Subsets of Osteoarthritis
Generalized osteoarthritis
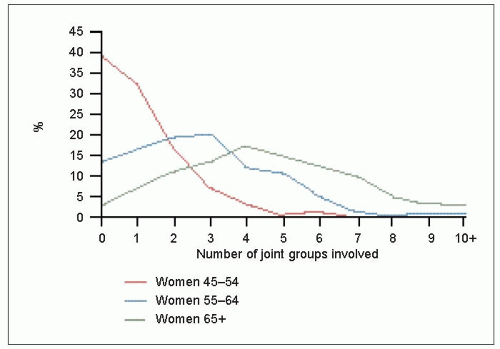
Early epidemiological studies using radiological surveys detailed the fact that many patients had osteoarthritis of multiple joints, suggesting a generalized, in-built predisposition (3.1).
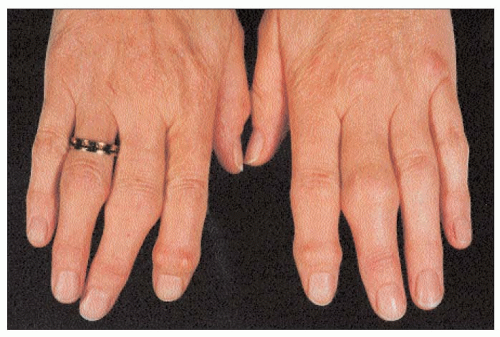
Furthermore, the pattern of joint involvement did not appear random, in that certain joints were commonly affected together. In particular, distal interphalangeal joints, medial tibiofemoral compartments, thumb bases, and intervertebral discs and apophyseal joints of the lumbar and cervical spine seemed to be affected quite commonly in the same patients (3.2). In addition, many patients were noted to have Heberden’s nodes. These occur at the distal interphalangeal joints, and were originally described as ‘pealike swellings’ on the posterolateral (radial and ulnar) aspects of the joint, either side of the extensor tendon. Their early development appears to involve a cystic swelling arising from the synovial cavity of the joint. The cyst contains a gelatinous material which subsequently appears to undergo chondroid metaplasia, and then ossification. Originally, it was unclear if Heberden’s nodes always relate to osteoarthritis, but recent studies suggest that the two are closely related. Similar changes can occur at the proximal interphalangeal joints where they are commonly known as Bouchard’s nodes (3.3).
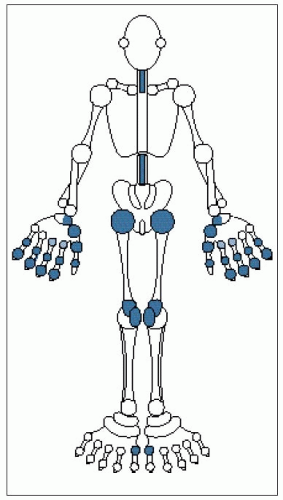 3.2 Distribution of joint involvement in generalized nodal osteoarthritis. Major target joints are shown in dark blue, moderately targeted joints in pale blue. |
While multiple Heberden’s nodes commonly associate with osteoarthritis at other sites, they may also occur in a few fingers without osteoarthritis elsewhere, perhaps reflecting localized hand trauma. However, multiple nodes commonly associate with polyarticular osteoarthritis in women(3.4). The appearance of multiple nodes often occurs around the time of the menopause, and was once known as ‘menopausal arthritis’. It is now more commonly termed ‘generalized nodal osteoarthritis’. It has a strong genetic component with a marked female preponderance, and a high degree of penetrance, behaving almost like a Mendelian recessive trait.
Erosive osteoarthritis
Some patients with polyarticular hand osteoarthritis appear to have a worse prognosis. Clinically, this includes a high degree of interphalangeal joint instability (3.5), a restricted range of movement, and even joint ankylosis. In addition, there is an almost equal involvement of proximal and distal interphalangeal joints, compared to generalized nodal osteoarthritis where the involvement is predominantly distal.
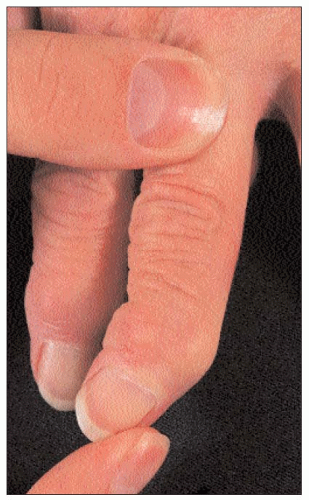 3.5 Marked lateral instability of a distal interphalangeal joint in a patient with ‘erosive’ osteoarthritis. Such instability is not a feature of common nodal osteoarthritis. |
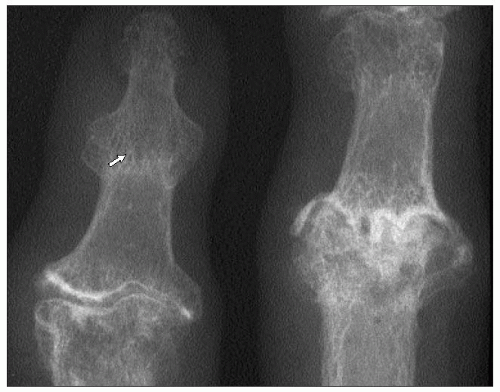
Radiographically, erosive osteoarthritis is characterized by subchondral erosion of bone. This can give rise to a characteristic ‘sea-gull wing’ appearance (3.6). Bone loss can be marked and lead to finger shortening and, hence, joint laxity. In some cases, there can be late bony fusion (3.7). Instability and bony ankylosis are not features of common nodal osteoarthritis.
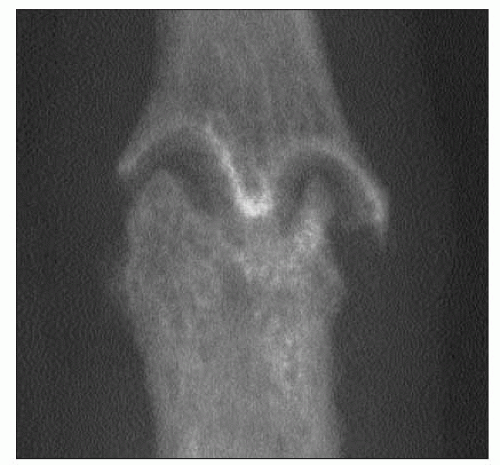 3.6 Erosive osteoarthritis. Marked subchondral erosion leads to scalloping of the bone ends and a ‘gull’s wing’ appearance. |
Pyrophosphate arthropathy
After the nature of gout as a crystal-based arthropathy was elucidated, a group of patients were described in the 1960s with acute self-limiting synovitis of the knee, which clinically resembled gout. However, examination of their aspirated synovial fluid under polarizing light did not reveal the bright, negatively birefringent, needle-shaped crystals of monosodium urate (the gout culprit), but other much smaller, positively birefringent, rhomboid crystals that were chemically identified as calcium pyrophosphate dihydrate (CPPD) crystals (3.8, 3.9). The attacks of acute selflimiting inflammation caused by CPPD crystals were called ‘pseudogout’.
Plain radiographs of some patients can also demonstrate calcification of cartilage (chondrocalcinosis) affecting fibrocartilage and less commonly hyaline cartilage (3.10). Cadaveric and synovial fluid studies have confirmed that usual cause of chondrocalcinosis is CPPD crystal deposition, with other less common causes being apatite and other basic calcium phosphate crystals. Chondrocalcinosis is a common, age-associated radiographic finding that can occur in structurally normal joints. However, there is an increased prevalence of chondrocalcinosis and CPPD crystal deposition in osteoarthritic joints, especially knees, and when they co-exist, the term ‘chronic pyrophosphate arthropathy’ is often used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree