Introduction
What is osteoarthritis?
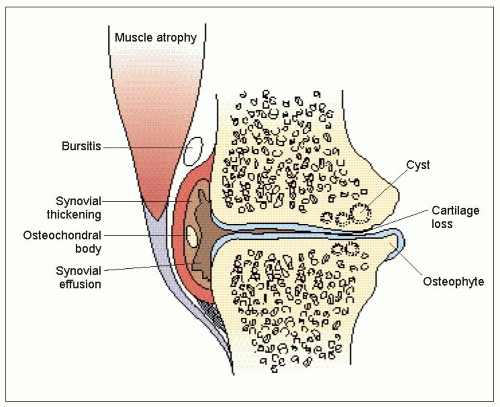
The answer to this apparently simple question is an ongoing problem for a condition that is so common. Everyone seems to be able to recognize ‘osteoarthritis’ when they see it, but, as with many rheumatological conditions, providing clearcut diagnostic criteria has proved more difficult. Notwithstanding problems of definition, it is widely accepted that osteoarthritis is the most common condition to affect synovial joints, and is responsible for a great deal of pain and disability. Although a universally accepted definition has proved elusive, there is general agreement on some of the hallmark features of osteoarthritis. Cartilage loss is universally observed in all patients with osteoarthritis and, as will be discussed further below, is a sine qua non for diagnosis. Cartilage loss tends to be focal rather than widespread throughout the joint, particularly in the early stages of osteoarthritis (1.1).
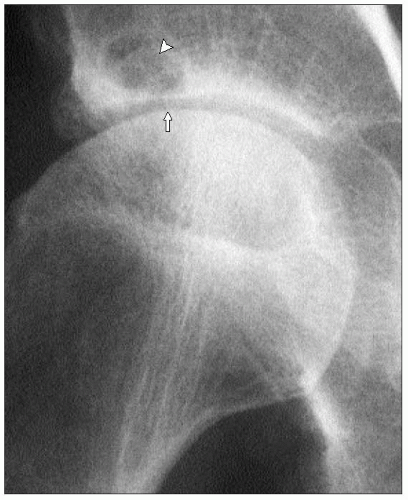 1.1 X-ray of a hip showing focal cartilage loss (joint space narrowing) (arrow) in the superior aspect of the joint. Note also the prominent acetabular cyst (arrowhead). |
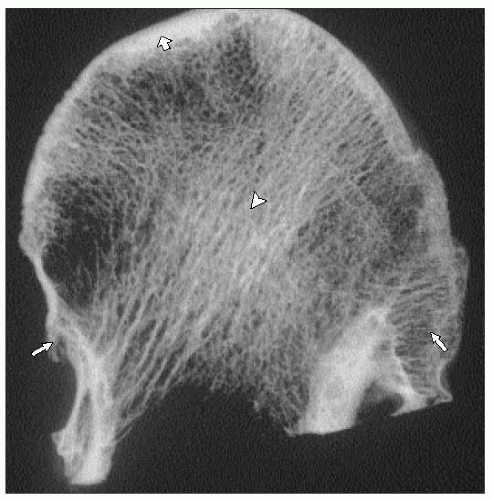
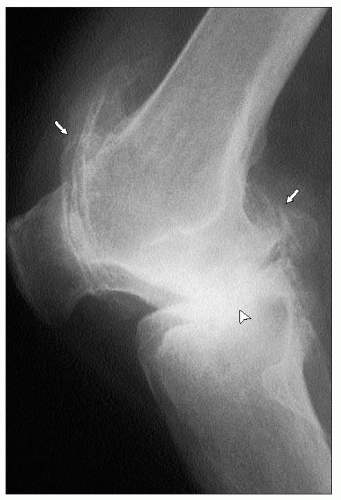
Bone response with increased bone formation adjacent to the joint is also commonly observed although, as discussed later, this varies in prominence at different joint sites and between patients (1.2,1.3,1.4).
Bone response may manifest itself as either as osteophytosis or subchondral bone sclerosis. These two features (i.e. cartilage loss and bone response) have often been considered the main features of osteoarthritis, but, as will be discussed later, it is now clear that many other tissues are involved in osteoarthritis. Indeed, it is likely that these other tissues are more important in determining the symptomatic and functional consequences of osteoarthritis. (Table 1.1, 1.5).
Table 1.1 Tissues involved in osteoarthritis | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The history of osteoarthritis
In order to understand the concept of any disease, it is necessary to look at its historical context. It is likely that osteoarthritis has been present throughout human history. Indeed, it may be of significant evolutionary importance, and this is discussed further below (page 29). The first attempts to describe ‘arthritis’ generally did not distinguish inflammatory from non-inflammatory disease (1.6). Gouty arthritis was probably the first specific arthropathy to be characterized, followed by infective arthritis and rheumatoid disease.
The reduction in infectious diseases as a result of public health measures, and the introduction of effective therapies for inflammatory arthritis, have resulted in an increased awareness and interest in non-fatal, but disabling diseases, such as osteoarthritis. In the 1950s, the introduction of the widespread use of radiography enabled ready study of diseases (such as osteoarthritis) which principally affect bony structures.
The combination of these factors resulted in an increased awareness of the impact of osteoarthritis, and enabled the conduct of large-scale epidemiological studies of this disease.
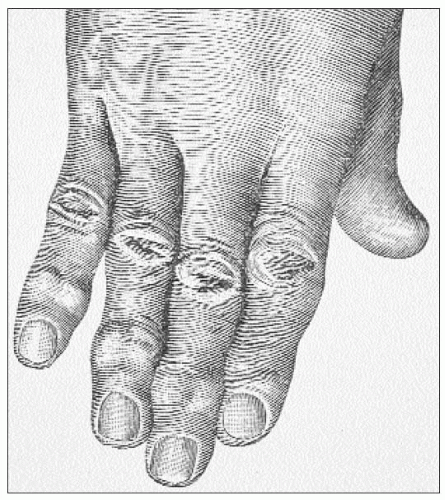 1.6 Nineteenth century drawing of a hand affected by nodal osteoarthritis prior to formal description of the condition (Charcot, Paris). |
The next boost to the study of osteoarthritis came with the development of animal models of osteoarthritis and, in particular, the Pond-Nuki model of osteoarthritis — the anterior cruciate-deficient dog. The importance of this model is that it allowed study of the factors involved in the development of osteoarthritis. This, and other animal models, led to the realization that osteoarthritis is an active metabolic process, rather than a simple eburnation and erosion of cartilage. It also ultimately led to the realization that many other tissues, especially the neuromuscular system, are crucially important in the development of osteoarthritis.
Improved biochemical and cellular techniques further developed interest in the metabolic features of osteoarthritis, although arguably it may have led to an initial undue emphasis on cartilage.
In the 1980s and 1990s, a re-exploration of the epidemiology of osteoarthritis resulted in a renewed appreciation of the fact that not all patients with osteoarthritis are symptomatic. This is an obvious fact to anyone who looks at community samples of osteoarthritis, but can easily be overlooked in an outpatient setting where all patients have been referred because of symptoms. The implications of this has important consequences for understanding the epidemiology of osteoarthritis, and is discussed further below (page 29).
More recent developments in osteoarthritis have followed from the observations of the metabolic activity of osteoarthritis tissues and the realization that these processes may be amenable to modification by pharmaceutical means. This is more fully discussed in the section on disease modification (page 99). It has meant, however, that the pessimistic view that osteoarthritis is inevitably progressive has been challenged, and there is increasing pharmaceutical interest in manipulating this process.
The realization that osteoarthritis is the cause of significant health care expenditure, and that use of these resources may not always be rational, has led to increased health service research in this area, and the development of care pathways and guidelines for the management of osteoarthritis. The principles that have emerged from such endeavours are discussed in Chapter 5.
Finally, it is important not to forget that, in parallel with this, there has been immense interest in surgical interventions for osteoarthritis. These have included osteotomy, arthroplasty with increasingly complex prostheses, and, more recently, arthroscopic approaches, including tissue transplantation.
The epidemiology of osteoarthritis
The epidemiology of osteoarthritis has been elucidated by a number of major cross-sectional studies (pathological, clinical, and/or radiographic). There have also been a number of prospective studies of varying duration which have also illuminated our knowledge. Due to this, a number of risk factors and associations have been identified.
Other species
Osteoarthritis appears to have been present throughout our evolutionary history and, indeed, in many current nonhuman species. Looking across species, it is clear that all animals that fuse epiphyses of synovial joints are capable of developing osteoarthritis. The few often quoted exceptions (e.g. bats and sloths) probably simply reflect lack of study rather than any specific species difference (1.7). This has several important implications. Firstly, it allows potential study of mechanisms of osteoarthritis in non-human, nonprimate species which can thus enhance understanding. Secondly, it probably implies that the biological processes that underlie osteoarthritis are most likely of great evolutionary value to the host organism. This has led some to speculate that osteoarthritis is an aspect of the inherent repair process of the joint, and has led to the coining of the term ‘regenerative’ joint disease.
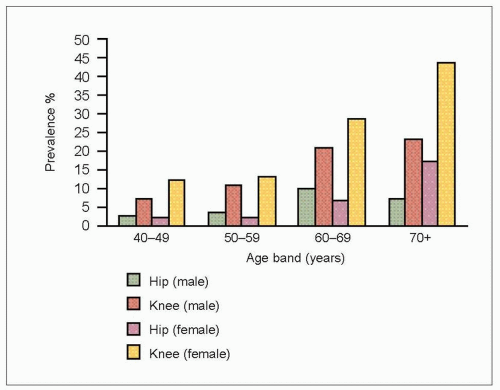
Age
All studies clearly define that the prevalence of osteoarthritis increases with age at nearly all joint sites (1.8). Obviously, since osteoarthritis, once established, demonstrates permanent changes in the joint, some of this could be regarded as the simple accrual of new joint involvement. However, there is a rapid rise in the prevalence of osteoarthritis after the age of 40. This occurs at all synovial joints, although the absolute prevalence varies at different joint sites.
Some forms of osteoarthritis are more likely to develop at specific ages. For example, osteoarthritis of the distal interphalangeal joint is uncommon before the age of 40, but polyarticular onset around the time of the menopause is common with a period of rapid accrual in the decade either side of 50 years of age.
There is a suggestion that the prevalence of osteoarthritis may even decline in the very elderly. These data derive from cross-sectional surveys and, of course, may reflect a survival effect (censureship) in that osteoarthritis may associate with premature cardiovascular mortality.
Gender
A number of studies have demonstrated that the relative prevalence of osteoarthritis at different joint sites differs between genders, usually being more prevalent in women. Both polyarticular osteoarthritis of the distal interphalangeal joints (‘nodal generalized osteoarthritis’) and knee osteoarthritis are more common in women than in men. At other joint sites, this sex difference is less dramatic and may differ with age. For example, hip osteoarthritis is more common in men before retirement age, but becomes more prevalent in women in older age.
Animal studies have confirmed that sex hormones can have a major effect on the development of osteoarthritis. Studies in humans have, however, only hinted at an effect on osteoarthritis, and a therapeutic use for sex hormones has not been demonstrated.
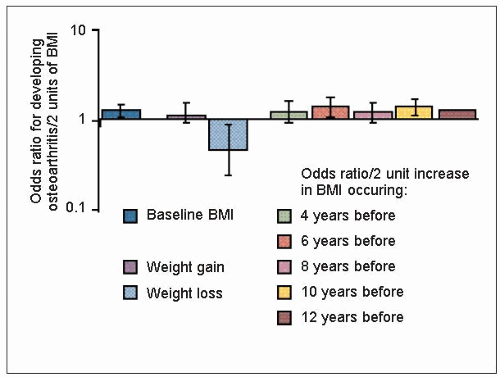
Obesity
At most joint sites, but particularly the knee, weight has an important impact on the development and severity of osteoarthritis (1.9). More importantly reduction of weight in obese and overweight adults has been shown in a prospective observational study to reduce the subsequent development of knee osteoarthritis (1.10).
How obesity and overweight lead to the development of osteoarthritis is not entirely clear. The most likely explanation is mechanical overloading. The support for this comes from a study that has demonstrated that obesity interacts with malalignment at the knee (either varus or valgus) to increase the risk of developing radiographic osteoarthritis.
A counter to the simple mechanical argument is that obesity is acting through a metabolic mechanism. The main support for this proposal relates to hand osteoarthritis. It is argued that hand joints are ‘non-weight bearing’. Therefore, the mechanism of the observed increase in hand osteoarthritis seen in the obese must relate to an associated metabolic imbalance. A number of possible mediating factors have been suggested including insulin-derived growth factor. However, it may not be that straightforward since mechanical studies have shown that forces through the hand joints in the obese are substantially increased.
Trauma
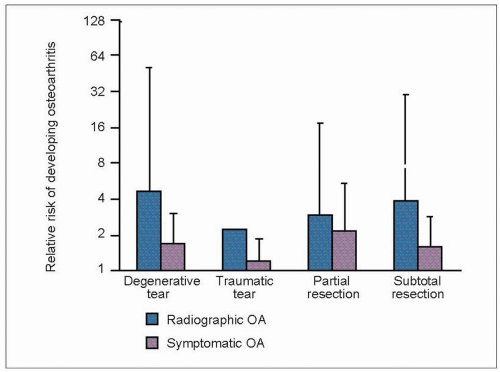
It has long been suspected that severe trauma to a synovial joint might predispose to subsequent osteoarthritis. Support for this comes from clinical observation of patients who have suffered fractures and who subsequently develop osteoarthritis of an adjacent joint (1.11). The risk of such ‘secondary’ osteoarthritis is particularly high when a fracture involves the articular surface of a joint.
Additional evidence comes from follow-up of patients who have undergone meniscectomy at the knee (1.12). Removal of a meniscus is a major mechanical insult to the knee and post-meniscectomy subjects are at increased risk of premature osteoarthritis on the side of the meniscectomy (1.13). The lifetime risk of developing osteoarthritis may not be increased, but the time of onset certainly does seem to be brought forward.
The degree of trauma required to increase the risk of subsequent osteoarthritis is unclear. However, a recent prospective study of college students suggests that even relatively minor trauma, insufficient to lead to hospitalization, is still associated with an increased risk of knee osteoarthritis in young adult life.
 1.12 A longitudinal ‘bucket-handle’ tear of the medial knee meniscus. Tears of the medial meniscus are three times more common than lateral tears. |
Genetic
An important genetic contribution to development of osteoarthritis has been suggested by classic twin and family studies. Strong heritability was first noticed for generalized nodal osteoarthritis, characterized by the presence of multiple Heberden’s nodes. These nodes were described by William Heberden in 1802 in his Commentary on the History and Cure of Disease:
‘What are those little hard knobs, about the size of a small pea, which are frequently seen upon the fingers, particularly a little below the top, near the joint? They have no connection with the gout, being found in persons who never had it; they continue for life; and being hardly ever attended with pain, or disposed to become sores, are rather unsightly, than inconvenient, though they must be some little hindrance to the free use of the fingers.’ (Heberden W [1802]. Commentarii de Morborum Historia et Curatione, London.)
As will be discussed later, this form of osteoarthritis generally has its onset in perimenopausal women, hence its other common name of ‘menopausal arthritis’. It shows strong inheritance, particularly in women, and behaves almost as a sex-linked, autosomal-dominant condition.
Other rare forms of atypical, young-onset osteoarthritis, often with minor degrees of dysplasia, have been described which transmit as monogenic disorders. In some families, the precise genetic association has been identified as mutations of the gene COL2A1 that encodes Type II collagen – the principal structural collagen of hyaline articular cartilage. However, investigation of patients with more common ‘sporadic’ osteoarthritis has failed to find such mutations as a common cause. Such reports in families have, however, fuelled interest in the genetics of more common forms of osteoarthritis.
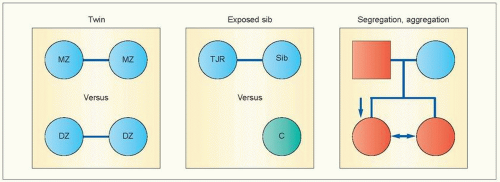
More recent genetic epidemiology studies, using a variety of strategies (1.14), have confirmed an important genetic component to the development of osteoarthritis at a number of sites including the hip, knee, hand, and spine. The heritability of osteoarthritis at these sites (that is, the degree of variance for osteoarthritis in the population that is explained by genetic factors) is estimated to be between 40-60%. Linkage and association studies continue to try to identify the responsible genes (1.15). Although a number of findings are reported, most have not been replicated in subsequent studies. It is clear, however, that osteoarthritis is a common complex disorder, and that several, possibly even multiple genes, will contribute to susceptibility. These are likely to be common polymorphisms rather than mutations; they may vary according to joint site, and they may need to interact with other genes, or with other constitutional or environmental risk factors to express the phenotype of osteoarthritis (1.16).
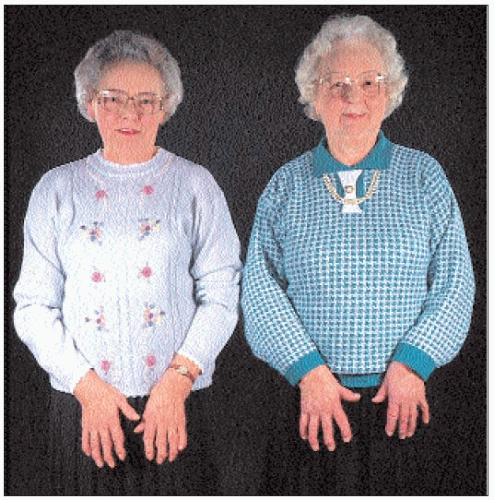 1.15 Two sisters affected by nodal generalized osteoarthritis affecting hands and knees. A sibling of someone who has required joint replacement for knee osteoarthritis is at more than twice the risk of developing knee osteoarthritis than someone without such a ‘genetic exposure’; the risk for a sibling of someone who has undergone joint replacement for hip osteoarthritis is even higher (3-9 fold depending on age and gender). Genetic studies undertaken on multiples families with such affected sibling pairs is the main way of determining linkage between osteoarthritis and specific chromosomal regions. Examination of possible candidate genes within those regions is a common strategy to determine the genes responsible for genetic susceptibility.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|