Interposition Arthroplasty of the Elbow
Bernard F. Morrey
INTRODUCTION
There are few areas in orthopedics that have a longer history or are more colorful than the history of interposition arthroplasty (1,2 and 3). This is largely due to the innovative options employed over the years to interpose or to serve as an articular surface. With the ongoing and possibly even increasing requirement to restore function to the destroyed elbow in the younger patient, because total elbow arthroplasty is less reliable as a long-term solution, alternatives must be sought. Interposition arthroplasty today remains the only viable alternative to total elbow arthroplasty for end-stage arthritis in the young patient. In general, we consider this a salvage operation.
INDICATIONS
Any form of arthritis in the younger patient is an indication, that is, a patient under the age of 60 or so (4).
The success of interposition arthroplasty has been documented to be equivalent for both inflammatory and posttraumatic conditions.
In the inflammatory arthritic patient, interposition is offered in those under the age of 40.
Inflammatory arthritis patients over the age of 50, almost always do better with a total elbow unless the elbow is the only or one of the few joints involved.
CONTRAINDICATIONS
An absolute contraindication in the author’s practice is an angular deformity of more than 20 degrees or a dissociation of the forearm relative to the humerus.
In addition, acute or subacute infections are contraindications to this or any definitive reconstructive procedure.
Motor insufficiency especially in flexion is an absolute contraindication to interposition arthroplasty.
Over the years, the relative contraindications to interposition arthroplasty have become very clear: pain at rest and instability (4,5).
Preoperative instability is correlated with postoperative instability.
Patients with interposition arthroplasty with residual instability do poorer than do those in whom the stability is rendered normal or near normal (6).
PREOPERATIVE PLANNING
Patient Characteristics
A history and understanding of expectations are extremely important. The patient should be very clear that interposition arthroplasty is a challenging operation, that the pain relief is not as predictable as that of a total elbow arthroplasty, and that the arc of motion is typically not as good as that which can be realized with a prosthetic joint replacement. On the other hand, this is an operation that allows restoration of function without placing any arbitrary restrictions on the patient’s activity. It should also be very clear to the patient that this procedure, while it can be very successful, can also fail with time (5). When this occurs, the salvage operation may be that of a total elbow arthroplasty (7) or possibly even a repeat interposition. The latter has been shown to be effective in up to 50% of patients (6). The important feature is a clear understanding of these data and communication of those to the patient.
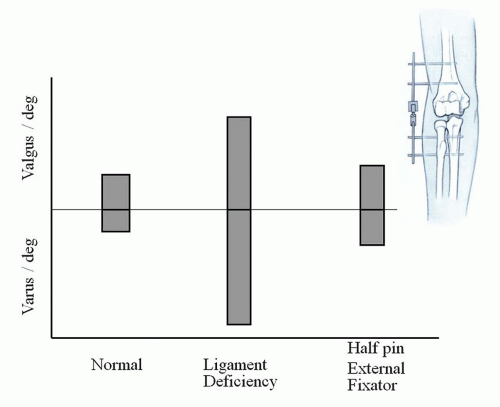
In addition to the communication of expectations, risks, and benefits, the degree of angular deformity and joint line angulation should be assessed. It is not reliable to attempt to correct more than about a 15-degree joint angle since this degree of correction results in so much bone removal that it compromises bone strength. Too much resection may allow progressive resorption of the trochlea. As mentioned under contraindications, the joint stability should be evaluated and an assessment made of whether or not this joint, if unstable preoperatively, has a high likelihood of being rendered stable postoperatively. Since stability is so important, we apply the external fixation in most instances. Data show this device can reliably stabilize joints even with both collateral ligaments detached (8) (Fig. 31-1). In addition, distracting the joint a couple of mm reduces the shear forces on the interposed material while it heals. The interposition tissue is of choice. Today, the most popular are fascia (9,10), cutis (11,12 and 13), and Achilles tendon allograft (5,10). The fascia and cutis autografts have deficiencies of requiring harvesting and cause some problems with the donor site. In addition, the amount of tissue is somewhat limited, and these do not lend themselves naturally toward assisting in the collateral reconstruction. Achilles tendon is preferred by the author because of its excellent clinical track record and because there is adequate tissue to allow not only interposition of the joint but reconstruction of both collateral ligaments if this should be necessary.
SURGICAL TECHNIQUE
The key elements of the surgical technique are shown in Table 31-1.
TABLE 31-1 Key Elements of the Surgical Technique | |
|---|---|
|
Patient Positioning and Exposure
The patient is placed prone with the arm brought across the chest. After the standard prep and drape, a straight posterior incision is made either medial or lateral to the tip of the olecranon (Fig. 31-2).
A previous skin incision should be followed unless the position prompts concern of dermal necrosis. The dissection is carried to the medial aspect of the triceps where the ulnar nerve is always identified and followed to its resting position in the cubital tunnel or to its previously translocated position. Because the technique pivots the ulna on the humerus medially, the ulnar nerve is decompressed at that point, but it may stay in the groove for the moment.
The dissection elevates the flap laterally to the level of the lateral epicondyle (Fig. 31-3). The Kocher interval is entered. The extensor carpi ulnaris is identified and is elevated by sharp dissection from the epicondyle and elevated from the capsule or pseudocapsule if there has been previous surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree