Chapter 5. Investigations
Although laboratory and radiological investigation of orthopaedic patients is helpful, the single most important step in establishing a diagnosis and determining the management of a patient is a properly taken history. The clinical history yields information that no laboratory or computer can provide.
The second most useful step in determining management is clinical examination. Only when a proper history has been taken and a clinical examination performed should investigations be requested. When these results are available they should be interpreted in the context of the patient’s symptoms, job and home circumstances. To rely on investigations alone, without relating them to the patient’s symptoms and individual circumstances, is wrong.
Radiology
Radiographs are essential in orthopaedics, not only to recognize fractures and other bone lesions but also to determine the best way to treat a fracture, the accuracy of reduction and the state of union. Radiographs are so important that it is sometimes forgotten that the bones they show belong to people and it is all too common an error for treatment to be decided on the basis of radiographs alone. Pain and motivation do not show on a radiograph!
Physics of radiology
The visibility of a structure on a radiograph depends upon the atomic weights of its constituent elements. Calcium, with an atomic weight of 40, is easily visible, and so are barium (137) and iodine (127). Fat, water and carbohydrate, which consist of carbon (12), hydrogen (1) and oxygen (16), are hardly visible but the iron (56) of haemoglobin and fascia, which contains sulphur (32) within the collagen molecule, can be seen more clearly. Careful examination of a radiograph will therefore show far more than just bone. The individual muscles and the fascial sheaths around them can be seen, and a fluid level of fat in a joint is a sure indication of an intra-articular fracture (Fig. 5.1). Although it is fair to say that many of the abnormalities visible radiologically can be detected more easily by clinical examination, it is still helpful to recognize a joint effusion on a radiograph and know that it consists of blood rather than synovial fluid.
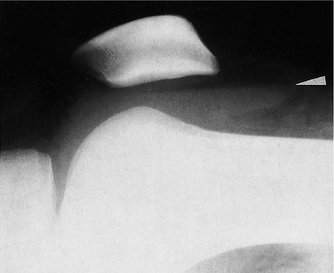 |
| Fig. 5.1 Haemarthrosis of the knee. Note the fluid level, with fat floating on blood, indicating a fracture within the knee. |
Looking at a radiograph
Orthopaedic radiographs must always be taken in at least two planes because lesions can be missed if one shadow is superimposed upon another, particularly with fractures, where one view may show gross displacement while the other is anatomical. When one view is good and one is bad, the worse position is always correct because displacement can never be an artefact (Fig. 5.2).
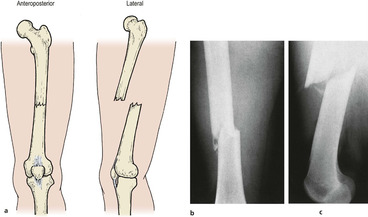 |
| Fig. 5.2 The worst views are always the most accurate: (a) good alignment may be an artefact but bad alignment can never be; (b), (c) radiographs of the same fracture. |
All radiographs are eventually examined by a radiologist, but the orthopaedic surgeon has to make a decision on management before the report is available and must therefore examine the films correctly. This is especially true in the accident department, a place rich in pitfalls for the unwary (Fig. 5.3a and Fig. 5.3b). Undisplaced fractures which are missed always slip when the patient reaches home and impacted fractures never disimpact until the patient has been reassured that he has no broken bones.
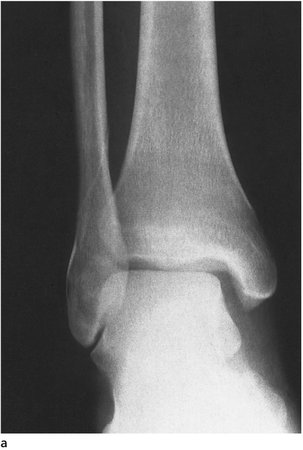 |
| Fig. 5.3a The importance of two projections. Can you see the fracture on this X-ray? See (b). |
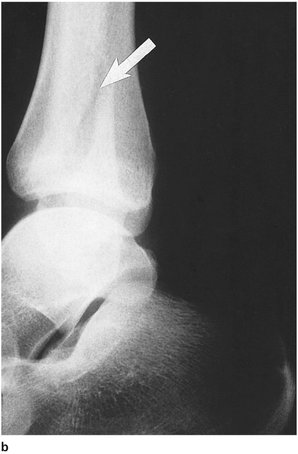 |
| Fig. 5.3b The fracture is in the fibula. |
If treacherous fractures are not to be missed, every cortex of every bone must be examined systematically on every view. It helps to trace around the cortices with a pencil (without marking the film) when doing this. Meticulous examination of each bony detail can, however, lead to something very obvious being missed and it is just as important to stand back and view the radiograph as a whole picture, particularly when a structure such as the spine is being examined.
Although bones are easily seen, soft tissues also cast shadows, but the brightness of the viewing box makes them difficult to see. Because the area of viewing box not covered by the radiograph is very bright, the examiner’s iris constricts and obscures detail in the darker areas. It is surprising how much more of the soft tissues can be seen if the exposed area of the viewing box is masked; try looking down a tube of rolled up radiograph to confirm this.
Special techniques
Tomograms
The X-ray source and plate are moved to produce a blurred radiograph that leaves only one plane or slice of tissue in focus. Tomograms are useful in the investigation of defects deep within a bone, but they have their limitations (Fig. 5.4). To make tomographic cuts less than 1 cm apart is difficult and lesions less than 1 cm in diameter are easily missed. These shortcomings have made the technique almost obsolete but it is important to understand the principles because it is the forerunner of computed tomography (CT), which has largely superseded plain tomography.
 |
| Fig. 5.4 A tomogram showing an area of avascular bone and depressed cortex in a joint. |
Contrast studies
Structures that are not normally seen on a radiograph can be made visible by coating them with a radiopaque material such as iodine or barium, by filling cavities with gas, or both. The use of two materials, gas and a solution opaque to X-rays, is double-contrast radiography and is particularly useful in the investigation of joints, when it becomes double-contrast arthrography.
Radiculography and myelography. Iodine solutions can be injected into the spinal theca to outline the spinal canal and nerve roots stretched over a prolapsed intervertebral disc.
Arthrography. Double-contrast arthrography can outline the menisci and other intra-articular structures with great clarity (Fig. 5.5). A radiopaque medium is injected first, left in the joint long enough to spread over the intra-articular structures, and the joint inflated gently with gas, usually carbon dioxide, to outline the intra-articular surfaces more clearly. Carbon dioxide is used because it is more rapidly absorbed; if air or nitrogen is used the joint can make an unpleasant squelching noise for as long as a week.
 |
| Fig. 5.5 An arthrogram showing a torn meniscus, a deep meniscosynovial sulcus, articular cartilage and bone. |
Although double-contrast arthrography is helpful in outlining solid structures, it is less useful in showing irregularities of joint surfaces or inflammation of soft tissue. Particular applications of double-contrast arthrography are in the investigation of internal derangements of the knee or shoulder and in congenital dislocation of the hip in children.
Discography. Radiopaque medium can be injected into the intervertebral discs to demonstrate lesions in the body of the disc. Apart from making the disc lesions visible, the increase of intradiscal pressure caused by an injection may reproduce the patient’s symptoms and confirm the diagnosis.
Stress radiographs
Joints with doubtful stability can be examined under load to detect abnormal joint laxity and are particularly useful at the ankle and knee if plain films are unhelpful (Fig. 5.6).
 |
| Fig. 5.6 Stress radiographs. Stress is applied to a knee with a ligament rupture. The shadow is the surgeon’s hand in a lead glove. |
Computed tomography
Slight differences between the radiodensities of various elements can be enhanced by computer. If radiographs are made at different angles and in different planes, the computer can integrate the information to produce pictorial ‘slices’ of the body and demonstrate structures not recognizable on a standard radiograph or tomogram. New developments include a ‘three-dimensional’ presentation of the image which displays an entire bone as if it were a shaded drawing (Fig. 5.7). A disadvantage, doubtless soon to be overcome, is an inability to show metal without distorting the rest of the image.
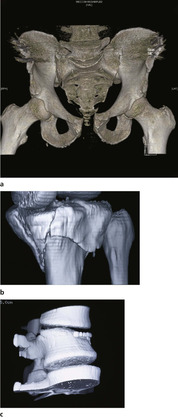 |
| Fig. 5.7 (a) CT 3D reconstruction of pubic diastasis and damage to sacroiliac joint; (b) reconstruction tibial plateau fracture; (c) reconstruction vertebral crush fracture. |
CT has made an enormous impact on the management of soft tissue lesions in the abdomen and central nervous system, including prolapsed intervertebral discs, and is now essential to determine the exact anatomy of complicated spinal and pelvic fractures (Fig. 5.8). CT scans give precise information and reveal spicules of bone that might damage nerve roots or the spinal cord. A practical problem is that CT equipment is so large and cumbersome that severely injured patients and those with multiple fractures cannot easily be examined, and this limits its usefulness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








