Injuries of the Wrist and Hand
Ethan R. Wiesler MD
Jian Shen MD
Anastasios Papadonikolakis MD
Wrist ligaments are classified as either extrinsic or intrinsic. Extrinsic ligaments connect the forearm bones with the carpus. Intrinsic ligaments originate and insert within the carpus. Extrinsic ligaments are stiffer but have a lower ultimate yield point than the intrinsic ligaments.
There are two main carpal instability patterns: static and dynamic. Static instability is present at rest and can be diagnosed on routine anteroposterior (AP) and lateral radiographs. Dynamic instability requires certain maneuvers to occur with stress; motion fluoroscopy is often required for diagnosis.
Scapholunate (S-L) instability is the most common form of carpal instability. Two ligaments out of interosseous S-L ligament, the dorsal S-L ligament and the volar radioscapholunate ligament, must be disrupted for dissociation to occur.
Injuries to the ligaments and other supporting structures in the thumb offer results in joint instability.
The periscaphoid area is the site of 95% of all wrist degenerative diseases. Scapholunate advanced collapse (SLAC) of the wrist is the most common pattern of degenerative arthritis in the wrist.
The extrinsic flexors of the finger consist of the flexor digitorum profundus (FDP) and the flexor digitorum superficialis (FDS). The FDP originates from the proximal ulna and interossesus membrane; and then divides into two muscle groups in the forearm, the most radial part supplying the index finger and the ulnar part supplying the middle, ring, and little fingers. The FDS has two heads: the radial head originates from the proximal shaft of the radius and the humeral ulnar head originates from the medial epicondyle of the humerus and the coronoid process of the ulna.
The most common complication following flexor tendon surgery is the formation of adhesions, which may occur in spite of appropriate therapy and a compliant patient. Tenolysis should be considered when active flexion is restricted despite a normal passive range of motion, in a wound that has reached soft-tissue equilibrium (usually more than 3 months since repair).
Fractures of the distal radius are the most common of all skeletal injuries. These fractions, which are the most frequent type of bone injury in the upper extremity, occur in athletes of all ages. Distal radius injuries in the athlete typically occur secondary to high energy and are encounted most often in impact sports, but they can occur in any activity where falling onto an outstretched hand is possible.
Carpal scaphoid fractures are the most common and yet problematic fractures of the wrists of athletes. The pattern of scaphoid fractures depends on the force and position of the wrist. The most common mechanism of scaphoid fractures is a fall on an outstretched hand with the wrist in extension and the forearm in pronation.
Fracture of the hamate usually occurs at the hook and is most common in stick- or racquet-handling sports, such as golf, baseball, or tennis. The hook of the hamate is the site of origin for the hypothenar muscles, pisohamate ligaments, and the distal attachment of the transverse ligament.
Fractures of the thumb metacarpal occur most frequently at the base and are subdivided into intra-articular and extra-articular types. Extra-articular fractures occur in transverse and oblique fracture patterns and can be managed without surgery.
Most metacarpal fractures occur in adolescents and young adults from sports or industrial accidents. Fractures of the metacarpals and phalanges comprise approximately 10% of all fractures and 30% to 40% of all hand fractures.
Phalangeal fractures are a common injury affecting all age groups and they are among the most common in all sports. Most phalangeal fractures are caused by direct blows and result in transverse fractures. Distal phalanx fractures are most often caused by crushing forces that lead to comminuted fracture patterns and are frequently accompanied by nailbed lacerations.
Ganglion cyst is the most common soft-tissue lesion of the hand and wrist. Ganglions have been reported at almost every joint in the hand and wrist. The most common location is the dorsum of the wrist. Cyst lining is usually a bland, fibrous, relatively acellular membrane with compressed collagen fibers.
Nerve injuries in athletes are usually the result of chronic overuse or overload, although they may result from acute compression. Chronic overuse injuries are mainly dependent on the sport and biomechanical loading related to the activity. Fractures, compartment syndromes, or blunt trauma may result in acute compression nerve syndromes.
While many sports injuries occur to the lower extremity, the use of the upper extremity for many sports places the wrist and hand in an extremely vulnerable position. Knowledge of both basic science of the structures at risk, and common injuries and their treatment will be outlined in this chapter.
There are multiple anatomic variations in ligament shape and size (1) (Fig 24-1). This explains the existence of so many different descriptions of carpal ligaments in the orthopedic literature (2,3). Wrist ligaments are classified as either extrinsic or intrinsic (4). Extrinsic ligaments connect the forearm bones with the carpus. Intrinsic ligaments originate and insert within the carpus. The existing literature indicates that the extrinsic ligaments are stiffer but have lower ultimate yield point than the intrinsic ligaments (5). The extrinsic ligaments usually rupture mid-substance but the intrinsic ligaments appear to more typically avulse from their osseous origins and insertions than rupture (6).
Extrinsic Ligaments
Superficial Extrinsic Radiocarpal Ligaments: The most lateral superficial ligaments are the radioscaphoid (RS), radiocapitate (RC), and long radiolunate (long RL) ligament (7). The dorsal extrinsic radiocarpal ligamentous complex is formed by the dorsal radiotriquetral (RTq) ligament.
Superficial Extrinsic Ulnocarpal Ligaments: The ulnocapitate (UC) ligament, which inserts into the neck of the capitate (8), forms this complex.
 Fig 24-1. Schematic representation of the most consistently present wrist ligaments. These drawings do not aim to replicate the exact shape and dimensions of the actual ligaments, nor their frequent anatomic variations. A: Palmar superficial ligaments: (1) radioscaphoid, (2) radiocapitate, (3) long radiolunate, (4) lunocapitate, (5) scaphocapitate, (6) pisohamate, and (7) flexor retinaculum or transverse carpal ligament. B: Palmar deep ligaments: (8) short radiolunate; (9) ulnolunate; (10) ulnotriquetral; (11) palmar scapholunate, (12) palmar lunotriquetral, (13) triquetral-hamate-capitate, also known as the ulnar limb of the arcuate ligament; (14) dorsolateral scaphotrapezial; and (15) palmar transverse interosseous ligaments of the distal row. C: Dorsal ligaments: (16) radiotriquetral; (17) triquetrum-scaphoid-trapezium-trapezoid, also known as the dorsal intercarpal ligament; (18) dorsal scapholunate; (19) dorsal lunotriquetral; and (20) dorsal transverse interosseous ligaments of the distal row. |
Deep Extrinsic Radiocarpal Ligaments: This complex is made up of the short radiolunate (short RL) ligament and the radioscapholunate ligament.
Deep Extrinsic Ulnocarpal Ligaments: The ulnotriquetral (UTq) and the ulnolunate (UL) form this complex.
Intrinsic Ligaments
These ligaments connect the bones of the proximal and distal carpal bones or link the two rows to each other.
S-L Interosseous Ligaments: Is formed by three distinct structures: two SL ligaments (palmar and dorsal) and the proximal fibrocartilaginous membrane.
Lunotriquetral Interosseous Ligaments: Two interosseous ligaments (palmar and dorsal) formed by stout transverse fibers connecting the palmar and dorsal aspects of the two bones (9).
Distal Carpal Row Interosseous Ligaments: These ligaments connect transversely the distal carpal row bones and they are classified into dorsal, palmar, or deep intra-articular (10).
1-Dorsal Intercarpal Ligament: It arises from the dorsal ridge of the triquetrum and fans out to insert on the dorsal rim of the scaphoid, the trapezium, and the trapezoid bones (11).
2-Palmar Intercarpal Ligaments: Medially, the triquetral-hamate-capitate (TqHC) ligamentous complex. And laterally, the anteromedial scaphocapitate (SC) ligament and the dorsolateral scaphotrapeziotrapezoid (STT) ligament (12) form this complex.
Neither true radial nor ulnar collateral ligaments of the wrist exist.
Carpal Instability
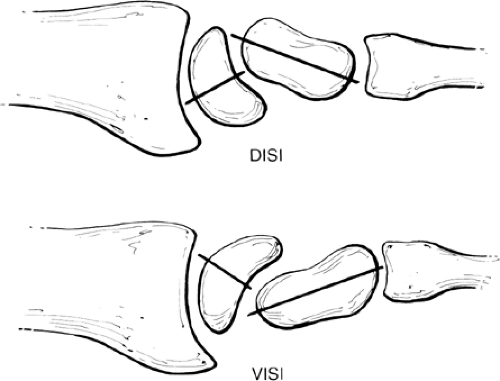
Carpal instability is defined as the inability to bear physiologic loads without losing the normal carpal alignment (13). There are two main carpal instability patterns: static and dynamic. Static instability is present at rest and can be diagnosed on routine AP and lateral radiographs. Dynamic instability requires certain maneuvers to occur with stress, and motion fluoroscopy is often required for diagnosis. Larsen et al. (14) has classified wrist instability into acute (<1 week, maximum primary healing potential), subacute (1 to 6 weeks, some healing potential), and chronic (>6 weeks, little primary healing potential). Most instability patterns can be identified on the lateral radiograph. In the normal wrist in the neutral position, the axes of the radius, the lunate, and the capitate co-align. Dorsal intercalary segmental instability (DISI) is present when the lunate lies palmar to the capitate but is flexed dorsally (Fig 24-2). Volar intercalary segmental instability (VISI) is present if the lunate lies dorsal to the capitate and is palmar flexed (Fig 24-2). Either of these collapsed patterns can be associated with carpal instabilities.
Scapholunate Instability
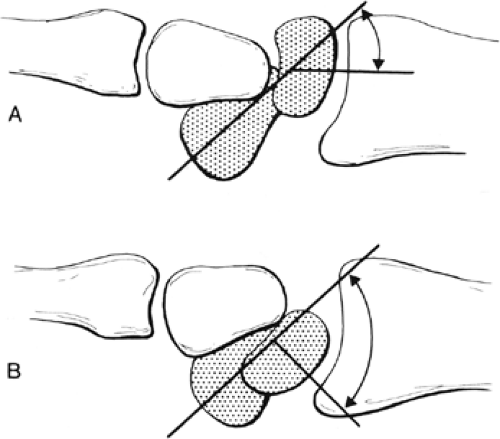
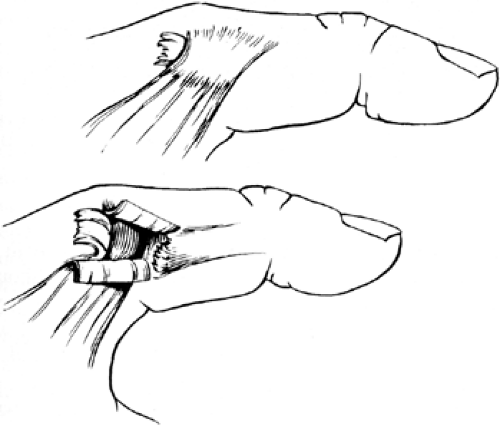
Scapholunate (S-L) instability is the most common form of carpal instability. Diagnosis can be challenging due to the subtle findings in this entity. Three ligaments are involved in this condition: the interosseous S-L ligament, the dorsal S-L ligament, and the volar radioscapholunate ligament. Two of the three ligaments must be disrupted for dissociation to occur. It is generally thought that the volar radioscapholunate ligament must be disrupted before complete subluxation can occur (15). The mechanism of injury usually involves a fall or direct blow that causes hyperextension of the wrist. Pain, swelling, and tenderness are noted over the dorsoradial aspect of the wrist. Watson and Hempton (16) described a diagnostic test in which the examiner stabilizes the scaphoid by placing his or her thumb over the volar pole of the scaphoid while the wrist is held in ulnar deviation. When the wrist is brought into radial deviation, pain is produced as the force is transmitted to the injured S-L ligaments (Fig 24-3).
Radiograph Findings
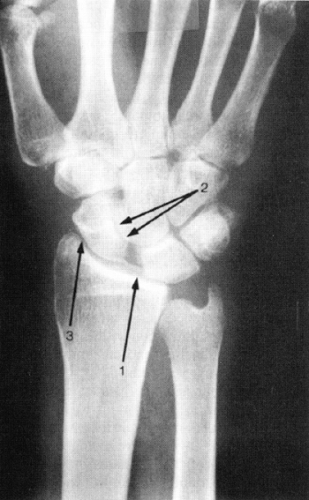
An AP view in full supination may demonstrate widening of the S-L interval. A gap of more than 2 mm is abnormal and should be compared to the contralateral side, provided it is uninjured. The scaphoid will be shortened and a ring sign may be present, which presents the cortical projection of the distal pole of the scaphoid in its more flexed position (Fig 24-4). On the lateral radiograph, a S-L angle of more than 70 degrees (normal range from 30 to 60 degrees) is also suggestive of S-L dissociation (Fig 24-5). Bone scans, arthrography, and, more recently, magnetic resonance imaging (MRI) can be helpful in localizing the area of injury (17).
Management
Injuries diagnosed within 3 weeks are considered acute (18). Cast immobilization with the wrist in full supination, mild dorsiflexion, and ulnar deviation is recommended (19). Closed reduction and cast immobilization for 6 to 10 weeks may allow healing. In complete tears, it is
difficult to obtain a satisfactory reduction by closed means.
difficult to obtain a satisfactory reduction by closed means.
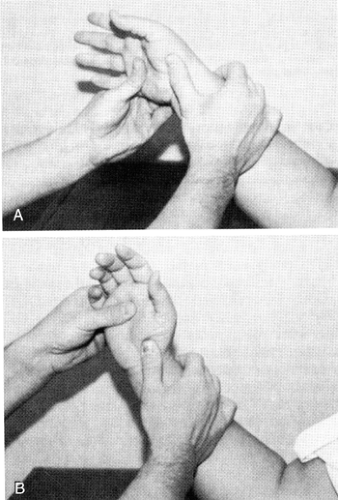 Fig 24-3. The Watson test for scapholunate instability. A: The scaphoid is stabilized with the thumb over the volar pole. B: When the hand is brought from ulnar to radial deviation, pain results. |
Closed reduction and percutaneous pinning in which the wrist is maintained in dorsiflexion to reduce the proximal pole of the scaphoid while the S-L joint is pinned may be successful. A Kirschner wire (K-wire) is passed percutaneously through the snuffbox and across the S-L joint. The wrist should then be gently palmar-flexed to approximate the volar ligaments. A K-wire is then passed across the scaphoid into the capitate for final stabilization. The wires can be removed after 6 to 8 weeks. A protective splint is used for another 4 weeks. Open reduction internal fixation (ORIF) of the S-L joint through a dorsal approach with direct repair of the ligament can be successful, especially if done in the acute period (20). Newer techniques based on improved understanding of carpal kinematics are being developed, but in all cases outcomes are proportional to the severity of injury and the early recognition of the injury pattern. Other treatment options for acute open repair of the injured S-L ligament, with direct repair or ligamentous reconstruction, is generally indicated.
Chronic instability is defined as an injury that has lasted longer than 3 months. There is no reliable procedure for treatment of chronic injuries. Some use a dorsal capsulodesis technique in which the dorsal capsule acts as a check rein to prevent palmar rotation of the distal pole of the scaphoid (21). Others have used various tendon grafts to reconstruct the S-L ligament or the radioscapholunate ligament (15,22).
A variety of intercarpal arthrodeses have been proposed. In S-L joint arthrodesis, it is difficult to attain successful fusion. There is currently no accepted means to achieve successful SL fusion, due to the high stresses imparted to this joint; nonunion rates are unacceptably high in the reported literature. The capitate can be included in the S-L arthrodesis to increase success rate in attaining solid fusion. This, however, is at the cost of loss of wrist motion (23), primarily palmar flexion. Triscaphe (trapezium-trapezoid-scaphoid, S-T-T) fusion (16) is a demanding technique; however, it prevents subluxation of the proximal pole. Although bony S-L arthrodesis may not occur, a fibrous union does occur to prevent capitate migration. Including the capitate in the fusion increases the chances of obtaining a bony fusion but results in restriction of motion. The scapho-trapezial-trapezoid arthrodesis described by Peterson and Lipscomb (24) may increase the stress on other joints, especially the RS joint.
It is the authors’ opinion that acute repair of the S-L ligament should be performed within the first 3 months. This may be done with tissue augmentation from the extensor or flexor tendons, or with a capsulodesis. After 3 months, especially in the case of significant static carpal instability, other options such as, but not limited to, those mentioned above should be performed to prevent the 9 to 12 year gradual progression to SLAC.
Medial (Ulnar) Carpal Instability
With medial (ulnar) carpal instability, patients present with wrist pain and often have a painful click, which may be audible or palpable. Often the patient does not recall a specific injury episode.
Triquetrohamate Instability
Triquetrohamate dissociation is the most common ulnar instability. The patients usually have a characteristic “clunk,” which maybe audible and/or palpable as produced by active motion. This clunk represents the triquetrum suddenly snapping back and forth over the lunate articulation with ulnar and radial deviation. Physical examination may elicit tenderness over the triquetrum. Plain radiographs are usually not helpful. Fluoroscopy is useful and sufficiently demonstrates abnormal motion (25). The lunate can be seen to snap suddenly when the triquetrum reduces on the lunate.
Lunotriquetral Instability
With lunotriquetral instability, patients may or may not have a wrist click on examination. For diagnostic purpose, a ballottement test (Fig 24-6) has been described (9) in which the lunate is stabilized by one hand while the other hand shifts the triquetrum in a palmar and dorsal direction. This reproduces the same pain that the patient is experiencing. Plain radiographs are not helpful. Fluoroscopy is usually normal.
Treatment includes a trial of conservative measures consisting of immobilization in a cast or a splint and an anti-inflammatory medication. From our own experience, local steroid injection into the joint can be helpful. Athletes who are mostly symptomatic during game activity can be fitted with a splint to correct triquetrohamate instability (26). This splint reduces the VISI sag of the proximal row by pushing dorsally on the pisiform. Surgery can be considered in those who fail conservative treatment. The triquetrohamate and lunotriquetral joints are first inspected, and then the wrist is stressed by axial compression and side deviation to confirm the location of the instability. The triquetrum is then reduced and fixed internally by inserting K-wires across the involved joint. The joint space is filled with cancellous bone graft to maintain the joint space. The wrist is then immobilized for 6 to 8 weeks in a short-arm cast, after which the pins are removed and a rehabilitation program is started. This joint has had more success than the S-L joint in arthrodesis in the literature. Consideration for arthroscopic debridement in mild cases with partial limited intercarpal (L-T) tears should be the first step in treatment; L-T fusion is an option in advanced cases of ligamentous instability.
Thumb Metacarpophalangeal Joint Instability
The human thumb plays a central role in almost all hand functions. Injuries to the ligaments and other supporting structures in the thumb often result in instability.
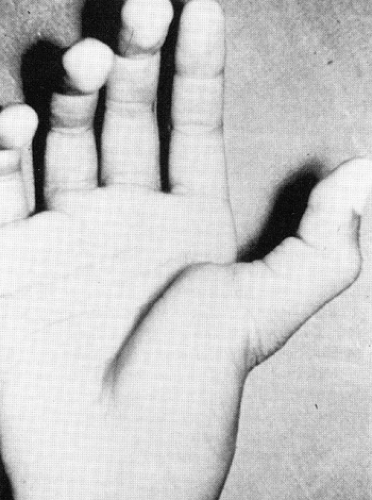
The most common thumb metacarpophalangeal (MCP) joint dislocation is dorsal dislocation (Fig 24-7). The mechanism is usually a hyperextension injury. The condition of the volar plate will determine if a dislocation is easily reducible or if it will require open reduction.
Volar dislocation of the thumb MCP joint is encountered in practice. However, it represents a global instability pattern resulting from extensive tearing of the dorsal capsule and the extensor pollicis brevis (EPB) tendon (27). The simple dislocation or subluxation is the most striking with regard to physical findings because the proximal phalanx assumes a posture of almost 90° to the metacarpal axis. This is relatively easy to reduce, with sufficient anesthesia and reversal of the responsible mechanism.
In complex dislocation, the position of the proximal phalanx is almost parallel to the metacarpal. The finding of skin dimpling over the volar MCP suggests complex dislocation. In complex dislocation, the surgeon should initially attempt a closed reduction. This would include insufflating the joint with anesthetic agent to essentially float out the volar plate. The procedure should include hyperextension combined with an attempt to coapt the dorsal rim of the proximal phalanx and the dorsal aspect of the articular surface of the metacarpal head, then dragging the base of the proximal phalanx over the articular surface of the metacarpal head in an attempt to push the volar plate out of the joint. This approach will result in successful closed reduction in a reasonable number of these somewhat rare injuries.
After closed reduction of either simple or complex dislocation is attained, the physician should check lateral stability to evaluate the integrity of the collateral ligaments. Anteroposterior (AP) translation, extension, and flexion should be checked while the thumb is still anesthetized. If surgical reduction is elected, digital nerves, which are more central and subcutaneous in the thumb MCP dislocations, are at significant risk in the volar approach. Recovery of almost normal stability and motion is expected. After surgery, thumb spica splinting, including the interphalangeal (IP) joint, is advisable to allow healing of the dorsal or volar skin incision and the underlying tissues. It is reasonable to allow protected return to play at 3 weeks.
Collateral Ligament Injuries of the Thumb Metacarpophalangeal Joint
Injury to the ulnar collateral ligament is more common than that of the radial counterpart (28). The proper collateral ligaments are the main stabilizers of the thumb MCP joint to valgus and varus stress and are the most important structures to repair to restore stability to the destabilized thumb MCP joint. The accessory collateral ligaments and the EPB tendon contribute static stability. Repair of these structures is critical in restoring stability when they are significantly compromised. Volar subluxation as seen on lateral radiograph of the thumb is twice as common in radial collateral ligament injuries as ulnar collateral injuries. In general, radial collateral ligament injuries are less prone to need acute or delayed repair or reconstruction.
Radial Collateral Ligament Injuries
In radial collateral ligament injuries, tenderness, deviation to ulnar-directed stress, and asymmetry of skin findings in contralateral comparison are the basic tenants of the diagnosis. However, incomplete ligament injury can be converted to a complete injury by vigorous examination.
The treatment of the radial collateral ligament is determined by the competence of the remaining ligament. Anatomy on the radial side of the joint does not include any soft tissue structures that routinely interfere with direct opposition of the torn ends of the ligament as opposed to the ulnar side (Stener lesion). In radial collateral ligament injuries, nonoperative treatment has a greater chance of success.
For complete tears, open treatment is still advocated. Reattachment of the avulsed ligament back to (usually) the proximal phalanx through pullout wire or suture anchor is performed. The joint is typically held after soft tissue repair with a single percutaneous pin for the first 4 weeks, followed by protected mobilization. Protection in a cast for 4 to 6 weeks is standard.
Ulnar Collateral Ligament Injuries
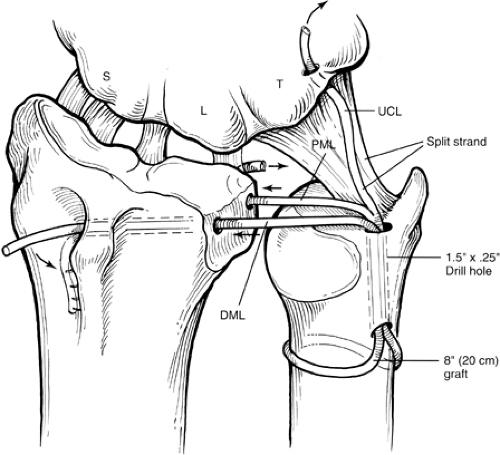
Gamekeeper’s thumb, or skier’s thumb, is one of the most common injuries in sports medicine and hand surgery. Palpation of the ulnar side of the MCP joint immediately after the injury may reveal a swelling that represents the distal edge of the displaced ulnar collateral ligament, the Stener lesion, which represents an avulsion of the UCL with proximal migration volar to the thumb adductor musculature (29) (Fig 24-8). The stress examination, under local anesthesia, is the most critical physical examination maneuver.
Examination should be performed by applying radially directed stress with the MCP joint in both neutral and 30-degree flexed posture. The flexed position isolates the UCL stabilization effect from that of the other ulnar-sided restraints. When compared to the other thumb, relative deviation compared with the contralateral side of greater than 10 to 15 degrees usually indicates complete tear.
The quality of the end point is an important indicator of ligament integrity.
Radiographs should be used for all patients to detect the presence and extent of bony injury. Radiographs should be performed prior to vigorous examination. Arthrography has been employed in several studies to determine the extent of MCP injury and the presence of a Stener lesion (30). The combination of palpation, stress examination, and fluoroscopic evaluation (Fig 24-9) remain the primary tools for diagnosis of these injuries.
Radiographs should be used for all patients to detect the presence and extent of bony injury. Radiographs should be performed prior to vigorous examination. Arthrography has been employed in several studies to determine the extent of MCP injury and the presence of a Stener lesion (30). The combination of palpation, stress examination, and fluoroscopic evaluation (Fig 24-9) remain the primary tools for diagnosis of these injuries.
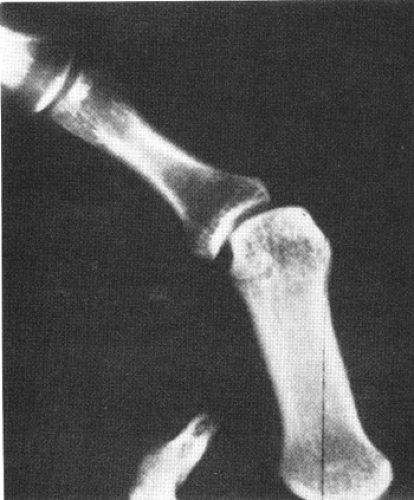 Fig 24-9. Stress radiographs of ulnar collateral ligament injuries of the thumb are indicated if complete rupture is not obvious on clinical examination. |
Treatment
Partial tears treatment: 2 to 6 weeks of immobilization in a forearm-based thumb spica with the IP joint included, followed by hand-based orthosis that allows wrist motion up to the fourth week to be followed by taping for an additional 2 to 4 weeks.
Complete tears treatment: anatomic repair is the rule (31). Because the Stener lesion is present in up to half of the suspected complete tears, open treatment is indicated. The primary repair is believed to yield superior results to late reconstruction and is thought to be possible up to 1 year post injury, after which an allograft reconstruction (using palmaris longus tendon) should be considered. Finding volar subluxation related to an ulnar-sided injury is an indication for open repair because it indicates severe tissue compromise
Technique of Repair of the Thumb MCP Ulnar Collateral Ligament. If the diagnosis is complete tear of the UCL, then surgical repair is indicated. A “lazy-S-shaped” incision is used that courses from the ulnar mid-axial line across the dorsum of the MCP joint and then proximally along the radial border of the metacarpal. Branches of the superficial radial nerve lying in the deep subcutaneous layer should be identified and protected. The proximal edge of the adductor aponeurosis is identified. A longitudinal incision is made in the adductor aponeurosis parallel and approximately 2 to 3 mm volar to the ulnar border of the extensor pollicis longus (EPL). The aponeurosisis reflected volarly to expose the ulnar aspect of the MCP joint, including the volar base of the proximal phalanx.
Tears in the middle two-thirds of the ligament can be re-approximated with interrupted figure-of-eight sutures using nonabsorbable suture material like 3-0 or 4-0 nylon. The ligament, however, is usually avulsed distally and can be approximated to the distal stump or into the bone defect from which it was detached with pull-out suture technique or a bone anchor. Secure fixation of the ligament to bone can be achieved by pull-out suture technique after scarifying the bone at the site of reattachment. A monofilament synthetic suture such as 3-0 Prolene, nylon, or stainless steel wire is placed in the proximal stump of the UCL with a modified Kessler technique. Keith needles are drilled across the base of the proximal phalanx to exit percutaneously on the radial side. The ends of the suture in the UCL stump are threaded through the eye of the Keith needles, which are then pulled through the proximal phalanx. The ligament is pulled up to the shallow trough previously made in the ulnar base of the phalanx and the ends of suture then tied over a button. An important technical point here is that the ligament repair needs to be performed such that the ligament is reinserted volar to the axis of rotation of the joint, so as not to cause undue tension to the repair and ultimately limit joint flexion.
If a fragment of bone accompanies the avulsed ligament, the repair technique is based on the size of the fragment. If the fragment is less than 15% of the articular surface, it can be excised and the ligament inserted directly into the defect with a pull-out suture. If the fragment is larger than 15% of the articular surface, it is reduced anatomically into the defect with a pull-out suture. A suture is placed between the distal volar portion of the repaired ligament and the volar plate to secure this three-dimensional complex. Repair of the dorsal ulnar capsule is performed to prevent volar subluxation of the joint. Radial stress is applied to the joint to test the stability of the repair. The thumb is immobilized in a thumb spica cast with the IP joint left free to move, which is encouraged to prevent adhesions of the extensor mechanism during healing time. Cast immobilization is continued for approximately 4 weeks, after which a hand-based orthosis is used to immobilize the MCP joint. Splint protection is discontinued 2 weeks later. Unrestricted use is not recommended for at least 3 months following surgery.
Metacarpophalangeal Joint
The MCP joint is a condyloid joint that allows greater freedom of movement than the interphalangeal joint. The collateral ligaments, volar plate, joint capsule, deep transverse
intermetacarpal ligament, and tendons all play a role in the stability of the MCP joint.
intermetacarpal ligament, and tendons all play a role in the stability of the MCP joint.
The safe position of the MCP joint is fully flexed because the proper collateral ligaments are at their greatest length and thus will not contract. Dislocations or subluxation of the MCP joint is relatively uncommon.
Lateral Plane Injury: Full-blown lateral injury is rare, but strains of the ligaments and small avulsion or impaction fractures are commonly seen.
Spontaneous reduction with reasonable stability is the rule for these injuries. Splinting and gradual liberation to play with appropriate buddy taping is the typical modality of treatment.
Dorsal Metacarpophalangeal Dislocations
The term simple dislocation has historically referred to an MCP joint that is in 70- to 90-degree of extension; however, the proximal phalanx is still in articular contact with the metacarpal head.
Complex dislocation, as described previously in the thumb section, denotes axial, dorsally translated, arrangement between the metacarpal and the proximal phalanx. As described previously in the thumb section, an attempt at closed reduction under adequate anesthesia should be made in all MCP dislocations. The reduction technique entails hyperextension at the MCP joint, enabling the dorsal margin of the proximal phalanx to contact the dorsal margin of the metacarpal head. The phalanx may be translated proximally or distally to “capture” the volar plate. The phalanx is then pushed across the metacarpal articular surface, with care to maintain the dorsal rim contact as long as possible to cause the volar plate to “pop” out of the joint and back into position. Postreduction radiographs are a must. Brief splinting for 3 to 5 days in the functional or safe position is followed by a buddy taping regimen to prevent hyperextension and allow motion. If closed reduction is unsuccessful, immediate open reduction is warranted. The common surgical approach to dorsal MCP dislocation is dorsal.
Volar Metacarpophalangeal Joint Dislocations
Volar MCP dislocation is extremely rare (32). The tissue that almost always causes difficulty in achieving closed reduction is likely a combination of the collateral ligament, the volar plate, the MCP capsule, and possibly the extensor mechanism. To reduce a volar MCP dislocation, the steps in reduction of a dorsal dislocation can simply be reversed. Failed closed reduction necessitates immediate open reduction through a volar approach to remove the interposed tissue. After reduction and brief splinting, motion is encouraged.
Proximal Interphalangeal Joint Dislocation
The proximal interphalangeal (PIP) joint dislocation is very common in all sports. The collateral ligaments along with the volar plate provide the most resistance to stress forces in lateral deviation. Secondary restraints include the joint capsule, flexor tendon sheath, and parts of the extensor apparatus. PIP dislocations are classified as dorsal and volar based on the direction of the distal segment.
Dorsal Proximal Interphalangeal Dislocations
The dorsal PIP dislocation is the most common PIP dislocation (Fig 24-10). Hyperextension of the middle phalanx is the usual mechanism. This entity can be either pure soft tissue or combined soft tissue and bone injury. Reduction is usually performed under digital block anesthesia. After reduction has been attained, while the patient’s finger is still anesthetized, it is important to test the range of motion through which the PIP remains stable and to observe the quality of the end points. The majority of these injuries will resume a concentric reduction and will have immediate stability in all directions but the extremes of hyperextension forces. The hallmark of closed treatment of these injuries is dorsal extension block splinting.
Volar Proximal Interphalangeal Dislocations
Volar dislocations are rare (33) (Fig 24-11). This is usually sustained when an extended digit is forcibly flexed at the PIP joint. The determining factors of treatment are the ability to achieve and maintain closed reduction and the extent of extensor mechanism disruption. Stable closed reduction should be kept in a position of PIP extension for a period of 4 to 6 weeks. Joint pinning can be used instead when there is difficulty in maintaining the extended posture in a splint. Formal open reduction is necessary when the lateral band of the extensor mechanism is blocking reduction. Primary repair of the rent between the lateral band and the central
tendon is advocated to avoid the development of a traumatic boutonnière deformity. Pinning after open repair is recommended. Early motion in volar dislocations is discouraged because the injured extensor must be allowed to heal.
tendon is advocated to avoid the development of a traumatic boutonnière deformity. Pinning after open repair is recommended. Early motion in volar dislocations is discouraged because the injured extensor must be allowed to heal.
Distal Interphalangeal Dislocations
Dislocation of the distal interphalangeal (DIP) joint is often seen in contact sports. The great majority of these dislocations are dorsal dislocations. After reduction, immediate stability is the rule. These injuries are commonly treated in a DIP extension splint, which keeps the DIP in a full extension or slightly hyperextended position for 6 weeks. DIP pinning can be used instead if DIP cannot be maintained in a splint, mostly due to patient’s occupation. Joint pinning is performed after open reduction for 4 weeks, while the PIP joint is left free for movement.
Distal Radioulnar Joint Anatomy
The anatomy of the distal radioulnar joint (DRUJ) is complex. The DRUJ articulation is trochoid. The marginal ligaments of the triangular fibrocartilage (TFC) are important in load transference from the carpus to the ulna and in the stability of the DRUJ.
The joint is most stable in the extremes of rotation, where the compressive forces between the radius and the ulna are resisted by the reciprocal tensile forces developed within the opposite TFC marginal ligament (34,35). Clinical stability is obviously related to many factors.
Ulnocarpal Ligaments
TFC and ulnocarpal ligaments constitute the triangular fibrocartilage complex (TFCC). The ulnocarpal ligaments are the combined volar UL and UTq ligaments. These ligaments originate at the base of the styloid, in tandem with the apical attachment of the TFC and insert volarly on the lunate and triquetrum.
Other Stabilizing Factors
The TFC and ulnocarpal ligaments make up the TFCC. Stability of the radioulnar-carpal unit is further influenced by the conformation of the sigmoid notch and the interosseous membrane (36), the extensor retinaculum, and the forces of the ECU and the pronator quadratus, and also by the dorsal carpal ligament complex. The DRUJ capsule is uniformly thin and cannot be thought of to offer stability in the usual sense.
Acute Joint Instability
Triangular Fibrocartilage Complex Disruption with Distal Radioulnar Joint: Instability Associated with Fractures or Dislocations. When the TFCC and DRUJ disruption is associated with radial or ulnar fractures or other dislocations, accurate closed reduction of the dislocation and associated fracture, followed by appropriate cast immobilization in mid-rotation with slight ulnar deviation and palmar flexion will often solve the problem. Alternative fracture management should be considered rather than accepting abnormal joint positioning. Ligament repair (DRUJ and TFCC) should be strongly considered when open reduction of the fracture is required and DRUJ disruption is evident.
The Essex-Lopresti Lesion (Radial Head Fracture with Injury to the Interosseous Membrane and Triangular Fibrocartilage Complex). DRUJ disruption associated with a displaced radial head fracture and proximal migration of the radius is termed the Essex-Lopresti fracture (37,38). The injury is complex, with sequential forces disrupting the DRUJ ligaments, interosseous membrane, and radiocapitellar articular surface. A high index of suspicion should occur in any patient with a displaced radial head fracture or acute DRUJ displacement. Posteroterior (PA) and lateral comparison views of both forearms, including the elbow and wrist, should be followed by comparison computed tomography (CT) scans of the DRUJ if any suspicion of this injury persists on plain films. If the forearm is to be opened for associated fractures, one should look at the interosseous membrane with a tendency toward repair or reconstruction. Acute large-fragment radial head fractures should be fixed in addition to reduction, repair, and pinning of the DRUJ (39). Acute, comminuted radial head fractures should be excised with replacement by radial head prostheses and the DRUJ reduced, repaired, and pinned. Fortunately, this combination of injuries is rare, and forearm longitudinal instability, though rare, is often missed. Early surgical address of associated injuries in this entity is critical in order to avoid late and often nonsalvageable forearm pathology.
Isolated Triangular Fibrocartilage Complex Disruption with Dislocation or Instability of the Distal Radioulnar Joint. Isolated DRUJ dislocations will respond to cast immobilization for 6 weeks if an accurate closed reduction can be obtained. If the ulna is palmar relative to the radius, pronation will reduce the dislocation. If the ulna is dorsal, supination will usually reduce the joint (40). It has been recommended that a long arm cast be used with the forearm in full supination for ulna dorsal and in full pronation for ulna volar. Most acute closed DRUJ disruptions can be satisfactorily handled by a careful nonoperative approach as described above.
The joint should be opened and reduced and the TFCC repaired only if the dislocation is locked or the reduction is incongruous. If instability persists after cast treatment and reasonable rehabilitation, the problem may be satisfactorily solved by operative intervention.
Management of Chronic Joint Instability
Stabilization by primary repair of the TFCC is recommended if possible. Although this approach should be considered first, problems such as contracture or loss of tissue may demand a reconstructive approach. There is no single optimal operation, but the following have received some support.
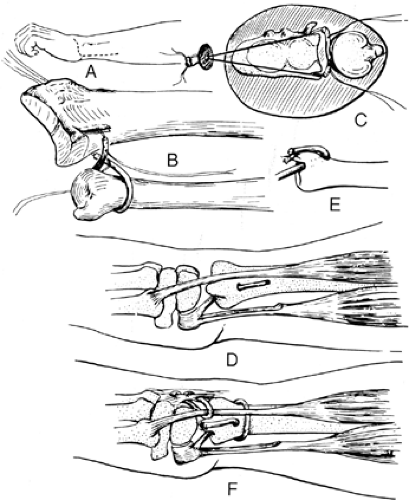
Triangular Fibrocartilage Complex Reconstruction or Substitution. The Bunnell-Boyes procedure (41) is innovative and anatomic insofar as reconstruction of DRUJ instability (Fig 24-12).
The procedure uses distally based portion of the FCU harvested proximally and stripped distally to the pisiform attachment. The new ligament is stabilized distally by weaving it through the remaining volar capsule. This new ligament is then passed through a drill hole in the styloid area and exits in the apex of the ulnar articular surface. The repair is completed with imbrication of the dorsal capsule. Others have used a reconstructive approach as illustrated in Figure 24-13. A palmaris or plantaris graft is harvested and doubled on itself. The two ends are looped around the neck of the ulna and passed distally through an oblique one-quarter-inch drill hole in the ulna. The hole begins proximally at the neck of the ulnar articular prominence and exits in the fovea at the TFC’s normal anatomic attachment site. The two ends are then used to reinforce or replace deficient portions of the dorsal and/or palmar marginal ligament or ulnocarpal ligaments. Many techniques have been described to accomplish the same extrinsic stability of the disrupted DRUJ. No single technique has been deemed superior, due to the absence of controlled trials in the literature.
The procedure uses distally based portion of the FCU harvested proximally and stripped distally to the pisiform attachment. The new ligament is stabilized distally by weaving it through the remaining volar capsule. This new ligament is then passed through a drill hole in the styloid area and exits in the apex of the ulnar articular surface. The repair is completed with imbrication of the dorsal capsule. Others have used a reconstructive approach as illustrated in Figure 24-13. A palmaris or plantaris graft is harvested and doubled on itself. The two ends are looped around the neck of the ulna and passed distally through an oblique one-quarter-inch drill hole in the ulna. The hole begins proximally at the neck of the ulnar articular prominence and exits in the fovea at the TFC’s normal anatomic attachment site. The two ends are then used to reinforce or replace deficient portions of the dorsal and/or palmar marginal ligament or ulnocarpal ligaments. Many techniques have been described to accomplish the same extrinsic stability of the disrupted DRUJ. No single technique has been deemed superior, due to the absence of controlled trials in the literature.
Substitution. Radioulnar tether procedures are the historical approach to substitution (42,43). Johnson (44) has proposed advancement of the pronator quadratus from its normal insertion on the ulna to a more lateral and dorsal insertion. He postulated that this might increase radioulnar joint stability.
Osteotomy. This is included in several procedural approaches to disorders of the DRUJ. The types of osteotomy vary, but it is used to correct abnormal rotation, angulation, or length discrepancies between the two forearm bones (45). Osteotomies should be considered only when there is demonstrable maintenance of the articular cartilage of the DRUJ. A CT scan of the DRUJ is a critical step in assessing the congruence and anatomy of the joint, as well as providing insight as to the quality of the cartilage. In the absence of joint cartilage, arthrodesis, arthroplasty, or excision should be considered. Algorithms have been developed to assist in the decision-making process.
Osteotomy of the Distal Radius. Osteotomy of the distal radius should be considered when correction of malunion or deformity of the distal radius is needed. The surgical technique usually requires a buttress plate and the addition of a bone graft.
If the original injury or insult involved the sigmoid notch, one must presume that this DRUJ surface is abnormal. An osteotomy done proximal to this level might not correct the sigmoid irregularity but instead change its angular relationship to the distal ulnar articular surface. If the deformity is the result of an injury not involving the notch, one might expect a well-done osteotomy to be highly beneficial if radial length, tilt, and inclination are well corrected.
Osteotomy of the Ulna. Performed to correct problems with ulnar shortening, rotation, or angulation. A variety of procedures have been utilized including ulnar head excision (46), hemiresection interposition arthroplasty with shortening (47,48), and ulnar recession and fusion of the ulnar head to the radius with restoration of forearm motion through creating a proximal pseudo-arthrosis (Sauve-Kapandji procedure) (49,50).
Articular cartilage is composed of hyaline cartilage that covers articulating surfaces. It is composed of
Chondrocytes (5%)
Extracellular matrix (95%)
Water (75%)
Collagen (mainly Type 2) (5%)
Proteoglycans (20%)
Enzymes
Growth Factors (PDGF, Platelet-derive growth factor; TGF beta, Transforming growth factor; FGF, Fibroblast growth factor; IGF-1, Insulin-like growth factor 1)
Lipids
Adhesives (fibronectin, chondronectin)
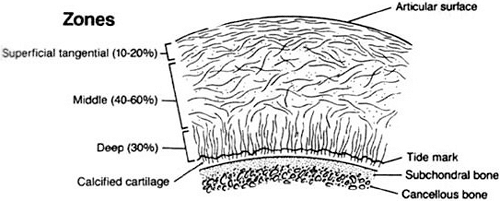
Articular cartilage zones (Fig 24-14) (superficial to deep) are:
Surface
Superficial Tangential Zone: Collagen fibers (Type 2) orientated tangential to surface. This layer has the greatest ability to resist shear stresses.
Transitional/Middle Zone: This is the transition between the shearing forces of surface layer to compression forces in the cartilage layer. In this layer collagen is arranged obliquely. This layer is composed almost entirely of proteoglycans.
Radial/Deep Zone: Here the collagen fibers are attached radially (vertical) into the tidemark. This layer distributes loads and resists compression.
Calcified Zone: This layer contains the Tidemark Layer (basophilic line that straddles the boundary between calcified and uncalcified cartilage). This layer contains Type 10 collagen.
Chondrocytes (5% wet weight): Chondroblasts, which are derived from mesenchymal cells, become trapped in lacunae and develop into chondrocytes. Chondrocytes are important in the control of matrix turnover through production of collagen, proteoglycans, and enzymes for cartilage metabolism.
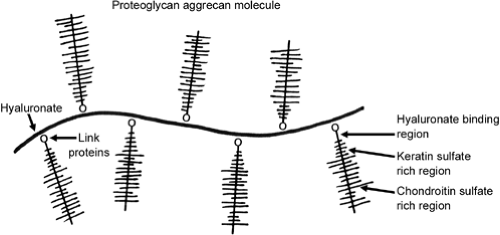
Organic Matrix: Proteoglycans (PG): 10% to 15% of wet weight. They are produced by chondrocytes and secreted into the matrix. These are responsible for the compressive strength of cartilage and serve to trap and hold water to regulate matrix hydration and bind growth factors. Proteoglycans look like test tube brush with keratan and chondroitin sulphate chains (glycosaminoglycans, GAGs) bound to a protein core molecule monomer (Fig 24-15). The monomer is attached via a link protein to hyaluronic acid. GAGs include: chondriotin-4-suphate (decreases with age), chondriotin-6-sulphate (increases with age), and keratan sulphate (increases with age). GAGs are bound to a protein core by sugar bonds to form a proteoglycan aggregen molecule. Link proteins stabilize aggregen molecules to hyaluronic acid to form a proteoglycan aggregate (Fig 24-16). The aggregated proteoglycans and water are strongly electronegative. This generates a resistance to compressive force and contributes to the elasticity of cartilage. Hyaluronic acid is the major aggregating factor.
Collagen: Mainly Type 2. Other Types = 5, 6, 9, and 11. Type 9 lies on the surface of Type 2, acting as interfibrillary glue. Type 10 is associated with calcification of cartilage. Disruption
of the collagen network is a key factor in the development of OA. Collagen forms the cartilaginous framework and is responsible for the tensile strength of cartilage.
of the collagen network is a key factor in the development of OA. Collagen forms the cartilaginous framework and is responsible for the tensile strength of cartilage.
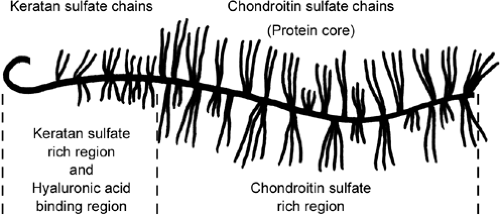 Fig 24-16. Link proteins stabilize aggregen molecules to hyaluronic acid to form a proteoglycan aggregate. |
Water: 75% of wet weight. Allows for deformation of the surface by shifting in and out in response to stress. Increased water content causes an increase in the permeability, decreased strength, and decreased Young’s modulus (less stiff). Water content increases in osteoarthritis.
Articular Cartilage Function: 1- Decreases friction in joints. 2- Load distribution in joints.
Articular Cartilage Nutrition: Mature articular cartilage is avascular, aneural, and alymphatic. Chondrocytes receive nutrition and oxygen via diffusion from synovial fluid through the cartilage matrix.
Articular Cartilage Biomechanics: Creep occurs when a viscoelastic tissue, like cartilage, is subjected to a constant load. Stress relaxation occurs with constant deformation. In contrast to bone, articular cartilage tends to stiffen with increasing strain.
Changes with Aging: With aging, cartilage becomes hypocellular and has decreased elasticity. Chondrocytes increase in size, increase their lysosomal enzymes, and cartilage becomes hypocellular (cells stop reproducing). Proteoglycans decrease in mass and size due to a decrease in the length of chondroitin sulfate chains and change in proportion. Keratin sulfate increases and hyaluronic acid decreases. Water content decreases with aging (increases in OA) and protein content increases due to a decrease in the ratio of carbohydrates to protein. Much of hyaline cartilage of the body ultimately calcifies with aging. When calcification occurs, chondrocytes die and matrix disintegrates. The superficial zones do not calcify, except in pathologic states such as pseudogout.
Healing of Articular Cartilage
Deep Lacerations: Extend below the tidemark and heal with fibrocartilage. Blunt trauma may cause osteoarthritic changes.
Superficial Lacerations: Above the tidemark. Chondrocytes proliferate but do not heal. Immobilization leads to atrophy while continuous passive motion is beneficial to healing.
Degenerative Joint Disease of the Hand: Osteoarthritis of the hand preferentially involves the DIP joint and the carpometacarpal (CMC) joint of the thumb. The PIP joint is affected less commonly. A multitude of hypotheses have been suggested for factors involved in osteoarthritis. Alterations in cartilage metabolism, trauma, infection, joint laxity, diet, hormonal changes, gout, calcium pyrophosphate deposition, microfractures, and immunologic factors have all been implicated in the etiology of osteoarthritis. Genetic factors play a role in some forms of osteoarthritis. The arthritic PIP joint demonstrates fusiform joint swelling. With progression of the condition, marginal osteophytes (Bouchard nodes) become evident with progressive lateral deviation of the digits (Fig 24-17).
Pain, stiffness, diminished strength, and angular deformities are the most common complaints. Early in the degenerative process, the patient complains of pain aggravated by activities. Often, in time, pain decreases but the deformity remains. Radiologic findings include severe joint destruction, subchondral sclerosis, and osteophyte formation. The differential diagnosis usually includes inflammatory arthritides, including rheumatoid arthritis. Periarticular osteopenia and involvement of the MCP joint characteristic of rheumatoid arthritis are usually absent in erosive osteoarthritis. Nonoperative treatment of patients with PIP joint arthritis is directed toward relieving pain, reducing swelling, and protecting the joint from further deterioration. During episodes of inflammatory response, rest rather than increased activity is indicated by using a removable resting splint of a thermoplastic material to
immobilize the PIP joint in full extension. Coban elastic bandage is used to wrap the finger in a circumferential manner from the fingertip to the web space of the digits in order to diminish morning swelling, and it can be used in association with the immobilization splint. Occasional injections of intra-articular glucocorticoids into the PIP joint may provide pain relief and decrease the inflammatory process. However, the authors are reluctant to prescribe this modality of treatment on a routine basis. More recently, multiple nonsteroidal anti-inflammatory drugs (NSAIDs) have emerged with preeminent efficacy. Adverse effects include upper gastrointestinal intolerance, ulceration, platelet dysfunction, and renal dysfunction. NSAIDs should not be considered in the presence of recent or active peptic ulcer or upper gastrointestinal bleeding and should be used with caution in older patients (>70 years) or in patients with a history of asthma.
immobilize the PIP joint in full extension. Coban elastic bandage is used to wrap the finger in a circumferential manner from the fingertip to the web space of the digits in order to diminish morning swelling, and it can be used in association with the immobilization splint. Occasional injections of intra-articular glucocorticoids into the PIP joint may provide pain relief and decrease the inflammatory process. However, the authors are reluctant to prescribe this modality of treatment on a routine basis. More recently, multiple nonsteroidal anti-inflammatory drugs (NSAIDs) have emerged with preeminent efficacy. Adverse effects include upper gastrointestinal intolerance, ulceration, platelet dysfunction, and renal dysfunction. NSAIDs should not be considered in the presence of recent or active peptic ulcer or upper gastrointestinal bleeding and should be used with caution in older patients (>70 years) or in patients with a history of asthma.
Surgical Therapy
Operative treatment is indicated for the PIP joint when medical management has failed to relieve the pain, when the digit deformity is interfering with hand function, or when a significant restriction of motion limits the activities of daily living. When choosing the method of surgical treatment for a painful arthritic PIP joint, consider the clinical role of the PIP joint in the patient’s particular activities.
Flatt (51) noted that the PIP joint has the greatest degree of movement and functional adaptations of the hand. He has found loss of movement to be a frequent complaint, especially in the third, fourth, and fifth digits.
Stability is equally important, especially in the radial digits involved during pinching activities, in which the index finger must withstand forceful contact with the thumb, especially in the lateral or key pinch. Patients with impaired index fingers pinch with the middle finger when possible, so stability of the middle finger becomes more important when the index finger is affected also. Relatively few surgical options exist for the painful arthritic PIP joint. Most surgeries are arthroplasties or arthrodeses. There has also been limited success with joint denervation when other techniques are either not indicated or not desired by the physician or patient.
Arthroplasty
A Swanson silicone interpositional arthroplasty (52) of the PIP joint through a dorsal approach has been recommended. However, a volar surgical approach is advocated by many because it minimizes the risk of extensor lag, avoids interference with the extensor tendons, preserving the central slip, allows for more prompt active range of motion in the postoperative period, and eliminates the risk of central slip rupture with a resultant boutonniere deformity or a flexion contracture deformity.
The volar approach also has better cosmetic and functional results. This approach provides an excellent exposure, which is critical given the importance of the technique with this type of procedure. However, with the volar approach, the risk of creating a swan-neck deformity exists.
One potential shortcoming of the silicone implant is if the collateral ligaments are compromised, implantation of the device in the index or long finger PIP joint may affect lateral pinch stability. In contrast, most surface resurfacing implants preserve collateral ligaments.
Many surgeons favor a dorsal approach, with longitudinal splitting of the extensor tendon or through a distally based flap of the central slip, as described by Chamay in 1988 (53). The Chamay approach is the favored approach for surface replacement arthroplasty (SRA). Various nonsilicone implant arthroplasties are either available for use or under investigation. They include the Saffar, the Digitos, the DJO3A, the Mathy, the Ascension, and the Avanta PIP SRA.
An alternative treatment for PIP joint osteoarthritis is arthrodesis of the joint in a functional position. This option continues to be the best surgical treatment for the painful unstable PIP joint in the index or long finger, which is usually subjected to lateral stress during pinching activities. Arthrodesis offers stability, durability, and little need for further procedures. It is the procedure of choice for the index finger. However, depending upon the patient’s needs, arthrodesis may impair or even be incompatible with satisfactory function. On the ulnar aspect of the hand, preservation of mobility at the level of the PIP joint is important, especially to obtain functional ability to grasp small objects. Arthrodesis of the PIP joint is indicated mainly for the index and middle fingers in patients who are young or active or when a significant loss of bone has occurred.
Surgical Methods
Arthroplasty
In the volar approach, a radial- or ulnar-based Bruner incision is made, with the apex at the PIP joint flexion crease. After the skin flap is elevated, the Grayson ligaments are completely released from their origin, exposing the neurovascular bundle. The bundle is retracted, exposing the Cleland ligaments dorsally. These also are released.
The proximal and interphalangeal transverse digital arteries, which consistently are present as communicating branches from the digital arteries, are cauterized and transected, allowing full mobilization of the neurovascular structures. The flexor tendon sheath is released by dividing the origin of the first and second cruciform pulleys and the third annular pulley at the volar plate. The volar plate is fully exposed and is released proximally and along its lateral margins from the accessory collateral ligaments, which are seen upon release of the transverse retinacular ligament from the volar capsule and tendon sheath. The collateral ligaments are then released proximally and the joint is opened by hyperextension. The flexor tendons retract to one side, and the neurovascular bundles are displaced dorsally. Both articular surfaces are completely exposed in this manner. The medullary cavities of the bone are reamed in order to accommodate the proper size of implant. After the implant is inserted in place, it is essential that full range of motion exists and the implant is stable.
Resurfacing prosthetic procedures, with or without bone cement, have been designed for the replacement of this joint. Limited experience with this design has shown promise for future consideration as an alternative treatment. The exposure for most SRAs spares the collateral ligaments; therefore, these joint replacements are an option for the index and long fingers.
Arthrodesis
The preferred position for arthrodesis of the PIP joints is 30 to 40 degrees for the index and the middle finger, 50 degrees for the ring finger, and 55 degrees for the small finger.
Several different arthrodesis techniques for the PIP joint are based on the type of fixation used. The appropriate finger position varies for the radial to the ulnar fingers and with the assessment of the patient’s particular needs. K-wires, interosseous wiring, tension band wiring, and screw fixation have been used to achieve a solid nonpainful arthrodesis. The rate of nonunion is reported to be at 0% to 10%.
Postoperative Care: Primary wound healing is the first goal of postoperative care. Elevation is important to prevent swelling. Active motion of the PIP joint usually begins on the third to seventh day, as the swelling subsides. A Coban elastic bandage helps to control swelling.
Following arthrodesis surgery, the PIP joint is protected in a dorsal and volar Orthoplast splint for approximately 4 to 6 weeks. Motion of the MCP and DIP joints is allowed shortly after surgery.
A hand therapist evaluates the patient to ensure adequate splinting, joint protection, and assistive devices to carry out activities of daily living. Patients with silicone implant arthroplasties are monitored indefinitely for signs of fracture. Patients who have undergone SRAs are likewise monitored indefinitely for signs of loosening.
Patients who have undergone arthrodeses are monitored radiographically for signs of bony union. Hardware removal may become necessary but is not recommended until a year after surgery.
The periscaphoid area is the site of 95% of all wrist degenerative diseases. SLAC of the wrist is the most common pattern of degenerative arthritis in the wrist. Watson and Ballet (54) coined the term SLAC wrist in 1984. The hallmark of the disorder is scaphoid or S-L ligament injury with collapse on the radial side of the wrist. It is most common in the dominant wrist. A SLAC wrist pattern is the result of many radial-sided wrist pathologies. Most common is S-L dissociation with rotatory subluxation of the scaphoid. Scaphoid nonunion advanced collapse (SNAC) is another common cause (Fig 24-18). Other etiologies include Preiser disease (avascular necrosis of the scaphoid), midcarpal instability, intra-articular fractures involving the RS or capitate-lunate joints, Kienböck disease, primary degenerative arthritis with attenuation of the S-L ligament and S-L dissociation, capitolunate degeneration, and inflammatory arthritis, such as seen in the crystalline deposition disorders of gout and calcium pyrophosphate dihydrate deposition disease (CPPD).
Pathophysiology and Staging
The distal radius has two articular fossae for the scaphoid and lunate. The scaphoid fossa is elliptical or ovoid. It narrows towards the radial styloid in a dorsal-volar plane. Thus, the scaphoid proximal articular surface is shaped like a spoon. The lunate fossa is spherical. Injury of the scaphoid or its supportive ligaments can cause radial-sided collapse with flexion of the scaphoid, thus resulting in incongruency of the RS joint.
Thus, narrowing of the RS joint first begins at the radial styloid aspect (Stage 1A). Radiographic changes appear as a sharp elongation on the radial styloid. As the disease progresses, the rest of the RS joint is destroyed (Stage 1B). In Stage 1B, the entire scaphoid fossa is involved. Complete collapse of RS joint alters the normal load-bearing ability of the capitolunate joint. This results in a radial or dorsal radial position of the capitate. Shear stress destroys cartilage in the capitolunate joint leading to the most advanced stage,
midcarpal SLAC (Stage 2). In Stage 2 (Fig 24-19), the capitolunate joint is additionally narrowed and sclerotic. As the arthritic pattern thus progresses, it shifts from the scaphoid fossa of the radius to the midcarpal capitate articulation.
midcarpal SLAC (Stage 2). In Stage 2 (Fig 24-19), the capitolunate joint is additionally narrowed and sclerotic. As the arthritic pattern thus progresses, it shifts from the scaphoid fossa of the radius to the midcarpal capitate articulation.
 Fig 24-19. Stage II SNAC wrist, with RS narrowing and preserved capitolunate and radiolunate joints. |
At all stages of SLAC wrist, the radiolunate joint is least involved because of its spherical shape. The lunate is congruently loaded in every position and, thus, highly resistant to degenerative changes. This sparing of the lunate fossa provides a basis for some of the motion-preserving procedures to treat SLAC wrist.
Long-standing and untreated SLAC wrist can lead to a painful wrist at rest and during use, deterioration of range of motion (ROM), and decreased grip strength. The radiographic SLAC appearance does not always correlate with the patient’s symptoms.
Clinical Presentation and Evaluation
A history of wrist injury, scaphoid fracture, carpal tunnel decompression, or carpal ganglion excision may be present. Many patients with SLAC wrist have minimal symptoms and may present because of a secondary problem, such as carpal tunnel syndrome (CTS). Patients may have a variable duration history of wrist pain during activity. Patients relate their symptoms to increased activity and overuse. Post activity pain may be present. Patients may have modified their activities, depending on the severity of symptoms. Many patients have used NSAIDs for pain relief.
Wrist edema may be present, and patients may have pain with motion, especially when loading the wrist in an extended position. Limited wrist ROM is typical, and an average wrist flexion/extension arc of 80 to 90 degrees has been reported. Direct palpation of the S-L joint or radiocarpal joint generally elicits pain. Pain with resistance against active finger extension while the wrist is held in passive flexion is common. A scaphoid shift test also elicits pain.
Plain wrist radiographs [posteroanterior (PA), lateral, and oblique] are usually sufficient to make the diagnosis and permit staging. They can reveal joint narrowing, sclerosis, osteophytes, cysts, S-L dislocation, and carpal collapse. Early changes at the RS articulation can appear as an elongated radial styloid process. The scaphoid may assume a vertical position with a cortical ring sign. In SLAC secondary to S-L dissociation, increased distance between the scaphoid and lunate as well as lunate ulnar translocation will be obvious. A lateral view can show an increase in the S-L angle with a dorsiflexion of the lunate [dorsal intercalated segment instability (DISI) deformity]. As the disease progresses, the whole RS joint becomes narrowed. In subtle cases, PA and lateral wrist CT can reveal these joint changes. For imaging of the skeletal morphology or occult fracture, CT is most useful. If avascularity is a concern, then magnetic resonance imaging is the best imaging modality.
Nagle (55) recommends staging wrist arthroscopy for articular surface evaluation since lunate fossa changes may be present in advanced cases of SLAC wrist but may not be appreciated on plain radiographs. Since scaphoid resection and ulnar column fusion in the presence of lunate fossa degenerative changes are contraindicated, an accurate assessment of the radiolunate joint is critical for correct surgical planning. When necessary, staging arthroscopy is performed as part of the definitive procedure.
Management
Nonoperative
Mild symptomatic SLAC can often be managed nonoperatively with periodic steroid injections, splinting, and NSAIDs. If the grip strength registers more than 80% that of the uninvolved wrist and the condition is not significantly impairing, then living with the condition is a valid option.
Operative Management: SLAC Reconstruction (Limited Wrist Fusion)
A SLAC reconstruction involves scaphoid excision and arthrodesis of the capitate, lunate, hamate, and triquetrum
(four-corner). Two parallel dorsal transverse incisions, a lazy S, or a central longitudinal incision over the distal radiocarpal joint and styloid process is made. The extensor retinaculum is incised through the third dorsal compartment. The terminal branch of the posterior interosseous nerve (PIN) in the floor of the fourth extensor compartment can be sacrificed as an adjunctive pain relief measure. The wrist capsule is opened over the capitolunate joint. The scaphoid is resected in piecemeal fashion. Articular cartilage and subchondral bone are removed from the capitate, lunate, hamate, and triquetrum. Care should be taken to maintain the anatomic relationship of the intercarpal intervals. Cancellous bone is harvested from the distal radius, the proximal ulna, or the iliac crest.
(four-corner). Two parallel dorsal transverse incisions, a lazy S, or a central longitudinal incision over the distal radiocarpal joint and styloid process is made. The extensor retinaculum is incised through the third dorsal compartment. The terminal branch of the posterior interosseous nerve (PIN) in the floor of the fourth extensor compartment can be sacrificed as an adjunctive pain relief measure. The wrist capsule is opened over the capitolunate joint. The scaphoid is resected in piecemeal fashion. Articular cartilage and subchondral bone are removed from the capitate, lunate, hamate, and triquetrum. Care should be taken to maintain the anatomic relationship of the intercarpal intervals. Cancellous bone is harvested from the distal radius, the proximal ulna, or the iliac crest.
Lunate DISI should be corrected, and five percutaneous K-wires are used. Two wires are placed through the capitate into the lunate, one each through the hamate and triquetrum into the lunate, and a fifth wire through the triquetrum into capitate. Cancellous bone graft is packed between the interstices of the four bones.
A long arm splint is placed after the procedure. After a week, the splint is replaced with a long arm cast, which is maintained for 3 weeks. Then, a short arm cast is placed and maintained for an additional 2 to 4 weeks. The cast and wires are removed when fusion is evident on radiographs.
Alternative methods for this four-quadrant fusion, such as the use of intercalary screws and a dorsal carpal plate, are made especially for this fusion. It remains to be seen whether the increased cost of such devices results in improved outcomes. More solid fixation does enable the use of a short arm cast and an earlier initiation of wrist ROM therapy. Patients with evidence of advanced radiocarpal arthritic changes are not candidates for this limited arthrodesis, and pre-operative discussion should include other options, such as devervation, total wrist arthrodesis, or wrist arthroplasty.
Proximal Row Carpectomy
PRC requires resection of the proximal row of wrist bones to enable articulation of the capitate within the lunate fossa. For a successful procedure, both the proximal capitate articular surface and the lunate fossa should ideally be free of pathology (56). The procedure is usually effective only when the disease is restricted to the RS joint; satisfactory capitate head articular surface and lunate fossa congruity must be confirmed. PRC provides the best motion but may be associated with painful narrowing of the RC joint. It is not indicated for Stage 2 SLAC wrist. It may serve as a salvage procedure for Stages 1A and 1B when limited wrist fusion is not indicated. Failure of PRC requires conversion to wrist arthrodesis.
A dorsal longitudinal or transverse incision is used. The extensor tendons are retracted. A longitudinal capsulotomy is extended radially and ulnarly. The capitate is identified and its articular surface is inspected. In the presence of capitate degenerative changes, the procedure should not be performed. If both proximal capitate articular surface and lunate fossa are free of pathology, the scaphoid, lunate, and triquetrum are excised. Both radioscaphocapitate and long RL ligaments are preserved. Wrist collapse follows, with placement of the capitate head in the lunate fossa along with radial deviation of the wrist. If impingement between the radial styloid and the trapezium is present, a limited radial styloidectomy is performed. Following the procedure, the wrist is splinted for 4 weeks. Early active digital flexion and extension are recommended. ROM exercises start 4 weeks after the procedure. Strengthening exercises and heavy lifting may begin 3 months after the procedure.
Total Wrist Arthrodis
Total wrist fusion diminishes pain, but wrist function is sacrificed. Patients may have functional limitations interfering with lifestyle, but current literature supports the fact that this procedure is compatible with most activities and job duties.
Using a central, dorsal, longitudinal incision, the extensor retinaculum is incised. The incision is carried down to bone surface from middle finger metacarpal to distal radius, raising capsular and periosteal flaps. Articular cartilage and subchondral bone are resected from the RS, RL, lunocapitate, scaphocapitate, and middle finger CMC joints. The radioulnar joint should not be entered unless distal ulna resection is planned. The radial metaphysis is generally used for the necessary cancellous bone graft and more distal harvest is not required.
Bone grafts are placed in the radiocarpal, midcarpal, and CMC fusion sites, and a wrist fusion plate is applied. The fusion plate is secured with screws at the middle finger metacarpal, the capitate, and the radius. Periosteal and capsular flaps are reapproximated. A short arm splint is applied until fusion can be seen on radiographs. Fusion is usually evident in 8 weeks.
Total Wrist Arthroplasty
Total wrist arthroplasty is an alternative to diffuse arthrosis of the wrist, especially in rheumatoid arthritis and if bilateral disease is present. With bilateral disease, a combination of a total wrist arthroplasty and a contralateral total wrist fusion is an option. Numerous implants have been used; however, major complications of implant loosening and wear of the components are common. In general, indications are in the lower-demand patient, especially with contralateral disease or prior arthrodesis. Newer implants and techniques have improved survivability of this prosthesis.
A common area of hand involvement in osteoarthritis is the CMC joint of the thumb. This is the joint that most commonly requires surgery in the osteoarthritic hand. Patients present with increasing pain at the base of the thumb. The joint space between the first metacarpal and trapezium narrows with loss of articular cartilage. Rotary motions of the joint are particularly painful. With a gradual lateral subluxation
of the joint, typically the thumb develops a “shoulder” or a prominence at its base. The patient has increasing difficulty applying pressure with the thumb, making any activity requiring pinch painful. A simple activity such as opening a car door becomes difficult and painful. Secondary deformities include adduction of the metacarpal and MCP hyperextension; these can cause further limitation in function, especially in activities involving grasp.
of the joint, typically the thumb develops a “shoulder” or a prominence at its base. The patient has increasing difficulty applying pressure with the thumb, making any activity requiring pinch painful. A simple activity such as opening a car door becomes difficult and painful. Secondary deformities include adduction of the metacarpal and MCP hyperextension; these can cause further limitation in function, especially in activities involving grasp.
Resting and splinting are frequently helpful in relieving pain and certainly should be tried before surgery is contemplated. Many of these patients respond to a conservative approach with relief of pain that is long-lasting in spite of advanced radiographic findings. When conservative treatment fails to relieve pain, arthroplasty affords an excellent solution. Three surgical approaches have been successful. The simplest procedure is osteotomy of the first metacarpal, which can provide satisfactory pain relief in 80% of patients (57). In another procedure, resection arthroplasty, the trapezium is removed and replaced by autogenous soft tissue, such as joint capsule or tendon. In the third approach, the trapezium is replaced by a prosthesis (58).
Resection arthroplasty gives predictable relief of pain but with some loss of pinch power and some residual proximal migration of the metacarpal. The advantages of this technique are the simplicity of surgical procedure and the consistency of satisfactory results. Other resection techniques may use a tendon sling to prevent proximal migration or to preserve the proximal half of the trapezium (59).
Trapezium replacement arthroplasties can also be used to maintain space and thumb alignment. Results with this technique, mainly using the silicone rubber trapezium prosthesis, were initially encouraging. However, this approach is surgically more demanding, and longer followup has shown increasingly frequent reports of prosthetic erosion or breakage or “Silastic synovitis” and deterioration of results (60). Thus, in most cases, complete trapezial resection with autogenous tissue interposition, with or without ligamentous reconstruction, is the procedure of choice (61).
CMC joint fusion can be successful in restoring stability and relieving pain in these patients but should be used only in patients who have localized CMC joint involvement and in whom MCP flexion is maintained. CMC joint fusion is currently advised only in traumatic arthritis in the young patient. This procedure requires 10 to 12 weeks of postoperative casting and has become less frequently used since the introduction of successful arthroplasties.
Flexor Tendon Anatomy
Tendons are vital structures connecting muscles to bones. The extrinsic flexors of the finger consist of the flexor digitorum profundus (FDP) and the flexor digitorum superficialis (FDS). The FDP originates from the proximal ulna and the interosseous membrane. In the forearm, it divides into two muscle groups, the most radial part supplying the index finger and the ulnar part supplying the middle, ring, and little fingers. The FDP and the flexor pollicis longus (FPL) form the deep compartment of the volar forearm, and they travel through the floor of the carpal tunnel. The FDP tendon passes through the bifurcation of the FDS before inserting into the proximal palmar base of the distal phalanx. The innervation of the FDP of the index and occasionally middle finger, and the FPL, is by the anterior interosseous branch of the median nerve (AIN), whereas the profundus of the ring and little fingers is innervated by the ulnar nerve. The FDP provides digital flexion at both the proximal and DIP joints.
The FDS has two heads: the radial head originates from the proximal shaft of the radius and the humeral ulnar head originates from the medial epicondyle of the humerus and the coronoid process of the ulna. As the FDS tendons pass through the carpal tunnel, the tendons of the middle and ring finger are more superficial and central than those of the index and little fingers. In the proximal aspect of the finger, the FDS tendon bifurcates around the FDP at the beginning of the A2 pulley. The FDS tendon slips then reunites distally at Camper chiasm, with approximately half of the fibers staying on the ipsilateral side and half crossing to the contralateral side of the finger. The tendon then inserts via radial and ulnar slips into the proximal metaphysis of the middle phalanx. The entire FDS muscle is innervated by the median nerve. The primary function of FDS is digital flexion at the PIP joints.
The FPL has two heads: the radial head originates from the proximal radius and interosseous membrane, and an accessory head originates from the coronoid process of the ulna and from the medial epicondyle of the humerus. In the palm, the FPL tendon transverses between the abductor pollicis longus (APL) and the flexor pollicis brevis (FPB). The FPL inserts into the proximal base of the distal phalanx and is innervated by the AIN. The FPL flexes both the interphalangeal and MCP joints of the thumb.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree