Horlocker and Hebl5 performed an evidence-based review of published studies comparing various anesthetic methods for knee arthroscopy. They reported that the results of most studies were biased by surgeon and patient expectations as well as by differences in postoperative management. They concluded that a single method of anesthesia could not be recommended for all surgeons performing or patients undergoing knee arthroscopy.
Arthroscopic Technique
Operating Room Setup
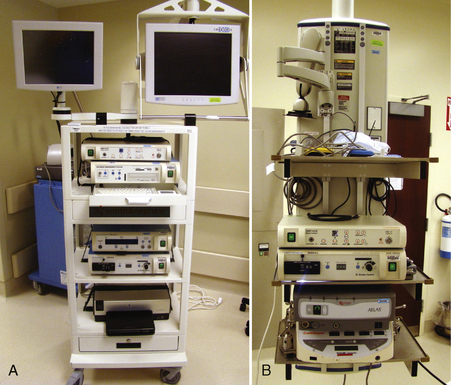
One or more video monitors are required. Traditionally, cathode ray tube (CRT) monitors have been the standard. New flat screen liquid crystal display (LCD) monitors are increasingly being used (Fig. 1-7) and currently most manufacturers of arthroscopic video equipment also offer high definition (HD) monitors. Although only one monitor is needed, many operating rooms use two or more monitors (see Fig. 1-8). Although there is less benefit of multiple monitors for knee arthroscopy, they can be very useful for shoulder and hip arthroscopy.
The control boxes for the arthroscopic camera, shavers, pump, and other devices can be placed on a mobile tower (Fig. 1-8A) that is easily moved from room to room or can be contained on a boom (see Fig. 1-8B). The advantage of the boom is that there are less electrical cords across the floor and that the monitor(s) can be positioned independently of the tower.
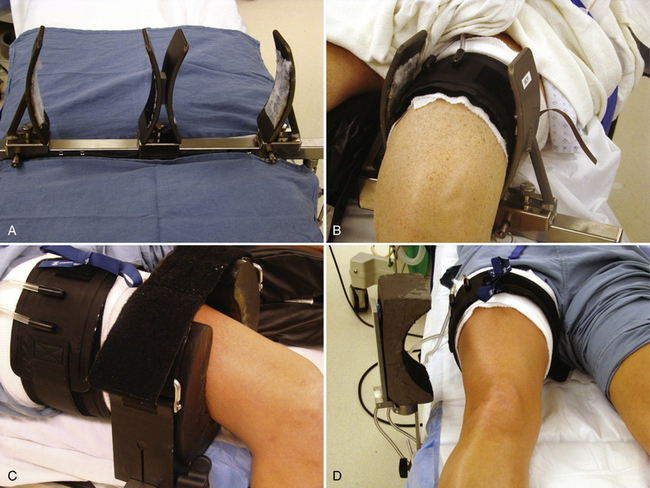
The use of leg holders or posts is determined by the preoperative diagnosis, surgical plan, and surgeon preference. A variety of different commercial leg holders are available for the operative and nonoperative leg. When operating on both knees, bilateral leg holders are also available (Fig. 1-9A). In most cases, a unilateral leg holder (see Fig. 1-9B and C) or lateral post (see Fig. 1-9D) is used for the operative leg. Leg holders may include padding, and some others require you to apply padding to the leg prior to securing it within the holder. Some holders are designed to hold the leg with a tourniquet (see Fig. 1-9B) and others require the tourniquet to be outside the holder (see Fig. 1-9C). If you prefer a unilateral holder or lateral post, it will be important to determine how to protect the contralateral leg. The use of a leg holder for the nonoperative leg has been shown to increase the risk of compression to the peroneal nerve as courses around the fibular neck.2 Nonoperative leg holders can also cause a stretch injury to the femoral nerve if the hip is held extended. If the foot of the bed is left up for a lateral post, then positioning the nonoperative leg does not require anything special. If the foot is dropped, it is often easiest to place a large pad under the nonoperative thigh to keep the hip flexed (Fig. 1-10). If there is concern about pressure on the peroneal nerve, additional foam padding can be applied in this region, particularly in thin patients.
Other issues related to the leg holder include the position of the foot of the bed and the use of hip bumps. For lateral post use, the foot of the bed can remain up (see Fig. 1-9D) or it can be lowered. The advantage of the lateral post is faster setup and positioning, ability to move the leg freely during surgery, ability to hyperflex the knee, and ease of placing the knee in a figure-of-four position. The primary disadvantage is that the leg tends to slide over the post when placing valgus stress on the knee for access to posterior horn of medial meniscus. This can be prevented, however, by having an assistant place downward pressure on the thigh (Fig. 1-11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree