Intramedullary Fixation of Forearm Shaft Fractures
Charles T. Mehlman
DEFINITION
ANATOMY
The forearm represents a largely nonsynovial, two bone joint with a high-amplitude range of motion (roughly 180 degrees). In the fully supinated anteroposterior (AP) plane, the radius bows naturally out and away from the relatively straight ulna, whereas both bones are predominantly straight in the lateral plane.
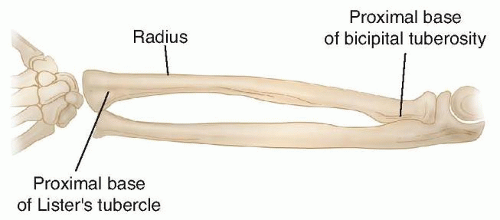
Anatomically, the shaft of the radius extends from the most proximal aspect of the tubercle of Lister (which approximates the distal metaphyseal-diaphyseal junction) to the proximal base of the bicipital tuberosity. The shaft of the ulna corresponds to these same points on the radius (FIG 1).11,13
In unfractured bones, the normal orientation of the radial styloid and bicipital tuberosity is slightly less than 180 degrees from one another, whereas the ulnar styloid and coronoid process come closer to a true 180-degree relationship.
Classically, forearm shaft fractures are divided into distal third (pronator quadratus region), central third (pronator teres region), and proximal third (biceps and supinator region). These anatomic relationships offer insight into the deforming forces acting on the fractured forearm (FIG 2).
PATHOGENESIS
Forearm shaft fractures most commonly occur secondary to a fall on an outstretched arm and usually involve both bones. Forward falls tend to involve a pronated forearm, and backward falls involve a supinated forearm.
Single-bone forearm shaft fractures should raise significant suspicion regarding the presence of a Galeazzi or Monteggia-type injury (see Chap. 11).
Mechanisms of injury that involve little rotational force result in forearm fractures at nearly the same levels, whereas greater rotational force results in fractures at rather different levels.
NATURAL HISTORY
The remodeling potential of the pediatric forearm shaft has been well documented and is considered to be most predictable in children younger than about 8 to 10 years of age.
Spontaneous correction and improvement of malaligned shaft fractures are considered to occur in young children via three mechanisms:
PATIENT HISTORY AND PHYSICAL FINDINGS
The clinician should gather as much pertinent information as possible regarding the mechanism of injury (eg, a fall from the bottom step of the playground sliding board may be much different from a fall from the top step of the same sliding board).
The clinician should determine whether the patient has any other complaints of pain beyond the forearm shaft region (eg, wrist or elbow tenderness). Any perceived deformity or pain to palpation should trigger dedicated radiographs of the problematic region.
The clinician should elicit any past history of fracture or bone disease in the patient or the patient’s family.
Physical examination of the skin of the child’s forearm should be performed to rule out the presence of an open fracture. Any wound, no matter how small or seemingly superficial, should be carefully evaluated. Persistent bleeding or oozing from a small suspicious wound should be considered an open fracture until proven otherwise.
The environment of the injury has special significance for open fracture management. For instance, farm-related injuries may alter the treatment regimen for the patient.
Multiple trauma or high-energy trauma scenarios dictate that a screening orthopaedic examination be performed to help rule out injuries to the other extremities as well as the spine.
Brachial, radial, and ulnar pulses should be palpated, and distal capillary refill should be assessed.
Sensory examination should include, at minimum, light touch sensation testing (or pinprick testing if necessary)
of the autonomous zones of the radial, ulnar, and median nerves. Older children may be able to comply with formal two-point discrimination testing.
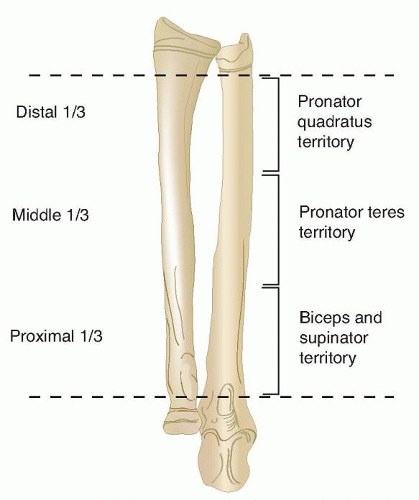
FIG 2 • Forearm shaft fractures are divided into distal third (pronator quadratus region), central third (pronator teres region), and proximal third (biceps and supinator region).
It has been said that you need only a thumb to test the motor function of all three major nerves: radial nerve = extensor pollicis longus, ulnar nerve = adductor pollicis, median nerve = opponens pollicis.
Peripheral nerves in the fractured extremity are assessed with the “rock-paper-scissors” method.
The radial nerve (really the posterior interosseous nerve in the forearm) is tested with “paper”—extension of the fingers and wrist well above a zero-degree wrist position. The autonomous zone is the dorsal web space between the thumb and index finger. There is a risk of iatrogenic injury during surgical exposure of the proximal radial shaft.
The ulnar nerve is tested with “scissors”—adducted thumb, abducted fingers, and flexor digitorum profundus function to ring and pinky. The autonomous zone is palmar tip pinky finger. This is the most common iatrogenic nerve injury after internal fixation of forearm shaft fractures.
The median nerve is tested with “rock.” The autonomous zone is palmar tip index finger. The median is the most commonly injured nerve after closed or open forearm shaft fractures.
The anterior interosseous nerve is tested with the “okay” sign. Flexion of the distal interphalangeal of the index finger and the interphalangeal of the thumb herald flexor digitorum profundus and flexor pollicis longus function of these digits. This is a motor branch only (it has no cutaneous innervation, only articular). Isolated palsy has been reported secondary to constrictive dressings and after proximal ulnar fracture.
IMAGING AND OTHER DIAGNOSTIC STUDIES
AP and lateral radiographs (two orthogonal views) that include the entire radius and ulna are essential for proper diagnosis of forearm shaft fractures in children (FIG 3). If suspicion exists for compromise of the distal or proximal radioulnar joints (Galeazzi or Monteggia injuries), dedicated wrist and elbow radiographs are also indicated.

FIG 3 • AP (A) and lateral (B) radiographs of a boy age 9 years and 11 months with a forearm shaft fracture.
If fracture angulation is noted on both orthogonal forearm views, the true fracture angulation exceeds that measured on either individual view (FIG 4).
The radiographs should be used to classify the forearm fracture in a practical fashion with respect to two bones, three
levels, four fracture patterns (Table 1). This is akin to describing bone tumors in terms of matrix, margins, and so forth.
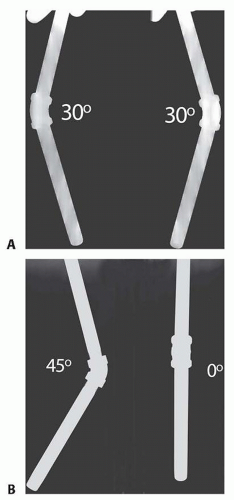
FIG 4 • A. Out-of-plane AP and lateral views of a 45-degree angulated iron pipe. B. True AP and lateral views of the same pipe.
Table 1 Practical Classification of Forearm Shaft Fractures
Bones: Single-bone fractures occur but both-bone injuries predominate.
Radius
Ulna
Level: Fracture level has bearing on nonoperative versus operative decision making.
Distal third
Middle third
Proximal third
Pattern: Fracture pattern has bearing on nonoperative versus operative decision making.
Bow (also known as plastic deformation)
Greenstick
Complete
Comminuted
DIFFERENTIAL DIAGNOSIS
Galeazzi injury (concomitant distal radioulnar joint disruption)
Monteggia injury (concomitant proximal radioulnar joint disruption)
Coexisting distal humeral fracture (eg, supracondylar humeral fracture, also known as floating elbow)
Open fracture (the clinician must be beware of small, innocuous-appearing wounds)
Compartment syndrome (more common in setting of floating elbow and extended efforts at indirect reduction of difficult to reduce fractures)3
NONOPERATIVE MANAGEMENT
Nonoperative (closed) fracture management is used in the vast majority of pediatric forearm shaft fractures.4
Successful nonoperative treatment requires an eclectic mix of anatomic knowledge, skillful application of reduction techniques, appreciation for remodeling potential, and respect for the character of the soft tissue envelope.
Greenstick fracture patterns retain a degree of inherent stability; intentional completion of these fractures is not recommended. Davis and Green7 reported a 10% loss of reduction rate with greenstick fractures and a 25% rate with complete fractures.
Greenstick fracture patterns often involve variable amounts of rotational deformity such that when the forearm is appropriately derotated, reduction of angulation occurs simultaneously.
Apex volar greenstick fractures are considered to represent supination injuries that require a relative degree of pronation to effect reduction.
Apex dorsal greenstick fractures are considered to be pronation injuries that require supination to aid reduction.
Classic finger-trap and traction reduction techniques are probably best reserved for complete both-bone fracture patterns. When dealing with complete both-bone shaft fractures, respect should be paid to the level of the fractures when choosing a relatively neutral, pronated, or supinated forearm position.
Price et al14 has suggested that estimated rotational malalignment should not exceed 45 degrees. The related concepts of maintenance of an appropriate amount of radial bow and interosseous space on the AP radiograph must also not be forgotten, but precise criteria do not exist at this time.
Initial above-elbow cast immobilization is the rule for all forearm shaft fractures, as this appropriately controls pronation-supination as well as obeying the orthopaedic maxim of immobilizing the joints above and below the fracture. An extra benefit of above-elbow immobilization relates to the activity limitation it imposes; in some instances, this may increase the chances of maintaining a satisfactory reduction in an otherwise very active customer.
SURGICAL MANAGEMENT
Flexible intramedullary nail treatment of pediatric forearm shaft fractures focuses predominantly on displaced complete fractures, many of which may have minor comminution (butterfly fragments usually <25% of a shaft diameter).
When efforts at closed fracture management do not achieve and maintain fracture reduction within accepted guidelines, surgical treatment is indicated.
When complete fractures occur in children younger than about 8 to 10 years of age with angulation of at least 20 degrees in the distal third, 15 degrees in the central third, or 10 degrees in the proximal third, risk-benefit discussions are appropriate regarding further efforts at fracture reduction and possible internal fixation.8,17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree