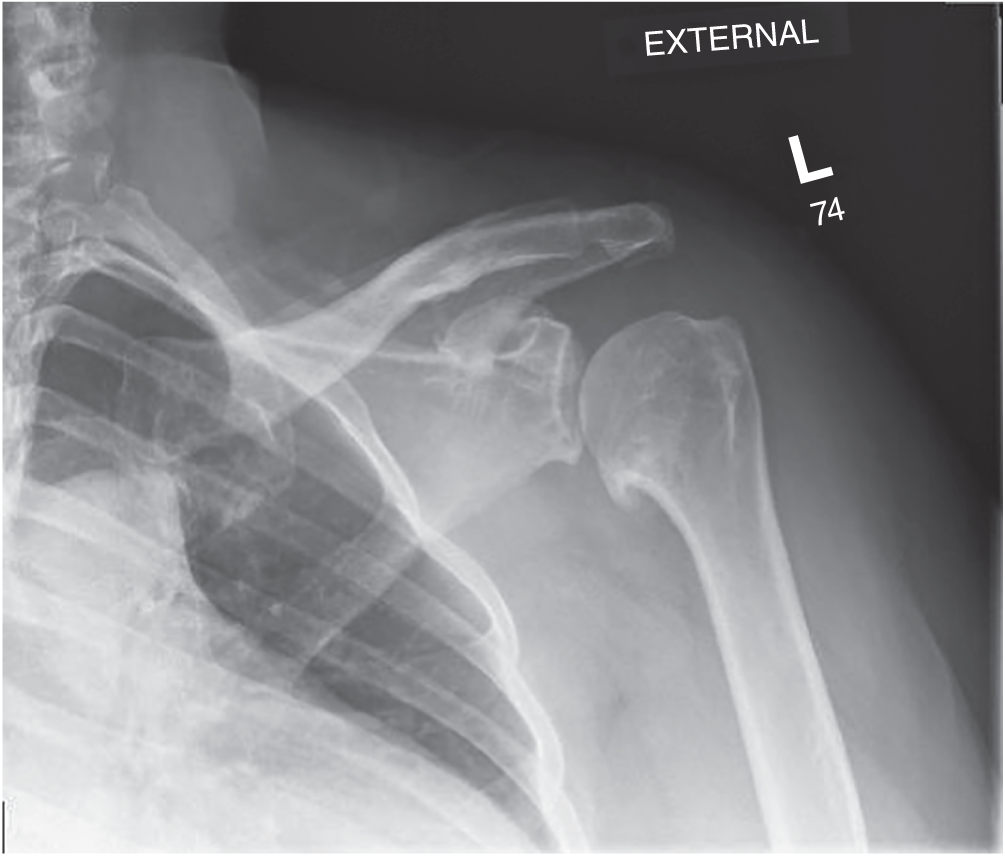
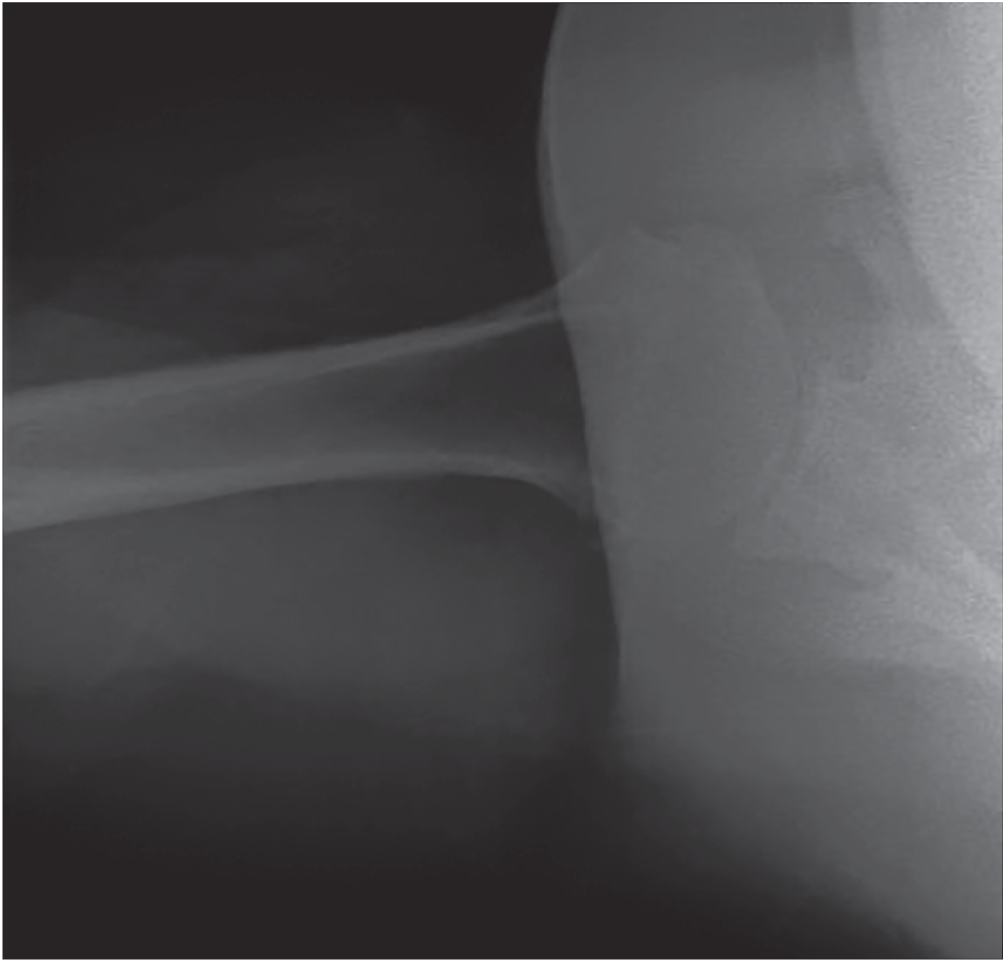
Chad Myeroff MD1, Michael Knudsen MD2, and Michael D. McKee MD FRCS(C)3 1University of Minnesota Department of Orthopaedic Surgery, Regions Hospital and TRIA Orthopedic Center, St. Paul, MN, USA 2Department of Orthopaedic Surgery, University of Minnesota, Minneapolis, MN, USA 3Department of Orthopaedic Surgery, University of Arizona College of Medicine, Phoenix, AZ, USA Several options are currently available for shoulder reconstruction, each with unique indications, benefits, risks, and functional outcomes that must be considered. Personal training biases, local trends, and isolated reviews of the literature can be persuasive in clinical decision‐making. When deciding on the ideal reconstructive option, it is important to have an unbiased and complete view of the literature. This question is best answered with a systematic review of level III and IV studies. This is a 70‐year‐old active individual with end‐stage osteoarthritis and a Walch type A1 glenoid. Walch type A glenoids are centered, with or without central deformity. Walch type B glenoids are posteriorly eroded with or without deformity, and Walch type C glenoids are considered dysplastic.1 The later varieties are more likely to undergo progressive deformity, subluxation, and pose biomechanical challenges that are potentially time sensitive.2,3 Since this glenoid is concentrically worn, there is less concern for progression and continued injection treatment can be considered (Figure 60.1 and 60.2). If conservative treatment fails, hemiarthroplasty or anatomic TSA are common reconstructive options. Both of these options require an intact rotator cuff for ideal function, to avoid anterosuperior escape and early glenoid failure from eccentric loading.4 Fortunately, full thickness rotator cuff tears are only present in 7.6% of patients presenting with primary osteoarthritis, and partial thickness tears have not been shown to influence outcome.5 This patient has a centered head without radiographic signs of cuff tear arthropathy,6 but advanced three‐dimensional imaging may be obtained when there is clinical concern. A full thickness irreparable supraspinatus tear, or any infraspinatus or subscapularis tear, would be a contraindication to primary TSA. Figure 60.1 True AP radiograph of the left shoulder shows joint space collapse, subchondral sclerosis, inferior humeral osteophytes and medialization of the humerus without signs of rotator cuff insufficiency. Source: Chad Myeroff, Michael Knudsen, Michael D. McKee. Figure 60.2 Axillary radiograph of the left shoulder showing concentric glenohumeral joint space loss without subluxation of the humeral head or any eccentric ware. Source: Chad Myeroff, Michael Knudsen, Michael D. McKee. Hemiarthroplasty offers the benefits of preserving glenoid bone stock, less operative time, and less blood loss, and eliminates the risk of glenoid implant failure when compared with TSA. However, hemiarthroplasty carries the inherent risk of progressive glenoid arthritis and pain. While the results have been variable, some authors report success, especially in young active laborers with intractable pain, especially those with a high degree of posterior wear and subluxation where glenoid components would have a higher risk of failure.7–9 In TSA, resurfacing of the glenoid theoretically decreases long‐term pain and restores physiological tension on the rotator cuff, with the traded risk of glenoid implant failure necessitating later revision surgery. A randomized controlled trial (RCT) of 42 arthritic shoulders comparing hemiarthroplasty to TSA showed a trend toward improved disease specific quality of life for TSA as measured by the previously validated Western Ontario Osteoarthritis of the Shoulder (WOOS) score,10 (WOOS 90.6 for TSA vs 81.5 for hemiarthroplasty; p = 0.18) but was underpowered to show a difference.11 Radnay et al. published a systematic review of 23 studies (1952 patients) with an average level of evidence of 3.72 with a mean 43.4 months’ follow‐up.12 TSA provided significantly greater pain relief (86 vs 78; p <0.0001), forward elevation (p <0.0001), external rotation (p = 0.0002), patient satisfaction (97% vs 80%; p <0.0001), and lower revision rate (10.7% hemiarthroplasty vs 1.7% for TSA with all polyethylene cemented glenoids; p <0.025). Of the included hemiarthroplasties, 10.2% required revisions, 79.4% of which (8.1% of all hemiarthroplasties) were converted to TSA for pain.12 Economically, TSA is more cost‐effective. Mather et al. created a Markov decision model using available literature to compare cost utility and reported that a TSA is $1970 cheaper per patient than hemiarthroplasty and provides more quality‐adjusted life years (QALYs).13 Hemiarthroplasty would not be preferred unless the TSA annual revision rate reached 8.52% or $50 000 in initial cost.13 In 2011, the American Academy of Orthopaedic Surgeons (AAOS) concluded there was moderate evidence to recommend TSA over hemiarthroplasty in the surgical management of glenohumeral osteoarthritis. Metal‐backed (MB) glenoid components were introduced to theoretically offer a better mechanical interface, allow surgical correction of complex glenoid deformity, and allow modularity between TSA and reverse total shoulder arthroplasty (RTSA). All‐polyethylene (AP) glenoids have two traditional fixation options: in‐line pegged components are relatively bone preserving, while keeled implants may be technically easier in difficult exposures and lower the risk of vault perforation in smaller glenoids. The glenoid component is the most technically demanding aspect of TSA and is the most likely reason for mechanical failure postoperatively, necessitating meticulous technique and thoughtful implant choice. The vast majority of technical principles have come from level III and IV studies. There are several RCTs comparing glenoid resurfacing options, supported prevalently with level III and IV retrospective studies and biomechanical research. Glenoid reconstruction remains the weak link in TSA with a 0.8% risk of glenoid revision per year and is the most common underlying reason for humeral sided revision as well.14–16 It has been shown that restoring close to normal version (to <10–15° retroversion) lowers radiographic osteolysis and cement mantle shear forces.17,18 Conservative reaming should maintain the subchondral plate to minimize failure.19 It is recommended that glenoid surface and humeral head have a 4° radius of curvature mismatch to avoid edge loading and best restore anatomic translation and motion.20 Although anatomic glenoid reconstruction has an overall 95% 10‐year survivorship on the aggregate, there is variability in implants. Clinical results for MB glenoid components have shown increased failure and revision rates. In Radnay et al.’s systematic review of 1952 patients, they found a higher risk for revision for MB implants (6.8% MB vs 1.7% AP).12 Cil et al. showed higher humeral sided 10‐year revision‐free survival with AP glenoids in a systematic review of 1584 implants (96.5% vs 86.8%).15 Fox et al. reviewed 1542 TSAs and found that revision‐free survival was superior for AP glenoids (p <0.01).21 Clitherow et al. performed a registry study of 1056 AP glenoid implants versus 540 MB glenoid implants placed in New Zealand. They found a 4.4‐fold higher risk for revision in MB (1.92% vs 0.44%; p <0.001).22 Boileau et al. published an RCT on 39 patients comparing AP pegged glenoid design to MB glenoid design with 36 months’ follow‐op and found higher radiolucent lines for AP component (85% vs 25%; p <0.01);23 however, the majority of AP radiolucencies were nonprogressive and there was no correlation with functional outcome (p = 0.3). Radiolucent lines are rare with MB implants but progressive and sinister when present (clinical loosening/failure: 20% MB vs 0% AP; p <0.001). Additionally, these authors found that MB glenoid implants correlated significantly with decreased functional results and increased pain (p <0.05).23 The same authors published long‐term outcomes of 165 MB glenoids and reported only 46% revision free survival at 12 years.24
60
Implant Design Options in the Treatment of Shoulder Osteoarthritis
Clinical scenario
Top three questions
Question 1: In this patient with end‐stage shoulder osteoarthritis, what is the ideal surgical treatment?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
Resolution of clinical scenario
Question 2: If an anatomic total shoulder arthroplasty (TSA) is elected, what is the ideal glenoid component design?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





