Chapter 25. Disorders of the ankle and foot
Ankle
Osteoarthritis of the ankle
Osteoarthritis of the ankle can follow any damage to the joint. The damage may be a single injury such as a fracture, repeated minor trauma, or any other insult to the joint, including infection.
Clinical features
As the degeneration proceeds, osteophytes form on the neck of the talus and obstruct joint movement. Dorsiflexion is usually the first to be affected. The patient gradually becomes aware that they cannot walk comfortably barefoot. This is because the heel of the shoe allows the ankle to be held in slight flexion.
Later, as the osteophytes on the neck of the talus and the anterior lip of the tibia enlarge, the ankle becomes progressively stiffer and it becomes painful to walk, even in normal shoes. At this point the patient will usually seek advice.
Footballer’s ankle
Footballer’s ankle occurs in habitual footballers and is caused by repeated strains of the anterior capsule (Fig. 25.1). Bone gradually builds up at each end of the anterior capsular fibres, producing osteophytes which restrict movement. The condition is indistinguishable from early osteoarthritis.
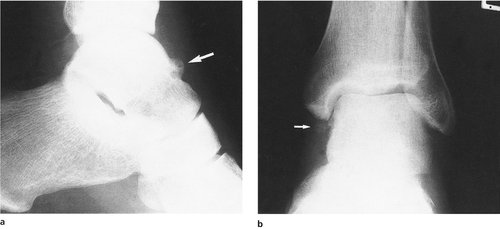 |
| Fig. 25.1 (a), (b) ‘Footballer’s ankle’. Early osteoarthritic change with osteophytes and new bone formation ( arrowed). |
Conservative treatment
There are three forms of conservative treatment:
1. A raise to the heel of the shoe will take pressure off the anterior osteophytes.
2. A normal working boot may reduce the angular forces at the ankle.
3. Anti-inflammatory drugs.
Operative treatment
Operative treatment is seldom required but three procedures are available:
1. Excision of osteophytes and arthroscopic debridement.
2. Arthrodesis.
3. Joint replacement.
Excision of osteophytes from the neck of the talus and the anterior margin of the tibia will improve extension and may relieve symptoms for many years, particularly in footballer’s ankle, but recurrence is likely if the patient continues to play.
Arthrodesis. If pain is severe, arthrodesis may be needed. Arthrodesis of the ankle only abolishes flexion and extension. Inversion and eversion, which occur at the subtalar joint, and supination and pronation, which occur at the midtarsal joint, are unaffected. Rehabilitation after arthrodesis of the ankle is slow, and patients should be warned that it takes 2 years to achieve the final result.
The ankle is usually arthrodesed in slight flexion to accommodate the heel of a normal shoe, although this makes it difficult to walk barefoot. The operation is unsuitable for women who wish to wear heels of a varying height.
Joint replacement is possible, but unsuccessful with present prostheses.
Osteochondritis dissecans and osteochondral fractures
A small fragment of talus may separate from the body as a loose fragment by a similar process to that seen at the knee (p. 326). Osteochondral fractures of the talus also occur (Fig. 25.2).
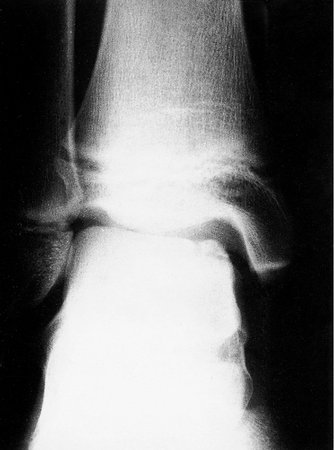 |
| Fig. 25.2 Osteochondritis dissecans of the talus. |
Treatment
If the loose bodies are painful or cause mechanical symptoms then they need to be removed, either arthroscopically or by arthrotomy.
Aseptic necrosis
Aseptic necrosis of the body of the talus may follow fractures through its neck (p. 276). The end result is a loss of height of the talus and a stiff ankle. Left untreated the ankle becomes progressively stiffer but usually becomes painless after a few years. Arthrodesis is not possible because the bone on the talar side of the ankle is dead. Prosthetic replacement is not possible and the disability has to be accepted.
Treatment
There is no active treatment for this condition apart from analgesics and a firm boot to support the ankle.
Rheumatoid arthritis
The bone destruction of rheumatoid arthritis produces a foot and ankle that are unstable as well as painful. Because bone is lost, the ligaments no longer hold the bones in the correct position, the foot rolls into valgus at the subtalar joint and the forces at the ankle produce wear on the lateral side. This in turn leads to a valgus deformity.
Treatment
The unstable valgus ankle of rheumatoid is difficult to manage. Conservative treatment should always be tried before operation. The following measures may help:
1. Ankle supports or surgical footwear to control the deformity, but these are often ineffective.
2. Arthrodesis, which is usually effective despite the poor bone texture.
3. Total ankle replacement, which is less reliable than joint replacement elsewhere.
4. Osteotomy to correct the alignment of the foot and ankle, but the deformity can recur.
Patients with rheumatoid arthritis of the ankle generally have other joints involved as well and the whole problem must be considered.
Ligamentous instability
Damage to the ligaments of the ankle from sprains may make the ankle liable to recurrent episodes of minor instability. The patient may complain that he or she keeps ‘turning the ankle over’ with trivial injury, but clinical and radiological examination are normal. Stress radiographs will demonstrate the opening of the joint and from this pattern the ligaments involved can be deduced.
The lateral collateral ligament, and in particular the anterior talar fibular ligament, is the most common site of injury but the anterior capsule can also be involved.
Treatment
The symptoms can often be relieved by exercises to improve the postural reflexes and strengthen the postural muscles around the ankle. If this is ineffective, operation may be needed to reinforce the lateral side of the ankle by rerouting the peroneus brevis tendon or by a free graft of plantaris. Direct suture methods and shortening of the lateral ligaments can give good results.
Tarsal tunnel syndrome
The medial plantar nerve enters the foot after passing beneath the medial ligament of the ankle, which it shares with the posterior tibial and flexor tendons. The anatomy is comparable with the carpal tunnel at the wrist and the medial plantar nerve is vulnerable to compression by swelling of the tendons or space-occupying lesions such as ganglia. The symptoms of ‘tarsal tunnel syndrome’ include pain and paraesthesia in the distribution of the medial plantar nerve.
Treatment
Decompression of the tunnel is needed only if there is definite proof by electrical studies that the nerve is compressed within the tunnel.
Foot
Subtalar joint
The subtalar joint allows inversion and eversion. Damage to the talus or fractures of the calcaneum can restrict eversion and inversion and make it difficult or painful to walk over rough ground.
Injuries to the subtalar joint commonly result from a fracture of the calcaneum in a fall onto the heel, a common injury in building workers. Ironically, these are the very people who need a good subtalar joint to walk over rough ground.
Treatment
Injuries to the subtalar joint can take at least 2 years to reach their final state and any decision on operation should be deferred until this time has been reached. Until then, support to the ankle and subtalar joint with a firm boot to restrict inversion and eversion will produce some relief and may allow the patient to walk over rough ground.
If the joint is still painful after 2 years, subtalar fusion may be required. Like ankle arthrodesis, it may take 2 years to achieve the final result.
Midtarsal joint
The midtarsal joint lies between the calcaneum proximally and the cuboid and navicular bones distally and, with the tarsometatarsal joint, allows pronation and supination of the forefoot on the hindfoot. Because the subtalar, midtarsal and tarsometatarsal joints are so closely connected, damage to one can impair the function of the other two.
The joint can be damaged by trauma (p. 278), talipes equinovarus (p. 352) and other foot deformities. The result is painful restriction of movement in the foot, detectable on clinical examination (p. 31).
Treatment
Conservative treatment with a firm shoe or boot is often effective, but if pain or deformity cannot be controlled, a triple fusion may be required.
Triple fusion is an arthrodesis of all three joints (talonavicular, calcaneocuboid and subtalar) and converts the tarsus into a solid block of bone (Fig. 25.3). Ankle movement and midtarsal movements are not affected, but inversion and eversion are abolished. The operation is often used as the definitive treatment for the residual deformity of talipes when the patient has reached adult life.
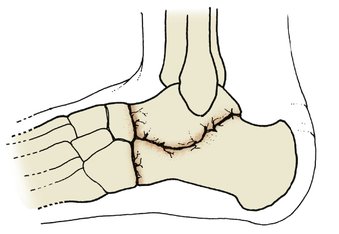 |
| Fig. 25.3 Triple fusion. Three joints are fused – calcaneocuboid, talonavicular and subtalar. |
Pantalar arthrodesis. If the triple fusion is accompanied by an ankle arthrodesis, the operation is known as a pantalar arthrodesis and may be required if the talus has been damaged by trauma or avascular necrosis.
Köhler’s disease
Köhler’s disease is a vascular osteochondritis which causes collapse of the navicular and is comparable with Perthes’ disease at the hip and Kienböck’s disease at the wrist. The joint becomes painful and the affected bone is tender. Radiographs show that the bone becomes dense, collapses and gradually reforms over a period of 2–3 years. The shape of the reformed bone is different from the original, but frequently produces an excellent functional result.
Sever’s disease
Sever’s disease is a traction apophysitis at the insertion of the Achilles tendon comparable with Osgood–Schlatter’s and Sinding Larsen’s diseases at the knee. The condition occurs most often in boys about the age of 12 and causes pain and tenderness at the insertion of the Achilles tendon onto the calcaneum.
Treatment
The symptoms usually resolve within 12 months and no treatment is required apart from a slight raise to the heel of the shoe to take tension off the Achilles tendon.
Achilles tendinitis and paratenonitis
The paratenon around the Achilles tendon may be irritated by repeated friction. The condition is common in athletes.
Treatment
If rest, a raise to the heel and attention to athletic technique do not help, a steroid injection into the space between the tendon and paratenon – but not into the tendon itself – may be helpful.
In very resistant cases the paratenon will need to be freed from the tendon surgically.
Partial rupture of the Achilles tendon
The central fibres of the Achilles tendon sometimes rupture without breaking the continuity of the tendon. In such patients, the ‘squeeze’ test (p. 276) is negative and the tendon will have a tender, fusiform swelling in its midportion.
Treatment
The symptoms usually resolve over 12–18 months and a raise to the heel is helpful. If the symptoms persist after this time, the tendon may need to be explored. A cyst or softened area of tendon will often be found in the centre of the tendon corresponding to the site of the rupture of the original central fibres.
Flexor and peroneal tendonitis
The peroneal and flexor tendons have flexor sheaths and are sometimes affected by tenosynovitis where the tendons run round the corner from the calf into the foot, particularly if there has been trauma to the ankle or subtalar joints.
Treatment
Anti-inflammatory drugs and steroid injection into the tendon sheaths are usually effective.
Recurrent subluxation of the peroneal tendons
The peroneal tendons run in a shallow groove behind the lateral malleolus and may become unstable. If this occurs, the tendons will flick out of their groove and lie in front of the malleolus. The ankle feels unstable and the patient may stumble.
Treatment
Conservative treatment is rarely effective. If the symptoms warrant it the tendons should be stabilized by a bone block to deepen the groove in which they run.









