Injuries to the Liver and Spleen
William J. Mileski
INTRODUCTION AND HISTORICAL PERSPECTIVE
The liver and spleen are the most commonly injured abdominal organs.1,2 Few areas of trauma care have evolved so dramatically over the last 4 decades as has the management approaches to hepatic and splenic injuries. The change from early surgery and emphasis on resectional and devascularization techniques to nonoperative approaches has been driven by the understanding that spontaneous hemostasis occurs in at least 50% of patients with injury to the liver or spleen. For example, Walt3 reviewed approximately 1,500 patients with liver injuries from a single trauma center and found that spontaneous hemostasis occurred in more than 50% of the patients. The converse of this concept is that injured patients who are going to bleed sufficiently from the injured liver or spleen to require surgery will manifest their bleeding clinically; the overwhelming majority of the patients requiring surgery will present to the trauma resuscitation area with signs of major blood loss and clinical evidence that the blood loss is intraperitoneal in location. For those patients who are initially stable, the success of nonoperative therapy depends on the knowledge that dangerous bleeding will be detectable in time to perform the necessary surgery before blood loss becomes life threatening.
For patients with liver injury, the conditions for consistently successful nonoperative management have been documented. The main historical reasons for early surgery, control of bleeding, debridement of devitalized liver tissue, and drainage have included fear of infection, bile leak, hemobilia, and late bleeding from hepatic venous injury. Some of these complications do occur but not often enough to threaten the patient’s life while nonoperative therapy is undertaken. Richardson4 described changes in management of liver injury over a 25-year time interval and noted that the use of nonoperative management was associated with improved outcomes in terms of mortality; declines in the rates of septic complications, particularly associated with the cessation of the practice of placing drains; and a reduced frequency of exsanguination from hepatic venous injuries. Walt3 also noted that hepatic venous and retrohepatic vena cava injuries were associated with spontaneous hemostasis. Although management of liver and spleen injuries is predominantly nonoperative, it is critical to remember that the liver and the spleen are both highly vascular, and can be the sources of major abdominal hemorrhage following either blunt or penetrating injuries and may require rapid operative intervention.
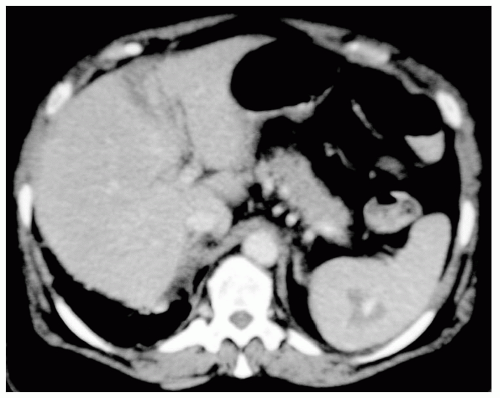
Close observation of hemodynamically stable patients with liver injury is now widely practiced and the success of this approach has been documented.5,6,7 Technologic advances have occurred as clinical experience has increased. Computed tomographic (CT) scans permit visualization of the injury (see Fig. 1) and assist in clinical decision making.8 Although the use of sequential CT scans to document liver healing is intellectually appealing, the utility of this approach has been controversial.9,10 Selective angiographic embolization has become the main means of controlling liver bleeding that occurs during nonoperative management in initially stable patients.11
Success of nonoperative management of liver injury also depends on the recognition that failures of this approach occur.12,13 Successful management of treatment failures depends heavily on recognition of high-risk comorbidities such as liver cirrhosis and severe associated injuries as
well as readily available methods of rapid detection of the need for surgery and the necessary institutional infrastructure such as available surgeons, operating rooms and equipment, radiology services, critical care units, and a responsive blood bank.14,15
well as readily available methods of rapid detection of the need for surgery and the necessary institutional infrastructure such as available surgeons, operating rooms and equipment, radiology services, critical care units, and a responsive blood bank.14,15
The change to mainly nonoperative management of spleen injuries also occurred because surgeons recognized the capacity for spontaneous hemostasis, especially in children.16 Another important influence was the description of serious, sometimes fatal infections in asplenic children.17,18,19,20 Fear of infection stimulated the expansion of nonoperative management to adults.21,22 Inconsistency of patient compliance with vaccination and postsplenectomy antibiotic prophylaxis has provided further impetus to efforts to conserve the injured spleen prompting the development of methods of splenic repair or embolization for preservation of splenic mass.23,24 The actual risk of life-threatening postsplenectomy infection in adults undergoing splenectomy for injury has been difficult to document.25,26 Similarly, the risk of life threatening delayed bleeding has been a controversial topic with some authors concerned that delayed bleeding is underreported.26 Nonetheless, nonoperative therapy for spleen injury in stable children and adults is the most often practiced approach.
MECHANISMS OF INJURY
Blunt trauma due to motor vehicle crashes, auto-pedestrian collisions, falls, and sports injuries is the most common cause of both liver injury and spleen injury and as already noted both types of injury are most frequently managed nonoperatively in hemodynamically normal/stable patients. Penetrating injuries of both the liver and spleen are generally treated surgically to ensure rapid control of bleeding as well as the identification and repair of any associated abdominal injuries.
ANATOMIC CONSIDERATIONS
The potential for exsanguination and death in patients who sustain liver and spleen injuries requires an understanding of anatomy and the emergent maneuvers to allow rapid control of severe hemorrhage.
Liver
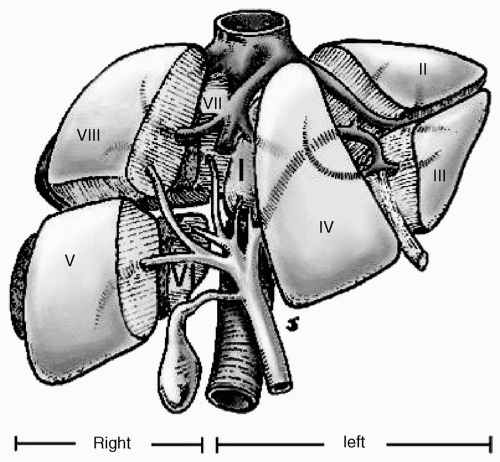
The liver is tethered superiorly by attachments to the diaphragm and the anterior parietal peritoneum through the coronary ligaments, triangular ligaments, and the falciform ligament. Inferiorly the liver is connected to the porta hepatis, including the portal vein, hepatic artery, and common bile duct, and to the lesser curve of the stomach, by the lesser omentum. Posteriorly the liver is connected to the inferior vena cava by numerous very short direct venous branches arising primarily from the caudate lobe. The hepatic veins—superior, middle, and inferior—are located in the central aspect of the coronary ligaments. They are short broad structures that empty directly into the vena cava and require careful attention when mobilizing the coronary ligament. Up to a dozen small venous channels empty into the inferior vena cava from the caudate lobe of the liver. The concept of segmental anatomy of the liver based on the locations of the portal vein branches and the hepatic veins has been eloquently reviewed by Bismuth.27,28 Figure 2 is an illustration of the segmental liver anatomy described in Bismuth’s articles. Liver injury results from compression of the hepatic parenchyma by blunt forces and penetration/cavitation of the parenchyma when penetrating mechanisms occur. Disruption of the liver occurs across segmental boundaries and, when bleeding occurs, multiple arterial and venous branches are involved. Anatomic liver resection is not often feasible for the bleeding patient with liver injury. Nonetheless, knowledge of the locations of inflow and outflow vessels facilitates management.
An important maneuver to achieve immediate control of hepatic hemorrhage is manual compression followed by perihepatic packing. Patients who undergo exploratory laparotomy for liver bleeding have the liver laceration compressed manually as quickly as possible. Then, the spaces above and below the liver are packed with gauze pads. Packing allows for freeing of the surgeon’s hands for additional exploration and hemorrhage control from other injuries. Packing may serve as the definitive means for controlling hemorrhage. Packing and temporary abdominal closure provide time for resuscitation and measures for prevention of coagulopathy and maintenance of body temperature (see the following text).
Another useful maneuver for temporary control of maj or hemorrhage associated with hepatic injures is occlusion of the hepatic artery and portal vein in the porta hepatis (Pringle Maneuver). This can be initially accomplished manually by placement of the index finger of the left hand in the epiploic foramen of Winslow followed by compression of the entire porta between the index finger and thumb. Manual control can be replaced with either a vascular clamp or Rommel tourniquet. Total vascular isolation of the liver is obtained by isolating the infrahepatic inferior vena cava superior to the renal and adrenal veins and inferior to the diaphragm using Rommel tourniquets. Extension of the midline abdominal incision to a median sternotomy may be necessary to gain exposure. On occasion, exposure of the intrapericardial inferior vena cava is the most expeditious method for encircling the vena cava above the liver.
Spleen
The vascular supply of the spleen is composed primarily of the splenic artery and vein and the short gastric vessels. Primary anatomic considerations in treating spleen injuries are related to immediate packing of the left upper quadrant to control ongoing bleeding followed by early control of the short gastric arteries and mobilization of the retroperitoneal attachments of the spleen, the splenocolic, splenorenal, and splenophrenic ligaments. These lateral, posterior, and superior retroperitoneal attachments can be sharply divided with scissors and rapidly released so that a retropancreatic/prenephric plane of dissection can be entered allowing the spleen to be retracted caudally and medially into the midline incision. Caution is required because of the ease of entering the plane between the splenic capsule and the parenchyma of the spleen. Active bleeding can be easily controlled with manual compression of the splenic hilum, or application of vascular clamps to the hilum. If clamps are used it is important to exercise care to avoid injury to the tail of the pancreas, which is always in close proximity to the splenic hilum. Several laparotomy pads can be packed behind the spleen to tamponade bleeding and support the spleen while the lesser sac is opened on the proximal aspect of the greater curve of the stomach and the short gastric vessels ligated. At this point, the spleen can be freely mobilized along with the tail of the pancreas to the midline. Splenic arterial branches and venous branches are individually isolated and controlled with suture ligatures followed by free ligatures.
INITIAL ASSESSMENT
The initial management of all injured patients should follow the principles outlined in the Advanced Trauma Life Support course sponsored by the American College of Surgeons. In patients who are hemodynamically unstable, early identification of intra-abdominal hemorrhage may be obvious based on physical examination but most often is identified by focused abdominal sonogram for trauma (FAST) supplemented, in selected patients, with diagnostic peritoneal lavage (DPL). Under such circumstances the specific identification and management of hepatic and/or splenic injury will occur at the subsequent exploratory laparotomy.
DIAGNOSIS AND SEVERITY GRADING
CT scanning is an increasingly integral part of the assessment of trauma patients and is highly sensitive and specific in the assessment of injuries to the liver and spleen in hemodynamically stable patients. The American Association for the Surgery of Trauma has developed organ injury severity scaling systems, based on CT scan imaging, as well as intraoperative observations that are helpful in making decisions regarding operative management of injuries of the liver and spleen.29,30 Table 1 represents the 1994 revision of the liver injury scale whereas Table 2 is the 1994 revision of the spleen injury scale.
PATIENT SELECTION AND CONDUCT OF NONOPERATIVE MANAGEMENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree