Intramedullary and Dorsal Plate Fixation of Distal Radius Fractures
Nayoung Kim
Fred Liss
Christopher Doumas
Pedro K. Beredjiklian
DEFINITION
Distal radius fractures typically originate in the radial metaphysis and occasionally enter the radiocarpal joint and distal radioulnar joint (DRUJ).
These fractures may be stable or unstable, intra-articular or extra-articular, and have significant incidences of associated bony and soft tissue injuries about the wrist.
Distal radius fractures are most commonly dorsally displaced or angulated (apex volar).
Treatment is based on fracture stability, comminution, articular segment displacement, articular surface displacement, and the functional demand of the patient.
ANATOMY
The distal radius has articulations at the scaphoid fossa, lunate fossa, and sigmoid notch.
The normal bony anatomy includes volar tilt of 10 degrees, radial height of 11 mm, and radial inclination of 22 degrees.
Ulnar variance (the length of the radius relative to the ulnar head at the sigmoid notch) is variable and patient dependent.
Dorsal ligamentous structures include the dorsal intercarpal ligament and the dorsal radiocarpal ligament.
The dorsal radiocarpal ligament originates from the dorsal lip of the radius and attaches on the ulnar carpus.
The dorsal intercarpal ligament represents a capsular thickening on the dorsum of the carpus, of which the fiber alignment is perpendicular to the long axis of the radius.
Volar ligamentous origins include the radioscaphocapitate ligament, the long radiolunate ligament, and the short radiolunate ligament, among others.
The triangular fibrocartilage complex (TFCC) consists of the triangular fibrocartilage and volar radioulnar and dorsal radioulnar ligaments.
The volar radioulnar and dorsal radioulnar ligaments originate from the volar and dorsal edges of the sigmoid notch, respectively, become confluent, and then insert together at the base of the ulnar styloid.
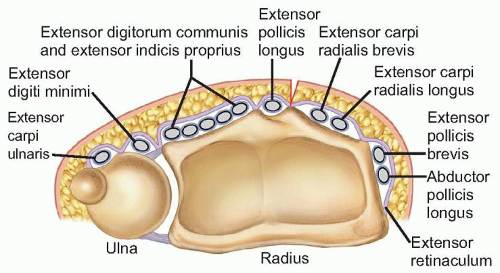
The extensor retinaculum lies superficial to the extensor tendons and deep to the subcutaneous tissues. It has septations creating six dorsal compartments (FIG 1).
The first compartment lies over the radial styloid and contains the abductor pollicis longus and the extensor pollicis brevis tendons (each may have multiple slips).
The second compartment, containing the extensor carpi radialis longus and extensor carpi radialis brevis, lies radial to the tubercle of Lister.
The third compartment, containing the extensor pollicis longus (EPL), lies ulnar to the tubercle of Lister.
The fourth compartment, containing the extensor indicis proprius and extensor digitorum communis, lies over the dorsoulnar distal radius.
The fifth compartment, containing the extensor digiti minimi, lies over the DRUJ.
The sixth compartment, containing the extensor carpi ulnaris, lies over the distal ulna.
PATHOGENESIS
Distal radius fractures typically occur due to a fall on an outstretched hand.
Fractures occur when the force of axial loading exceeds the failure strength of cortical and trabecular bone.14
The fracture pattern is determined by the magnitude and direction of the force applied and the position of the hand during impact.5,13
Dorsally displaced or angulated fractures occur when the wrist is neutral or extended and an axially or dorsally directed force is applied to the carpus.
Osteoporosis, metabolic bone diseases, and bone tumors increase the risk of fracture.
NATURAL HISTORY
Distal radius fractures are either stable or unstable.
Satisfactorily positioned stable fractures, when treated nonoperatively, historically have excellent outcomes in terms of range of motion, pain, strength, and function.1
Nonoperative management consists of immobilization with either a cast or a splint molded to prevent dorsal displacement.
Displaced, unstable, and comminuted fractures often require operative treatment.
The goals of surgical treatment are to provide stability and improve bony alignment in order to achieve pain control, improve range of motion, and increase function.1,8
Two millimeter or more of the articular surface displacement of the distal radius leads to degenerative changes in young adults.8,12
Ten degrees of dorsal tilt (dorsal fracture angulation of 20 or more degrees) is considered unacceptable and may lead to pain, decreased motion, and grip strength.
PATIENT HISTORY AND PHYSICAL FINDINGS
A history of trauma is the most common patient presentation, but pathologic fractures may occur with minimal stress or trauma.
Patients complain of localized pain and present with swelling, decreased range of motion, and ecchymosis about the fracture.
A history of previous fractures in an older patient should alert the physician to the possibility of underlying osteoporosis.
The skin should be carefully examined to rule out the presence of an open fracture and to assess swelling before surgery or casting. If the wrist is markedly swollen or if swelling is anticipated, casting should be delayed and a splint should be placed.
Neurologic symptoms in the form of numbness, tingling, and radiating pain into the digits should alert the physician to the possibility of acute carpal tunnel syndrome (which is considered a surgical emergency). Careful neurologic assessments should be performed to rule out the presence of a progressive neurologic deficit.
If acute carpal tunnel syndrome is suspected, then immediate examination should include the following:
Remove splints and dressings to visualize all areas of skin.
Palpate for areas of tenderness or deformity. Palpate anatomic snuffbox.
Visualize and palpate the elbow for swelling, ecchymosis, tenderness, crepitus, and deformity.
Visualize and palpate the hand and fingers for swelling, ecchymosis, tenderness, crepitus, and deformity.
Use two-point tool or paper clip bent to 5 mm and touch radial and ulnar aspects of all fingers with one or two points. Greater than normal (5 mm) two-point testing in the form of progressive neurologic deficit may signify an acute or chronic carpal tunnel syndrome.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Posteroanterior (PA), lateral, and oblique radiographic views are critical in evaluating all suspected distal radius fractures.
Consider imaging the uninjured wrist for comparison and to serve as a template for surgical reconstruction.
Radiographs of the elbow should be obtained in almost all cases, especially if any tenderness, swelling, or deformity is detected clinically.
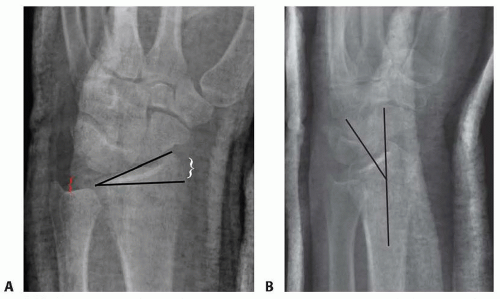
Radial inclination, which is the angle between a line perpendicular to the shaft of the radius at the articular margin and a line along the radial articular margin
Normal angle: 21 degrees
Radial length, which is the distance from a line tangential to the ulnar articular margin to a line drawn perpendicular to the long axis of the radius at the radial styloid tip
Normal length4: 9 to 11 mm
Ulnar variance, which is the distance from a line perpendicular to the long axis of the radius at the sigmoid notch and a line tangential to the ulnar articular surface
Normal length4: 0 mm
Lateral articular (volar) tilt is the angle between a line for the articular surface of the radius and a perpendicular line to the long axis of the radius.
Computed tomography (CT) scans can fully elucidate the anatomy of the fracture, particularly articular disruption or incongruity. They also help to determine the necessary surgical approach by defining the location and extent of comminution.
CT scans increase the interobserver reliability of treatment plans and may actually alter the initial treatment plan based on plain radiographs.7
Axial views provide a clear view of the DRUJ, which aids to identify subluxation, dislocation, bony fragments, and radioulnar ligament avulsions.19
Magnetic resonance imaging (MRI) is used in cases when the presence of a fracture is uncertain.19
MRI can be useful in evaluating for concomitant ligamentous injuries, TFCC injuries, stress fractures, and occult carpal fractures.
DIFFERENTIAL DIAGNOSIS
Bony contusion
Wrist dislocation
Scaphoid or other carpal fracture
Carpal instability or dislocation
Distal ulnar fracture
Wrist ligament or TFCC sprain or tear
NONOPERATIVE MANAGEMENT
Closed reduction can be performed in the emergency department (after hematoma block with 1% plain lidocaine) with longitudinal axial traction followed by volar displacement of the carpus. A bivalved, short-arm, well-molded cast or sugar-tong splint should be applied. It is appropriate to offer patients the option of reduction under intravenous (IV) sedation or general anesthesia.
Casting is the most commonly used method to definitively treat distal radius fractures and is preferred for nondisplaced or minimally displaced fractures and those that are stable after a reduction maneuver (ie, restored volar tilt with minimal dorsal comminution). A precise three-point mold is required to maintain fracture reduction.
Removable splinting can be considered when treating completely nondisplaced stable fractures in young adults.
If nonoperative treatment is chosen, repeat radiographs should be taken on a weekly basis for the first 3 weeks to ensure that the reduction is maintained. The physician should have a low threshold for changing the cast.
Any sign of dorsal migration indicates instability, and operative stabilization should be considered.
Finger range of motion is begun immediately, and wrist range of motion can be started as the fracture heals and is managed in a removable splint.
SURGICAL MANAGEMENT
Open reduction and internal fixation with a dorsal plate can be used successfully in the treatment of displaced, unstable, comminuted fractures of the distal radius that fail to respond to closed treatment.
Dorsal plating buttresses the fracture to correct deformity and maintain fracture reduction.
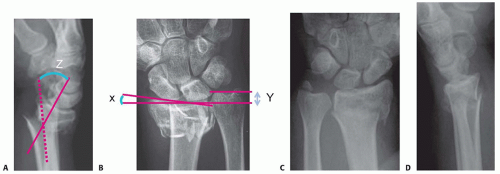
New intramedullary implants have been designed to alleviate some of the complications associated with traditional dorsal plates and allow a less invasive option for fixation of dorsally displaced fractures (FIG 3A,B).
Indications for plating include the following:
Severe initial dorsal displacement (>20 degrees from normal, ≥10 degrees dorsal tilt)10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree