CHAPTER 73 Injection Procedures
INTRODUCTION
Perhaps because of a reduced potential for injury, the prevalence of painful disorders of the thoracic spine is significantly less than disorders of the cervical and lumbar spine. Protection against injury may be due to increased stability afforded by the rib cage1,2 and the steep orientation of the spinous processes that limits excessive extension. Stolker at al.3 reported a 5:2:20 ratio of cervical:thoracic:lumbar complaints of spinal pain in a series of patients seen at a pain clinic. Similarly, Occhipinti et al.4 surveyed factory workers and found a prevalence of thoracic spine symptoms of 5% compared to 24% for cervical and 33% for lumbar. In addition, Linton et al.5 reported the prevalence of spinal pain in Sweden in 35–45-year-olds to be 66.3% and found a 56% incidence of low back pain, a 44% incidence of neck pain, and a 15% incidence of upper back pain.
Bogduk6 logically postulated that for any structure to be a cause of back pain it should have a nerve supply, for without access to the nervous system it could not evoke pain. The structure should be capable of causing pain similar to that seen clinically. Ideally, this should be demonstrated in normal volunteers, for inferences drawn from clinical studies may be compromised by observer bias or poor patient reliability. Further, the structure should be susceptible to diseases or injuries that are known to be painful and should have been shown to be a source of pain in patients using diagnostic techniques of known reliability and validity.
The potential sources of thoracic pain therefore include intervertebral discs, zygapophyseal joints, costotransverse and costovertebral joints, dura mater, nerve roots, ligaments, and muscles. However, referred pain from visceral sources such as lung, pleura, heart, aorta, gallbladder, esophagus, and mediastinal pathology must not be missed.7,8
THORACIC ZYGAPOPHYSEAL JOINT PAIN
Although the thoracic zygapophyseal joint pain is under-reported, the cervical zygapophyseal joints have been extensively studied9–12 and are considered a common cause of spinal pain. There are, however, a few thoracic studies. Manchikanti et al. performed controlled comparative local anesthetic blocks of thoracic medial branches in 46 patients to determine the prevalence of zygapophyseal joint pain.13 Inclusion criteria required failure of conservative management with physical therapy, chiropractic management with physical therapy, absence of radicular pattern of pain, absence of disc herniation, and duration of pain for more than 6 months. Forty-eight percent of patients had positive response to double blocks. Interestingly, a false-positive rate of 58% was seen with single blocks.
Anatomical considerations
Nerve fibers converge into medial branch of the primary posterior ramus and relay in dorsal root ganglion prior to entering the spinal cord. Because intersegmental connections in the thoracic spine are not as pronounced as in its cervical and lumbar counterparts, the pain arising in any particular segment of the thoracic spine is more precisely localized than comparable segmental lesions in upper or lower regions of the vertebral column.14
Encapsulated mechanoreceptors and nociceptors in joint capsules of thoracic and lumbar spine have been demonstrated histologically15 and immunohistochemically.16 These mechanoreceptors respond to different states of excursion, provide proprioceptive sense, modulate protective muscular reflexes, and via nociception signal potential tissue damage in the event excessive force is applied. Consistent with neck mobility, need to position the head accurately in space, and the need for coordinated muscle control for protection and posture the cervical spine has more mechanoreceptors than the thoracic spine.
In the experimental study of healthy subjects pain was provoked in 72.5% of 40 tested thoracic T3–4 to T10–11 zygapophyseal joints when injected contrast medium distended the joint capsule.17 Referral pain patterns, although overlapping between segmental levels, were more localized compared to patterns obtained by stimulation of lumbar and cervical joints. The most intense pain was reported one segment below and lateral to the injected joint (Fig. 73.1). Precise borders could not be delineated. The largest inferior referral was 2.5 segments while lateral referral did not cross the posterior axillary line. Two subjects reported interesting referral patterns. In one case the T3–4 injection produced pain in the back and subject also stated that ‘pain went into my lung behind my sternum.’ In another case the T3–4 injection produced pain in the back and the subject also reported that pain ‘like a quarter-sized cylinder went toward my breast bone.’
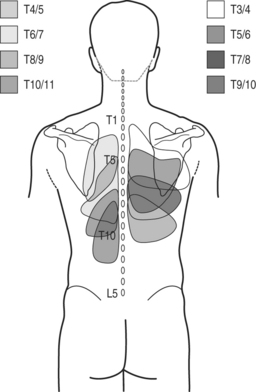
Fig. 73.1 Referral pain patterns from stimulation of zygapophyseal joints T3–4 to T10–11.
(Adapted from Dreyfuss et al. Thoracic zygapophyseal joint patterns: a study of normal volunteers. Spine 1994; 19(7):807–811)
Referral pain patterns from stimulation of zygapophyseal joints C7–T1 through T2–3 and T11–12 were described by Fukui et al. in 1997 (Fig. 73.2).18 A total of 21 joints were injected in 15 patients with previously documented zygapophyseal joint pain. At C7–T1 all patients described pain in paravertebral region extending towards the superior angle of scapula, into interscapular region, and to the inferior angle of scapula. Lateral extension toward the shoulder and suprascapular region was described by two patients. T1–2 stimulation referred into interscapular region and to the inferior angle of the scapula. In two subjects referral was reported into the superior angle of the scapula and suprascapular region. Stimulation at T2–3 joint provoked pain laterally toward the interscapular area and caudally toward the inferior angle of the scapula. T11–12 joint injection referred pain into localized area around the injection and one patient described pain over iliac crest. The authors conclude that referral maps from stimulation of joints at levels of C7–T1 to T2–3 provided such a large overlap that their clinical usefulness in tracking the origin of pain is limited. Anatomical dissection confirming the C7 and C8 medial branches traveling to T2 and T3 level17 may explain this observation.
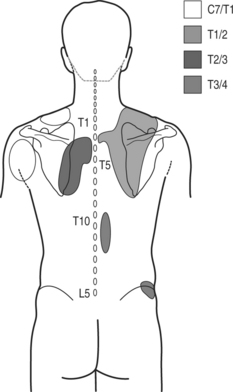
Fig. 73.2 Referral pain patterns from stimulation of zygapophyseal joints C7–T1 through T2–3 and T11–12.
(Adapted from Fukui et al. Regional Anesthesia 1997; 22(4):332–336)
Although lumbar facet denervation was introduced in 1974,19 the procedure was not properly performed until Bogduk20 described the anatomical course of the lumbar medial branches in 1979.
Percutaneous facet denervation was reported in thoracic Z-joints,3 but the study offered no data on the detailed surgical anatomy of the thoracic medial branches. The targeted points for the thoracic medial branches were at a location that was analogous to the position of the lumbar medial branches proposed previously20 at the junction between the superior articular process and the transverse process. In 1994, Stolker et al. published the data from the anatomical study of two thoracic cadaveric spines, where the cannula was placed under fluoroscopic guidance into a target point at the junction of the base of the superior articular process and the transverse process.21 The specimens were then frozen and sectioned with the heavy-duty cryomicrotome. It was observed that although the cannulas were placed reproducibly onto the osseous targets, the medial branch ‘stem’ was never found within the reach of the electrodes. The authors concluded that if the medial branch ‘stem’ is supposed to be the target, a more anterior, more cranial, and more lateral position would perhaps be more effective.
In contrast to the course of the lumbar medial branches, which are at the junction of superior articular process and the transverse process, the medial branch of the thoracic dorsal ramus has a different anatomical location (Figs 73.3, 73.4). Cadaveric dissection of 84 medial branches by Chua and Bogduk revealed the thoracic medial branch arose from the dorsal ramus typically 5 mm lateral to the intervertebral foramen, traversed laterally, dorsally, and inferiorly, and remained posterior to the superior costotransverse ligament.22 After leaving the intertransverse space the medial branch crossed the superolateral corner of the transverse process below (e.g. T3 medial branch and T4 transverse process) and then passed medially and inferiorly across the posterior surface of the transverse process. In its course over the dorsal aspect of the transverse process the nerve was sandwiched between the multifidus muscle anteriorly and the semispinalis thoracis posteriorly. This was the typical course at the levels of T1–4 and T9–10. The T11 medial branch crossed the lateral aspect of base of the superior articular process of T12 vertebra, the transverse process of which is much shorter that other transverse processes. The T12 medial branch had an analogous course to that of the lumbar medial branches at the junction of superior articular and the transverse process of L1. At midthoracic levels (T5–8) the medial branch did not always assume contact with the transverse process and often demonstrated cephalad displacement. The nerve, after making a turn medially in the intertransverse space, descended only slightly inferiorly and remained separated from the transverse process by the fascicles of multifidus muscle.22
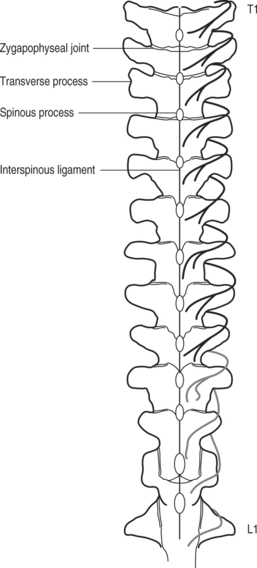
Fig. 73.3 Anatomical location of thoracic medial branches.
(Adapted from Chua and Bogduk. Acta Neurochir 1995; 136:140–144)
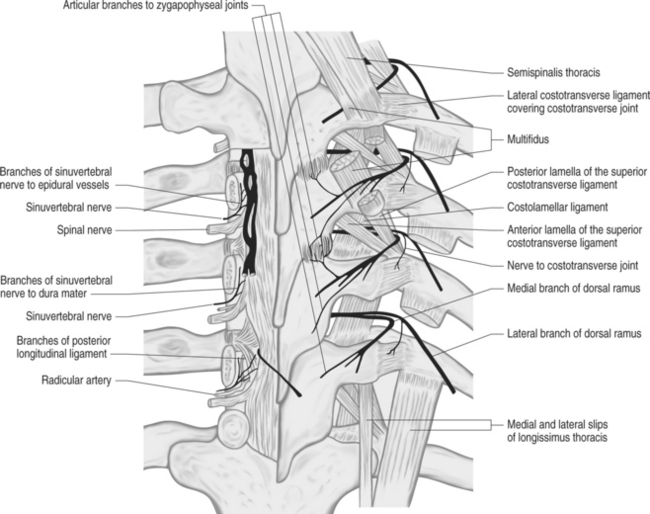
Fig. 73.4 Nerve supply of thoracic spine structures.
From Bogduk N. Innervation and pain patterns of the thoracic spine. In: Grant R, ed. Physical therapy of the cervical and thoracic spine, 3rd edn. New York: Churchill Livingstone; 2002:73–81)
Two articular branches were noted to arise from the medial branches. A short ascending branch separated from the medial branch inferior to the Z-joint and innervated the inferior capsule of the joint. A descending articular branch arose from the medial branch at the superolateral border of the transverse process and in its sinuous course through the multifidus muscle reached and innervated the superior capsule of the joint below.22
The medial branches in upper thoracic segments are musculocutaneous, while lower have only muscular distribution.7
Based on these data, the appropriate target for thoracic medial branch block at T1–3 and T9–10 levels is the superolateral corner of the transverse process where the nerve lies against the osseous structure. For radiofrequency denervation the probe, upon contacting the superolateral corner, should be passed over the edge of the transverse process to be in the contact with the medial branch. Targeting of midthoracic medial branches, due to their different positions, would be more challenging and less reliable. T11 and T12 medial branches are blocked in the same fashion as their lumbar counterparts (junction of the transverse process and the superior articular process). Interestingly, multiple interventional textbooks that have recently been published still describe the techniques of thoracic medial branch blocks and denervation not consistent with current knowledge of anatomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








