Injuries About The Ankle
ROTATIONAL ANKLE FRACTURES
Epidemiology
Population-based studies suggest that the incidence of ankle fractures has increased dramatically since the early 1960s.
The highest incidence of ankle fractures occurs in elderly women, although fractures of the ankle are generally not considered to be “fragility” fractures.
Most ankle fractures are isolated malleolar fractures, accounting for twothirds of fractures, with bimalleolar fractures occurring in one-fourth of patients and trimalleolar fractures occurring in the remaining 5% to 10%.
The incidence of ankle fractures is approximately 187 fractures per 100,000 people each year.
Open fractures are rare, accounting for just 2% of all ankle fractures.
Increased body mass index is considered a risk factor for sustaining an ankle fracture.
Anatomy
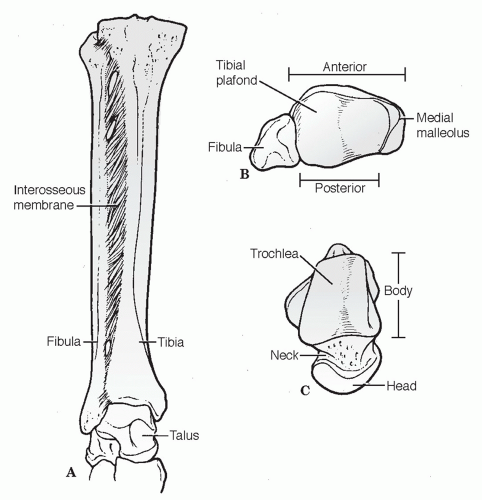
The ankle is a complex hinge joint composed of articulations among the fibula, tibia, and talus in close association with a complex ligamentous system (Fig. 38.1).
The distal tibial articular surface is referred to as the “plafond,” which, together with the medial and lateral malleoli, forms the mortise, a constrained articulation with the talar dome.
The plafond is concave in the anteroposterior (AP) plane but convex in the lateral plane. It is wider anteriorly to allow for congruency with the wedge-shaped talus. This provides for intrinsic stability, especially in weight bearing.
The talar dome is trapezoidal, with the anterior aspect 2.5 mm wider than the posterior talus. The body of the talus is almost entirely covered by articular cartilage.
The medial malleolus articulates with the medial facet of the talus and divides into an anterior colliculus and a posterior colliculus, which serve as attachments for the superficial and deep deltoid ligaments, respectively.
The lateral malleolus represents the distal aspect of the fibula and provides lateral support to the ankle. No articular surface exists between the distal tibia and fibula, although there is some motion between the two. Some intrinsic stability is provided between the distal tibia and fibula just proximal to the ankle where the fibula sits between a broad anterior tubercle and a smaller posterior tubercle of the tibia. The distal fibula has articular cartilage on its medial aspect
extending from the level of the plafond distally to a point halfway down its remaining length.
The syndesmotic ligament complex exists between the distal tibia and fibula, resisting axial, rotational, and translational forces to maintain the structural integrity of the mortise. It is composed of four ligaments, including:
Anterior inferior tibiofibular ligament
Posterior inferior tibiofibular ligament (PITFL). This is thicker and stronger than the anterior counterpart. Therefore, torsional or translational forces that rupture the anterior tibiofibular ligament may cause an avulsion fracture of the posterior tibial tubercle, leaving the posterior tibiofibular ligament intact.
Inferior transverse tibiofibular ligament (inferior to posterior tibiofibular)
Interosseous ligament (distal continuation of the interosseous membrane) (Fig. 38.2)
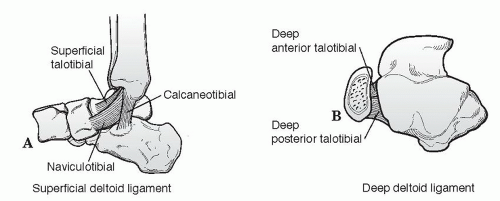
The deltoid ligament provides ligamentous support to the medial aspect of the ankle. It is separated into superficial and deep components (Fig. 38.3).
Superficial portion: This is composed of three ligaments that originate on the anterior colliculus but add little to ankle stability.
Naviculotibial ligament: This suspends the spring ligament and prevents inward displacement of the talar head.
Tibiocalcaneal ligament: This prevents valgus displacement. Superficial tibiotalar ligament.
Talotibial Ligament: This is the most prominent of the three.
Deep portion: This intra-articular ligament (deep tibiotalar) originates on the intercollicular groove and the posterior colliculus of the distal tibia and inserts on the entire nonarticular medial surface of the talus. Its fibers are transversely oriented; it is the primary medial stabilizer against lateral displacement of the talus.
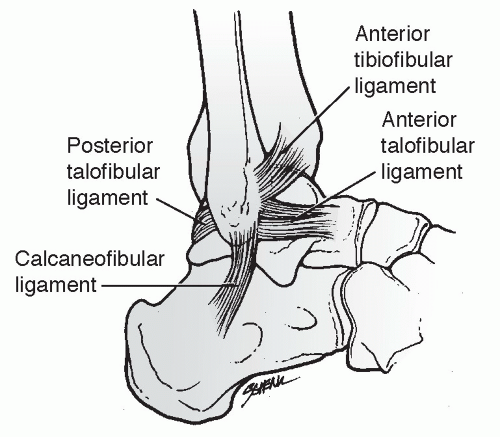
The fibular collateral ligament is made up of three ligaments that, together with the distal fibula, provide lateral support to the ankle. The lateral ligamentous complex is not as strong as the medial complex (Fig. 38.4).
Anterior talofibular ligament: This is the weakest of the lateral ligaments; it prevents anterior subluxation of the talus primarily in plantar flexion.
Posterior talofibular ligament: This is the strongest of the lateral ligaments; it prevents posterior and rotatory subluxation of the talus.
Calcaneofibular ligament: This is lax in neutral dorsiflexion owing to relative valgus orientation of calcaneus; it stabilizes the subtalar joint and limits inversion; rupture of this ligament will cause a positive talar tilt test.
Biomechanics
The normal range of motion (ROM) of the ankle in dorsiflexion is 30 degrees, and in plantar flexion it is 45 degrees; motion analysis studies reveal that a minimum of 10 degrees of dorsiflexion and 20 degrees of plantar flexion are required for normal gait.
The axis of flexion of the ankle runs between the distal aspect of the two malleoli, which is externally rotated 20 degrees compared with the knee axis.
A lateral talar shift of 1 mm will decrease surface contact by 40%; a 3-mm shift results in >60% decrease.
Mechanism of Injury
The pattern of ankle injury depends on many factors, including mechanism (axial vs. rotational loading); chronicity (recurrent ankle instability
may result in chronic ligamentous laxity and distorted ankle biomechanics); patient age; bone quality; position of the foot at time of injury; and the magnitude, direction, and rate of loading. Specific mechanisms and injuries are discussed in the section on classification.
may result in chronic ligamentous laxity and distorted ankle biomechanics); patient age; bone quality; position of the foot at time of injury; and the magnitude, direction, and rate of loading. Specific mechanisms and injuries are discussed in the section on classification.
Clinical Evaluation
Patients may have a variable presentation, ranging from a limp to nonambulatory in significant pain and discomfort, with swelling, tenderness, and variable deformity.
Neurovascular status should be carefully documented and compared with the contralateral side.
The extent of soft tissue injury should be evaluated, with particular attention to possible open injuries and blistering. The quality of surrounding tissues should also be noted.
The entire length of the fibula should be palpated for tenderness because associated fibular fractures may be found proximally as high as the proximal tibiofibular articulation. A “squeeze test” may be performed approximately 5 cm proximal to the intermalleolar axis to assess possible syndesmotic injury
A dislocated ankle should be reduced and splinted immediately (before radiographs if clinically evident) to prevent pressure or impaction injuries to the talar dome and to preserve neurovascular integrity.
Radiographic Evaluation
AP, lateral, and mortise views of the ankle should be obtained.
AP view
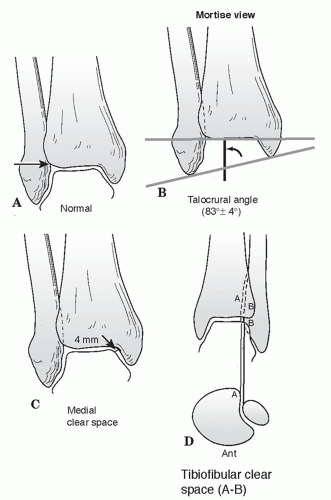
Tibiofibula overlap of <10 mm is abnormal and implies syndesmotic injury.
Tibiofibula clear space of >5 mm is abnormal and implies syndesmotic injury.
Talar tilt: A difference in width of the medial and lateral aspects of the superior joint space of >2 mm is abnormal and indicates medial or lateral disruption.
Lateral view
The dome of the talus should be centered under the tibia and congruous with the tibial plafond.
Posterior tibial tuberosity fractures can be identified, as well as direction of fibular injury.
Avulsion fractures of the talus by the anterior capsule may be identified.
Anterior or posterior translation of the fibula in relation to the tibia in comparison to the opposite uninjured side is indicative of a syndesmotic injury.
Mortise view (Fig. 38.5)
This is taken with the foot in 15 to 20 degrees of internal rotation to offset the intermalleolar axis.
A medial clear space >4 to 5 mm is abnormal and indicates lateral talar shift.
Talocrural angle: The angle subtended between the intermalleolar line and a line parallel to the distal tibial articular surface should be between 8 and 15 degrees. The angle should be within 2 to 3 degrees of the uninjured ankle.
Tibiofibular overlap <1 cm indicates syndesmotic disruption.
Talar shift >1 mm is abnormal.
A physician-assisted stress view with the ankle dorsiflexed and the foot stressed in external rotation can be used to identify medial injury with an isolated fibula fracture. A gravity stress view is an alternative with similar sensitivity.
Computed tomography (CT) scans help to delineate bony anatomy, especially in patients with plafond injuries.
Magnetic resonance imaging (MRI) may be used for assessing occult cartilaginous, ligamentous, or tendinous injuries.
Classification
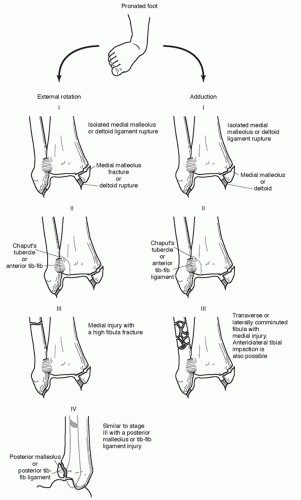
Lauge-Hansen (Rotational Ankle Fractures)
Four patterns are recognized, based on “pure” injury sequences, each subdivided into stages of increasing severity (Figs. 38.6 and 38.7).
This system is based on cadaveric studies.
Patterns may not always reflect clinical reality
The system takes into account (1) the position of the foot at the time of injury and (2) the direction of the deforming force.
Supination-Adduction (SA)
This accounts for 10% to 20% of malleolar fractures.
This is the only type associated with medial displacement of the talus.
Stage I: Produces either a transverse avulsion-type fracture of the fibula distal to the level of the joint or a rupture of the lateral collateral ligaments
Stage II: Results in a vertical medial malleolus fracture
Supination-External Rotation (SER)
This accounts for 40% to 75% of malleolar fractures.
Stage I: Produces disruption of the anterior tibiofibular ligament with or without an associated avulsion fracture at its tibial or fibular attachment
Stage II: Results in the typical spiral fracture of the distal fibula, which runs from anteroinferior to posterosuperior
Stage III: Produces either a disruption of the posterior tibiofibular ligament or a fracture of the posterior malleolus
Stage IV: Produces either a transverse avulsion-type fracture of the medial malleolus or a rupture of the deltoid ligament
Pronation-Abduction (PA)
This accounts for 5% to 20% of malleolar fractures.
Stage I: Results in either a transverse fracture of the medial malleolus or a rupture of the deltoid ligament
Stage II: Produces either a rupture of the syndesmotic ligaments or an avulsion fracture at their insertion sites
Stage III: Produces a transverse or short oblique fracture of the distal fibula at or above the level of the syndesmosis; this results from a bending force that causes medial tension and lateral compression of the fibula, producing lateral comminution or a butterfly fragment
Pronation-External Rotation (PER)
This accounts for 5% to 20% of malleolus fractures.
Stage I: Produces either a transverse fracture of the medial malleolus or a rupture of the deltoid ligament
Stage II: Results in disruption of the anterior tibiofibular ligament with or without avulsion fracture at its insertion sites
Stage III: Results in a spiral fracture of the distal fibula at or above the level of the syndesmosis running from anterosuperior to posteroinferior
Stage IV: Produces either a rupture of the posterior tibiofibular ligament or an avulsion fracture of the posterolateral tibia
Danis-Weber
This is based on the level of the fibular fracture: the more proximal, the greater the risk of syndesmotic disruption and associated instability. Three types of fractures are described (Fig. 38.8):
Type A: This involves a fracture of the fibula below the level of the tibial plafond, an avulsion injury that results from supination of the foot and that may be associated with an oblique or vertical fracture of the medial malleolus. This is equivalent to the Lauge-Hansen supination-adduction injury.
Type B: This oblique or spiral fracture of the fibula is caused by external rotation occurring at or near the level of the syndesmosis; 50% have an associated disruption of the anterior syndesmotic ligament, whereas the posterior syndesmotic ligament remains intact and attached to the distal fibular fragment. There may be an associated injury to the medial structures or the posterior malleolus. This is equivalent to the Lauge-Hansen supination-external rotation injury.
Type C: This involves a fracture of the fibula above the level of the syndesmosis causing disruption of the syndesmosis almost always with associated medial injury. This category includes
Maisonneuve-type injuries and corresponds to Lauge-Hansen pronation-external rotation or pronation-abduction stage III injuries.
Maisonneuve-type injuries and corresponds to Lauge-Hansen pronation-external rotation or pronation-abduction stage III injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree