Intramedullary nailing techniques are typically used for closed and open displaced diaphyseal tibial fractures.
The indications for intramedullary nailing can be extended to proximal and distal metaphyseal tibia fractures, including those associated with simple articular involvement.
Both traditional peripatellar and semiextended approaches are used to attain the entry site for nailing all levels of tibial fractures.
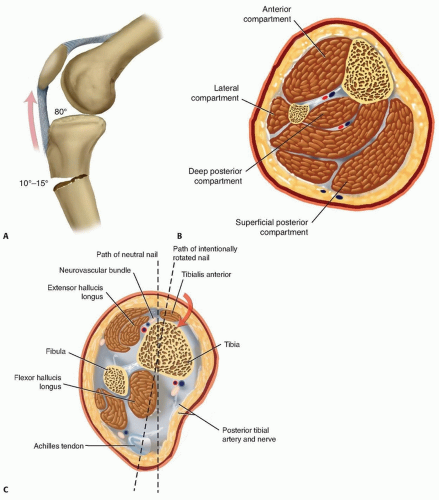
The triangular-shaped proximal tibia is narrowest medially, and the proximal medial cortex tibia is obliquely oriented to the frontal plane. The medullary canal of the tibia exits at the margin of the lateral articular facet. As a result of this complex proximal anatomy, there is less sagittal plane space for an intramedullary nail within the tibia metaphysis with a medial or central insertion path. With a medial start site, the anteromedial metaphyseal cortex can deflect the nail and create a valgus deformation. Due to these factors, a tendency toward a more lateral start site is favored.
The patellar tendon inserts on the tibial tubercle and extends the proximal fracture segment in proximal fracture patterns. This displacement is accentuated with further flexion of the knee, which typically is required to attain the proper starting point for intramedullary nailing (FIG 1A).
Gerdy tubercle—the origin of the anterior compartment muscles and insertion site of the iliotibial band—is palpable along the proximal lateral tibia. In addition to the deforming forces of the patellar tendon, the anterior compartment muscles and the iliotibial band contribute to the shortening and valgus deformity typically seen with more proximal fractures.
The anterior tibial crest corresponds to the vertical lateral surface of the tibia. When it is palpable, it is an excellent reference for the anatomic axis and nail path (FIG 1B).
The anteromedial tibial surface is subcutaneous and often is the site of traumatic open wounds.
The anterior neurovascular bundle and tibialis anterior tendon are at risk with anterior to posterior distal interlocking screw paths; internal rotation of the nail may decrease the risk of iatrogenic nerve injury3 (FIG 1C).
Tibial shaft fractures may occur from high-energy mechanisms of injury, as when a pedestrian is struck by a motor vehicle. Many fractures, however, result from lowenergy mechanisms such as simple falls in elderly patients or those with poor bone quality or sports-related injuries (common in soccer players) in younger patients.6
In this low-energy fracture group, elderly patients are more likely to have comminuted and open fractures due to simple falls.
The long-term outcome of tibial malunion is not clearly defined in the trauma literature.
Knee pain is reported in up to 58% of cases after intramedullary nailing. This pain typically is anterior, associated with activity, and exacerbated by kneeling activities.6, 11
Knee pain improves in about 50% of patients after hardware removal.6
Attempts to detect a correlation between start sites and knee pain have been inconclusive, and comparative evaluations between traditional start sites and semiextended start sites (ie, suprapatellar) are underway.
Understanding the mechanism of injury and the environment in which the injury occurred is important for evaluating a patient’s risk for associated injuries and compartment syndrome. In open fractures, it can help determine the choice of prophylactic antibiotic therapy.
All patients who sustain tibial shaft fractures from highenergy mechanisms should undergo standard advanced trauma and life support (ATLS) protocol to have a thorough examination for life- and other limb-threatening injuries. Seventy-five percent of patients with open tibia fractures have associated injuries.1
To evaluate a patient’s risk for potential complications, other medical conditions should be investigated, including a history of diabetes mellitus, renal disease, inflammatory arthropathies, tobacco use (which increases healing time by up to 40%), and peripheral vascular disease.4
It also is important to find out about the patient’s normal activities and employment requirements to give them a reasonable expectation for when they will be able to resume those activities.
Pain at the fracture site, swelling, and deformity are common findings in patients with tibial shaft fractures.
A thorough examination of the skin is important to avoid missing open fracture wounds.
Evaluation of the soft tissue envelope for abrasions, contusions, and fracture blisters can help determine whether
definitive treatment can be done primarily or if a staged or delayed approach is required.
A detailed neurovascular examination is critical to avoid the devastating complications associated with compartment syndrome, which can occur in both closed and open fractures (see Chap. 53).
Full-length anteroposterior (AP) and lateral plain radiographs are necessary to adequately evaluate the tibia and fibula. Complete orthogonal views of the tibia and fibula help evaluate for concurrent fractures or dislocation and any preexisting deformity or implants.
Orthogonal radiographic views of the knee and ankle are required to rule out articular involvement.
Axial computed tomography (CT) scan can be used for proximal and distal fractures to rule out intra-articular fracture extension.
Nondisplaced fracture lines are common.
Gunshot wounds may merit CT evaluation to rule out intra-articular bullet fragments and intra-articular fracture extension.
Magnetic resonance imaging (MRI) is not useful for most diaphyseal or metadiaphyseal fractures.
Ankle-brachial index (systolic pressure in injured leg below injury divided by systolic pressure of the brachium) after fracture reduction should be used to rule out vascular injuries in severely displaced fractures or fractures with severe soft tissue injury. Values of less than 0.9 may be indicative of vascular injury, requiring further investigation.18
Compartment pressure evaluation with a commercially available handheld single-stick monitor or with a sideported catheter connected to a pressure monitor (using the arterial line setup) is indicated in patients who have severe or increasing swelling and are not able to comply with physical examination and questioning.
Observe for early signs of compartment syndrome in all patients with tibial diaphyseal fractures.
Open fracture does not preclude development of compartment syndrome.
Measure the pressure difference between the diastolic pressure and the intracompartmental pressure—a differential value of less than 30 mm Hg is considered an indication for a four-compartment fasciotomy.17
Nonoperative management is indicated in ambulatory patients for closed and open fractures that do not require flap coverage and that do not present with excessive initial shortening or unacceptable angulation when a cast is applied (FIG 2).
An intact fibula with an axially unstable fracture pattern (ie, short oblique, butterfly fragment, or comminuted) is at risk for shortening and varus deformities and is a relative contraindication to nonoperative management.
A higher rate of malunion and nonunion with nonoperative management is seen in higher energy fractures.2, 9
Initial treatment includes ˜2 weeks of a long-leg splint, then a long-leg cast for 2 to 4 weeks.
When the initial swelling has subsided, the patient is graduated to a patellar tendon or functional brace. Weight bearing is allowed and encouraged.
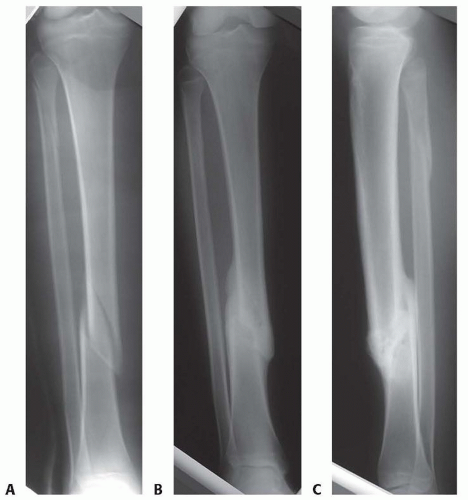
FIG 2 • A-C. An oblique diaphyseal tibial shaft fracture treated nonoperatively to union. (Courtesy of Paul Tornetta III, MD.)
Radiographs are evaluated at 1- to 2-week intervals over the first month of treatment to confirm maintenance of acceptable alignment.
Tibia fractures usually are classified according to the AO Foundation and Orthopaedic Trauma Association (AO/OTA) classification (Table 1).
Several relatively well-accepted indications and contraindications have been established for the intramedullary nailing of tibia fractures (Table 2).
A thorough evaluation of the patient’s soft tissue envelope will determine when the patient can proceed with definitive fixation.
Complete orthogonal radiographs of the entire tibia and fibula are important to determine whether the patient’s intramedullary canal is large enough to accommodate an intramedullary nail (approximately 8 mm) and identify any preexisting deformity that may preclude nail placement. Most modern cannulated nail designs start near 8 mm in diameter. Complete radiographs also identify any proximal or distal articular involvement.
Preoperative measurement of the intramedullary canal and the length of the tibia will help determine which size nail can be used.
The lateral radiograph is the most accurate to use for measuring the appropriate nail length.
Measuring the narrowest diameter of the diaphysis on the AP and lateral views will determine the appropriate nail diameter and whether intramedullary reaming will be necessary.
Table 1 The AO/OTA Classification of Diaphyseal Tibial Fractures
Classification
Description
Illustration
Classification
Description
Illustration
42-A
Simple
42-B3
Fragmented wedge

42-A1
Spiral

42-C
Complex
42-A2
Oblique (≥30 degrees)

42-C1
Spiral

42-A3
Transverse (<30 degrees)
42-C2
Segmented
42-B
Wedge
42-B1
Spiral wedge
42-C3
Irregular

42-B2
Bending wedge

Table 2 Relative Indications and Contraindications for Intramedullary Nailing of Tibial Fractures
Relative indications
High-energy mechanism
Moderate to severe soft tissue injury precluding cast or brace
Angular deformity ≥5 to 10 degrees
Rotational deformity ≥5 to 10 degrees
Shortening >1 cm
Displacement ≥50%
An ipsilateral fibula fracture at the same level
An intact fibula
Compartment syndrome
Ipsilateral femoral fracture
Inability to maintain reduction
Older age, inability to manage with cast or brace
Contraindications
Intramedullary canal diameter <6 mm
Gross contamination of intramedullary canal
Severe soft tissue injury where limb salvage is uncertain
Preexisting deformity precluding nail insertion
Ipsilateral total knee arthroplasty or knee arthrodesis
Significant articular involvement
Previous cruciate ligament reconstruction
Baumgartner M, Tornetta P, eds. Orthopaedic Knowledge Update: Trauma 3. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2005; Schmidt A, Finkemeier CG, Tornetta P. Treatment of closed tibia fractures. In: Tornetta P, ed. Instructional Course Lectures: Trauma. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2006:215-229.
Orthogonal radiographs of the uninjured tibia can be used as templates for determining the appropriate length, alignment, and rotation in comminuted fractures or open fractures with bone loss.
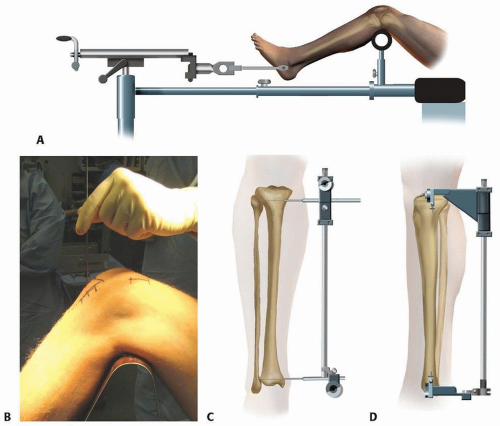
Supine positioning is standard.
A fracture table can be used with boot traction, calcaneal traction, or an arthroscopy leg holder that supports the leg and provides mechanical traction when no assistants are available. However, knee hyperflexion is difficult, and the guidewire insertion angle is suboptimal for proximal fractures16 (FIG 3A).
The patient is placed on the radiolucent table in one of the following positions:
Supine with the leg free (FIG 3B)
Mechanical traction is helpful to achieve reduction when the leg is draped free (FIG 3C,D).
The proximal posterior Schanz pin (FIG 3E) is inserted medial to lateral and parallel to the tibial plateau.
The distal Schanz pin (FIG 3F) is inserted parallel to the plafond and inferior to the projected end of the nail.
Supine with the leg flexed over a bolster or radiolucent triangle (FIG 3G)
Maximizing knee flexion makes it easier to attain a start site and to obtain an optimal insertion vector, which approaches a parallel path with the anterior tibial border.
Semiextended position
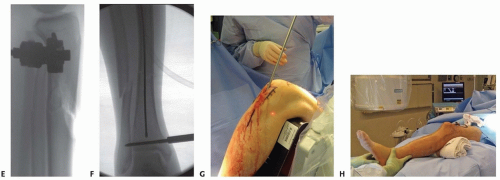
Use fluoroscopy to determine which approach will allow the starting point to be placed just medial to the lateral tibial spine on the AP view and at the anterior articular margin on the lateral view.27 A guidewire can be used to assess the relationship between the anatomic axis of the tibia and the appropriate start site (FIG 4). Externally rotated views are common and can be misleading in selecting the ideal start point.33
For diaphyseal and distal metaphyseal fractures, any of the following approaches are appropriate. As mentioned earlier, the patient’s anatomy and fracture deformity can be used to determine which approach allows for appropriate starting point placement.
Medial parapatellar
Transpatellar tendon (This approach may be avoided by some surgeons due to previous retrospective series that showed an increased likelihood of knee pain with this approach.11, 21 However, other retrospective series and more recent prospective trials have found no association between knee pain and the surgical approach used.)5, 29, 30, 31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree